Acute Lymphoblastic Leukaemia (ALL)
Acute lymphoblastic leukaemia is a cancer of the white blood cells. The white blood cells are cells in the bone marrow and blood stream that protect people against infections and provide immunity to the body. The white blood cells are made up of many different types of cells, namely neutrophils, lymphocytes, basophils and monocytes. Each of these cells again are at different stages of maturation and are called different names. Early lymphocytes are known as lymphoblasts and this cancer is when there is excessive uncontrolled production of lymphoblasts.
ALL is primarily a cancer in children in the age group of 1-4 years, but it is also seen in older children and young adult patients.
Unlike chronic leukaemia which develops slowly, ALL grows in a patient quickly over days or weeks.
All blood cells are made in the bone marrow, which is the soft spongy area in the centre of the bone. ALL cells increase in the marrow and spread into the blood stream and other parts of the body such as the lymph nodes, liver, spleen, nervous system and testes. While the cancer increases and occupies most of the space in the bone marrow, it prevents the production of other blood cells in the body such as other white blood cells, platelets, red blood cells etc. This leads to the symptoms produced by the cancer.
The risk factors associated in the development of acute lymphoid leukaemia are listed below.
Genetic conditions
People associated with the following genetic conditions have an increased risk of developing leukaemia.
- Down’s syndrome
- Li-Fraumeni syndrome
- Bloom syndrome
- Ataxia Telangiectasia
- Neurofibromatosis type 1
Radiation
People exposed to high levels of radiation in the past have a risk of developing acute leukaemia. The risk is higher for acute myeloid leukaemia than acute lymphoblastic leukaemia. Previous radiotherapy for other cancer or condition carries a risk for developing a leukaemia.
Previous chemotherapy
Children who had previous chemotherapy are at increased risk of leukaemia some years after treatment. This risk is more for acute myeloid leukaemia than ALL.
Sibling with leukaemia
Children with a brother or a sister who had leukaemia have a higher risk of getting it as compared to others with no such history.
Others
Exposure to certain pesticides, cigarette smoke or alcohol is a risk factor for childhood leukaemia. This exposure could be to the child or to the mother while pregnant.
Acute lymphoblastic leukaemia (ALL) can be broadly divided into three main subtypes. They are
- B Cell ALL
- T Cell ALL
- Philadelphia chromosome positive ALL
Philadelphia chromosome positive ALL
The B cell ALL is the commonest of them. Philadelphia chromosome positive ALL is also a type of B cell ALL that is more common in adults and is uncommon in children.
Phases of Acute Lymphoblastic Leukaemia (ALL)
The ALL that is present in the patient can be placed in different phases depending on the amount of disease present in the body and its response to treatment. These are briefly listed below.
Untreated disease
This is the phase of disease at the time of diagnosis when treatment has not been started yet. In this phase, the blood counts such as red blood cells, platelets and normal white blood cells may be low in number or normal. The blast cells that make up ALL are increased in number and make up more than 25% of the bone marrow cells. As explained before, blast cells are an early form of normal lymphocytes in the marrow and these are the cancer cells in ALL.
Disease in remission
Remission occurs after the patient has had treatment for the disease. Remission can be complete or partial.
Complete remission is when there are less than 5% of blast cells in the bone marrow. This is found out on bone marrow examination after treatment. The blood cell counts of other cells are normal and there is no disease in the brain or other parts of the nervous system. This is assessed by a lumbar puncture and sampling of the spinal fluid (CSF).
Partial remission is one where there are less than 25% of blast cells in the bone marrow.
Minimal residual disease (MRD)
If after completion of treatment, there is no evidence of disease (blast cells) on bone marrow examination but blast cells are seen on more sensitive tests such as PCR or flow cytometry, the patient is said to have MRD.
Recurrent or relapsed disease
This phase is when the patient was in remission before, but now the number of blast cells in the bone marrow have increased to more than 5%.
Refractory disease
This is when the leukaemia does not go into remission after treatment which implies that the given treatment has not worked as well as expected.
ALL can produce a variety of symptoms due to its effect on the bone marrow, lymph nodes, liver, brain, spinal cord and spleen. Common side effects associated with it are given below. It is important to note that these symptoms can happen due to other reasons and most patients that have these symptoms don not have a leukaemia.
Weakness and Tiredness
This is a common symptom that is present in patients with this condition. It can be due to anaemia as enough red blood cells are not being produced due to this condition. The patient notices tiredness on performing small tasks which they were able to do before.
Breathlessness
Breathlessness is also a symptom of anaemia as there are lesser number of red blood cells to transport oxygen to the tissues. This leads to the patient needing to put more effort in breathing to do the same amount of work.
Repeated Infections
Patients with ALL can have repeated infections due to reduced immunity. This is because of reduced production of normal white blood cells and reduced function of the white blood cells that are produced. The capacity for the body to fight infections will be less and hence patients can experience more infections.
Bleeding and bruising
There can be reduced number of platelets in patients with ALL because of reduced production of them in the bone marrow and also increased destruction of platelets in the body. As platelet function is to help with blood clotting, a reduction of these cells can lead to increased episodes of bleeding. The bleeding can be from anywhere in the body including the gums, nose, while passing motion or urine etc. Bruising may be visible on the skin.
Lymph node enlargement
Lymph nodes are present in all parts of the body including the neck, under the arms, chest, abdomen, pelvis and groins. Enlargement of these lymph nodes can be a symptom of ALL and this leads to swelling in these areas. Enlargement of nodes in the chest can lead to cough and breathlessness.
Swelling and fullness in the Abdomen
Some patients with ALL have enlargement of organs such as liver and spleen. Both these organs are present in the abdomen, and this enlargement leads to distension or a feeling of fullness in the abdomen, aching sensation or breathlessness.
CNS symptoms
In patients with involvement of the nervous system, the symptoms produced can be vomiting, feeling of nausea, visual disturbances, headaches, weakness in the muscles, loss of balance and unsteadiness on the feet.
Other symptoms
Other symptoms that could be present include fever, joint or bone pains, nodules on the skin, painful or swollen testicles.
When ALL is suspected, the following tests are done to aid in diagnosis and decide on treatment options.
Blood tests
Routine blood tests such as a full blood count or complete blood picture will inform about the number of red blood cells, white blood cells and platelets in the blood. It could also indicate the presence of leukaemia cells if present in the blood. Other blood tests include kidney function and liver function tests, bleeding and clotting profile of the blood, Lactate dehydrogenase (LDH) and uric acid.
Tests for Philadelphia chromosome
Genetic testing looking for the translocation protein is done with the help of blood or a bone marrow sample. This is done by FISH or RT-PCR testing. The test shows the abnormal translocation in patients with Philadelphia chromosome positive ALL.
Flow Cytometry
This is a process where blood cells are further characterised based on their physical and chemical properties. A flow cytometer is a machine which analyses the blood sample using a laser. It uses antibodies and fluorescence to locate the cells. The cells are named or separated by the different fluorescence produced by the cells. This is picked up and analysed by a computer. It helps in making a diagnosis of Acute lymphoblastic leukaemia and subtype the different types of ALL. Flow cytometry is a more sensitive test than standard microscopy and is used to diagnose and to detect recurrence of ALL after initial treatment.
Bone Marrow Examination
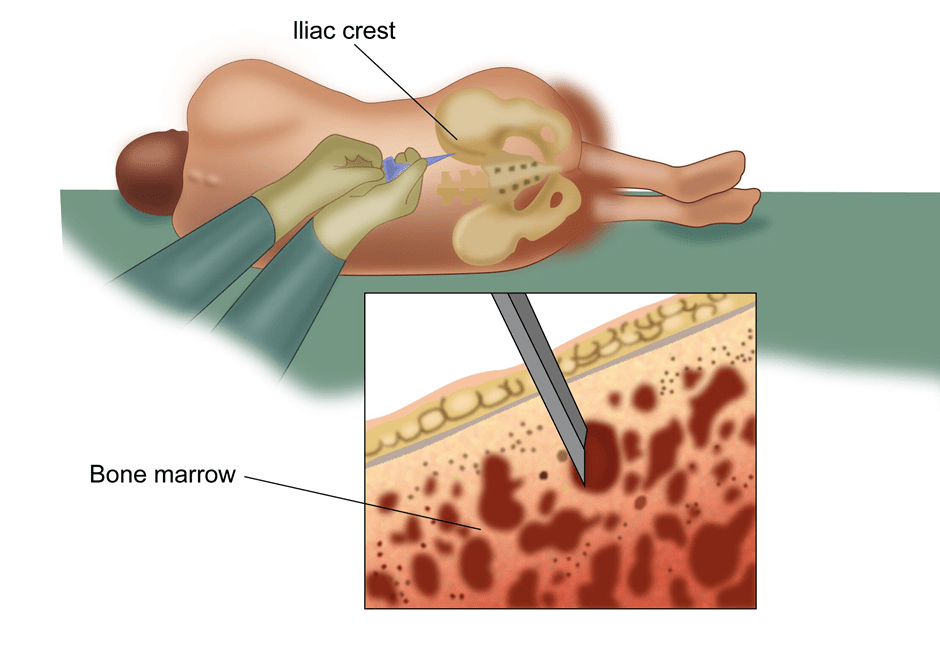
A bone marrow examination involves taking a sample of the marrow from the bone to look for cancer cells (ALL) and other abnormalities in the bone marrow. This test is commonly done in cancers related to the blood and lymphatic system. The marrow is taken from the bones of the pelvis or sternum. A local anaesthetic drug is given to reduce the discomfort prior to the procedure. The test is done on an outpatient basis and the patient can go home after the test is done. Two types of examination are done. One is bone marrow aspiration where a sample of fluid from the marrow is taken and the other is a trephine biopsy where a small piece of the bone is also taken. The report will be available in a few days.
Cytogenetics
Samples from the bone marrow biopsy are also tested for changes in the genetic material in the cells which can help in diagnosis of the subtype of ALL and inform about the possible outcomes of the condition after treatment.
Immunophenotyping and Immunohistochemistry
These tests look at the proteins on the cells using antigen and antibody reactions to exactly find and type the cells of ALL. The antibodies used to detect the antigens on the cells are fluorescent which enables the examiner to see the cells.
FISH and PCR
These are tests used to diagnose leukaemia by looking at the genetic changes by using DNA probes
Lumbar Puncture
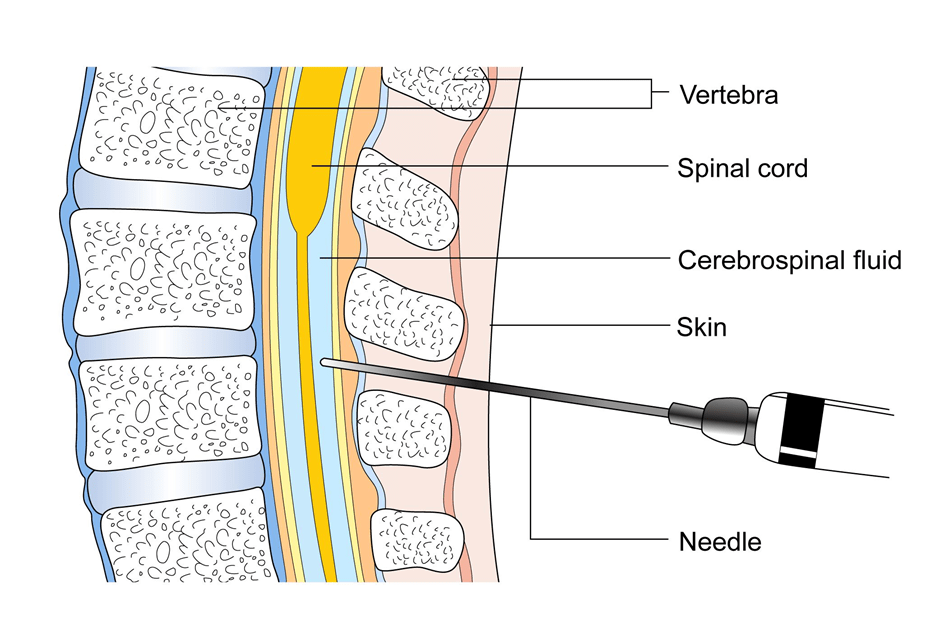
This is a test where is a needle is placed in the spine to take a sample of fluid present in the area surrounding the spinal cord to look for the presence of leukaemia cells. This test is done under local or general anaesthetic depending on the age of the patient.
CT Scan
A CT scan is done in patients with ALL to look for the presence of enlarged lymph nodes or organs such as liver and spleen. The scan will aim to cover the areas of the neck, chest, abdomen and the pelvis.
Acute lymphoblastic leukaemia (ALL) in a child is the most common cancer of childhood, accounting for 30% of all childhood cancers. With improvements in treatments over the last few decades, cure rates for ALL in children can be quite high, usually over 85% in good centres.
Treatment of Acute lymphoblastic leukaemia in children depends on the age of the cancer at diagnosis, the fitness of the patient and the subtype of ALL. Generally, the treatment can be divided into three phases which are induction phase, consolidation phase and maintenance phase. The treatment period lasts 2-3 years in total.
The main type of treatment used in these three phases is chemotherapy, which is use of drugs given through a vein. Chemotherapy is also given into the spine (into the CSF in spinal canal) to prevent relapse or to treat disease that is in the nervous system. Other forms of treatments used include targeted or biological therapy, radiotherapy and stem cell transplant. These are discussed below.
Chemotherapy
Induction Phase
The induction phase of chemotherapy involves the use of a combination of drugs with the aim to achieve a complete remission, wherein there are no residual ALL cells in the blood or bone marrow. Treatment is given as an in -patient basis and patient stays in hospital for some time to be monitored for blood counts and side effects of treatment. Most patients with childhood ALL are Philadelphia chromosome negative (90%). For these patients, the drugs that are commonly used as chemotherapy include
- Vincristine
- Asparaginase
- Steroids- can be Dexamethasone or Prednisolone
- Anthracyclines- can be Doxorubicin or Daunorubicin is added as a fourth drug in some patients.
Many different chemotherapy combinations are used as induction treatment. Chemotherapy is given into the vein and into the spinal fluid to treat any disease that has spread into the nervous system.
Patients who have Philadelphia chromosome positive ALL are treated with chemotherapy and a tyrosine kinase inhibitor such as Imatinib or Dasatinib. These act on specific receptors in patients with Ph+ve disease to help control it. In childhood ALL, about 5% of patients will have a positive Philadelphia chromosome.
Patients who have Down’s syndrome have a higher risk of developing ALL. These patients are treated with chemotherapy that is less intensive than other patients because of a higher risk of side effects in these patients.
Potential side effects of chemotherapy include tiredness, nausea, vomiting, constipation, hair loss, loss of taste and appetite, loose motions, blood clots, allergic reactions, soreness in the mouth, tingling in hands and feet, low blood counts and risk of infection.
In patients who have low blood counts, injections to help improve the white cell count (growth factors), blood or platelet transfusion may be needed. Antibiotics are given for patients with infection after treatment.
For patients who have definite involvement of the central nervous system at diagnosis, intrathecal chemotherapy, where treatment is given into the spinal canal is mostly used as an option of treatment. Radiotherapy to the brain and spinal cord, also known as cranio-spinal radiotherapy is an alternative option to use. When such radiotherapy is used, it is given over 6-12 daily week days.
Consolidation Phase
Consolidation phase involves continuation of combination chemotherapy after completion of induction treatment but with a different set of drugs usually. This treatment is given over many months, about 4-8, and usually includes drugs such as Cytarabine, Mehtotrexate, Etoposide, Cyclofosfamide, Anthracycline drugs, steroids and Imatinib or Dasatinib in patients who are Philadelphia chromosome positive. Treatment into the spine to reduce risk of recurrence in the nervous system is continued with chemotherapy.
Some centres would consider delayed intensification therapy, which is chemotherapy with a combination of drugs similar to those used in the induction phase. This is to get a better response and is considered in high risk patients. As this is more chemotherapy as compared to standard, the patient can have more side effects as well.
Maintenance Phase
Maintenance phase of ALL treatment involves chemotherapy which is less intensive than in the other phases. The purpose of maintenance treatment is to reduce risk of recurrence of ALL. In this phase, chemotherapy drugs that are used include Mercaptopurine which is given daily, Methotrexate which is given weekly, and Vincristine and steroids which are given periodically. In Ph+ve ALL patients, Imatinib or Dasatinib are continued.
Stem Cell Transplant
Stem cell transplant is a type of treatment that may be used in ALL in patients who had a complete remission and have a high risk of relapse of their disease later. Those patients who have a normal risk of relapse may not need a stem cell transplant.
Prior to having a transplant, the patient is given a high dose of chemotherapy, for example a regimen of chemotherapy. The aim of this chemotherapy is to kill off all ALL cells. As this chemotherapy is high dose, it kills off normal cells present in the bone marrow also.
The function of the bone marrow normally is to produce blood cells such as red blood cells which help the blood to carry oxygen, white blood cells which protect against infections and platelets which help stop bleeding. A significant lowering of these cells in the blood is dangerous to the patient and hence a transplant of these cells is needed after a high dose of chemotherapy.
Collection of Stem Cells
Stem cells are a type of blood cells that have the capacity to develop into any kind of blood cell such as red blood, white blood cell or platelets. These stem cells are present in the blood stream and bone marrow and are initially collected from the patient before the patient receives high dose chemotherapy. This process of collection of stem cells from the patient and infusing them back into the same patient after high dose chemotherapy is called as Autologous Stem cell transplant.
If the stem cells are from another person(donor), then it is called an Allogenic stem cell transplant. The donor can be related, usually a brother or a sister. A donor may be used in situations when there is cancer present in the marrow or an autologous transplant was done before, but the disease has relapsed again.
Before collection of stem cells, the patient may have chemotherapy and injections with G-CSF which will increase the number of stem cells in the blood to achieve a successful collection.
On the day of collection of stem cells, the patient is connected to a machine and the patient’s blood is taken out from one vein and it passes through the machine to collect the stem cells present in the blood. The blood then passes back into the patient through another vein. This process is done over a few hours.
Once the stem cells are collected, the patient receives the high dose chemotherapy. After the chemotherapy, the stem cells are infused back into the patient. These cells go into the bone marrow and start making blood cells again.
Risks and side effects of Stem cell Transplant
Having a stem cell transplant is a complex process and is associated with side effects. This procedure usually involves staying in hospital for a few weeks for the blood cells in the marrow and blood to recover to normal levels after the transplant is done. Common side effects associated with this procedure include
Nausea, Vomiting, Hair loss, altered function of the liver are potential side effects of this treatment.
Risk of Infection as white blood cells are low and the patient to prone to get an infection. The infections could be bacterial, viral or fungal and will usually need antibiotics to control them.
Mucositis is the effect of chemotherapy on the inside lining of the mouth and digestive tract. This can limit the amount of food taken by the patient and other methods of feeding may be used in that instance.
Bleeding is a risk associated with this procedure due to low platelet count, but platelet transfusion can be given to keep the platelet counts up.
Graft versus host disease is a reaction of the body to the transfused cells particularly if the stem cells or marrow is from a donor.
Radiotherapy
Radiotherapy is an option of treatment in some patients with ALL. Radiotherapy is given to the brain and spine in patients who have disease confirmed in the nervous system. In such a situation, treatment is given daily, once a day for 6-12 days.
Radiotherapy may also be used as a conditioning treatment prior to a stem cell transplant. Conditioning treatment is one where the treatment is aimed to get rid of all blood cells in the body prior to the transplant of stem cells. This conditioning treatment can be chemotherapy or radiotherapy. When radiotherapy is used, it is given to the whole body and is called as total body irradiation (TBI).
Treatment of relapsed or residual disease
A high proportion of patients in induction and consolidation treatment will go into remission. Some patients will not and will have to be treated with other drugs. A proportion of patients who have had a remission after above may develop a relapse of disease sometime later. Treatment options for these patients include chemotherapy with a different combination of drugs than before, stem cell transplant if they have achieved a partial or complete remission after treatment again or alternative targeted or biological therapy if they have Ph+ve disease. Drugs used in patients with relapsed disease include Nelarabine, Bortezomib, both used in T cell ALL, Blinatumomab (B cell ALL) among other drugs.
Car T Cell Therapy
This is a new form of immunotherapy and one of the types of adoptive cell therapy where the patient’s T lymphocytes (type of white blood cells) are removed from the bloodstream and are reprogrammed to express chimeric antigen receptors (CAR). These modified cells are then increased in number in the lab. These receptors are present on the surface of these T-cells and when injected back into the patient will enable the cells to track and kill ALL cells. This therapy has been found to be very effective and is used to treat B cell ALL in children.
Tisagenlecleucel is one such T cell therapy that is approved for use in patients under 25 years of age with B cell ALL that has come back after initial treatment.
Follow up
As childhood ALL is a disease in childhood and a highly curable disease, it is important that these children are followed up for a long period of time. The treatment regimens that are used are toxic and cause both short and long term side effects. The long term side effects can manifest months to years after completion of treatment. Therefore, regular follow up with the Oncologist as well as other teams is essential to manage these side effects well, so that the patient is able to lead as normal a life as possible.
Treatment of Acute lymphoblastic leukaemia depends on the age of the cancer at diagnosis, the fitness of the patient and the subtype of ALL. Generally, the treatment can be divided into three phases which are induction phase, consolidation phase and maintenance phase.
The main type of treatment used in these three phases is chemotherapy, which is use of drugs given through a vein. Chemotherapy is also given into the spine to prevent relapse or to treat disease that is in the nervous system. Other forms of treatments used include targeted or biological therapy, radiotherapy and stem cell transplant. These are discussed below.
Chemotherapy
Induction Phase
The induction phase of chemotherapy involves the use of a combination of drugs with the aim to achieve a complete remission, wherein there are no residual ALL cells in the blood or bone marrow. Treatment is given as an in -patient basis and patient stays in hospital for some time to be monitored for blood counts and side effects of treatment. Drugs that are commonly used as chemotherapy for induction phase include
- Vincristine
- Anthracyclines- can be Doxorubicin or Daunorubicin or a similar drug
- Steroids- can be Dexamethasone or Prednisolone
- Other drugs such as Cyclofosfamide, Cytarabine, Methotrexate, Asparaginase etc. Many different chemotherapy combinations are used as induction treatment.
Treatment with chemotherapy is given into the vein and into the spinal fluid to treat any disease that has spread into the nervous system.
Patients who have Philadelphia chromosome positive ALL are treated with chemotherapy and a tyrosine kinase inhibitor such as Imatinib or Dasatinib. Imatinib acts on specific receptors in patients with Ph+ve disease to help control it.
Potential side effects of chemotherapy include tiredness, nausea, vomiting, constipation, hair loss, loss of taste and appetite, loose motions, soreness in the mouth, tingling in hands and feet, low blood counts and risk of infection.
In patients who have low blood counts, injections to help improve the white cell count (growth factors), blood or platelet transfusion may be needed. Antibiotics are given for patients with infection after treatment.
For patients who have definite involvement of the central nervous system at diagnosis, radiotherapy to the brain over 12 days as well as chemotherapy into the spinal canal (Intrathecal) is given.
Consolidation Phase
Consolidation phase involves continuation of combination chemotherapy after completion of induction treatment. Most patients have minimal residual disease after induction treatment and therefore consolidation treatment aims to get rid of that disease. This treatment is given over many months and usually includes similar drugs used for the induction treatment such as Vincristine, Anthracycline drugs, steroids and Imatinib or Dasatinib in patients who are Philadelphia chromosome positive. Treatment into the spine to reduce risk of recurrence in the nervous system is continued with chemotherapy. A stem cell transplant may be considered if the patient goes into complete remission.
Maintenance Phase
Maintenance phase of ALL treatment involves chemotherapy which is less intensive than in the other phases. The purpose of maintenance treatment is to reduce risk of recurrence of ALL. It is given for a longer duration lasting up to 2-3 years. In this phase, chemotherapy is given into the vein as well as into the spine as before. The chemo drugs used are commonly Mercaptopurine and Methotrexate. Other drugs such as steroids and Vincristine may also be used. In Ph+ve ALL patients, Imatinib or Dasatinib are continued.
Stem Cell Transplant
Stem cell transplant is a type of treatment that may be used in ALL in patients who had a complete remission and have a high risk of relapse of their disease later. Those patients who have a normal risk of relapse may not need a stem cell transplant.
Prior to having a transplant, the patient is given a high dose of chemotherapy, for example a regimen of chemotherapy. The aim of this chemotherapy is to kill off all ALL cells. As this chemotherapy is high dose, it kills off normal cells present in the bone marrow also.
The function of the bone marrow normally is to produce blood cells such as red blood cells which help the blood to carry oxygen, white blood cells which protect against infections and platelets which help stop bleeding. A significant lowering of these cells in the blood is dangerous to the patient and hence a transplant of these cells is needed after a high dose of chemotherapy.
Collection of Stem Cells
Stem cells are a type of blood cells that have the capacity to develop into any kind of blood cell such as red blood, white blood cell or platelets. These stem cells are present in the blood stream and bone marrow and are initially collected from the patient before the patient receives high dose chemotherapy. This process of collection of stem cells from the patient and infusing them back into the same patient after high dose chemotherapy is called as Autologous Stem cell transplant.
If the stem cells are from another person(donor), then it is called an Allogenic stem cell transplant. The donor can be related, usually a brother or a sister, or unrelated but matched donor. A donor may be used in situations when there is cancer present in the marrow or an autologous transplant was done before, but the disease has relapsed again.
Before collection of stem cells, the patient may have chemotherapy and injections with G-CSF which will increase the number of stem cells in the blood to achieve a successful collection.
On the day of collection of stem cells, the patient/donor is connected to a machine and the patient’s/donor’s blood is taken out from one vein and it passes through the machine to collect the stem cells present in the blood. The blood then passes back into the patient through another vein. This process is done over a few hours.
Once the stem cells are collected, the patient receives the high dose chemotherapy. After the chemotherapy, the stem cells are infused into the patient. These cells go into the bone marrow and start making blood cells again.
Collection of bone marrow
Bone marrow is the spongy material that is present inside the bones. For a bone marrow transplant, the marrow needs to be collected prior to giving high dose chemotherapy. The procedure to collect the marrow is done under general anaesthesia usually in an operation theatre. The marrow may be taken out from different places in the bones and about 1 litre of it may be taken out at the procedure. Once taken out, it is stored and infused into the patient when needed.
Risks and side effects of Stem cell Transplant
Having a stem cell or bone marrow transplant is a complex process and is associated with side effects. This procedure usually involves staying in hospital for a few weeks for the blood cells in the marrow and blood to recover to normal levels after the transplant is done. Common side effects associated with this procedure include
Nausea, Vomiting, Hair loss, altered function of the liver are potential side effects of this treatment.
Risk of Infection as white blood cells are low and the patient to prone to get an infection. The infections could be bacterial, viral or fungal and will usually need antibiotics to control them.
Mucositis is the effect of chemotherapy on the inside lining of the mouth and digestive tract. This can limit the amount of food taken by the patient and other methods of feeding may be used in that instance.
Bleeding is a risk associated with this procedure due to low platelet count, but platelet transfusion can be given to keep the platelet counts up.
Graft versus host disease is a reaction of the body to the transfused cells particularly if the stem cells or marrow is from a donor.
Radiotherapy
Radiotherapy is an option of treatment in some patients with ALL. Radiotherapy is given to the brain in patients who have disease confirmed in the nervous system. In such a situation, treatment is given daily, once a day for 12 days.
Radiotherapy may also be used as a conditioning treatment prior to a stem cell transplant. Conditioning treatment is one where the treatment is aimed to get rid of all blood cells in the body prior to the transplant of stem cells. This conditioning treatment can be chemotherapy or radiotherapy. When radiotherapy is used, it is given to the whole body and is called as total body irradiation (TBI).
Treatment of relapsed or residual disease
A high proportion of patients in induction and consolidation treatment will go into remission. Some patients will not and will have to be treated with other drugs. A proportion of patients who have had a remission after above may develop a relapse of disease sometime later. Treatment options for these patients include chemotherapy with a different combination of drugs than before, stem cell transplant if they have achieved a partial or complete remission after treatment again or alternative targeted or biological therapy if they have Ph+ve disease.
Treatments for childhood leukaemia can impact a child in many ways. Various organs in children are in different stages of development and treatments for this condition can have an impact on that development. Therefore, children who have treatment for leukaemia are prone to get long term side effects of treatment which can manifest months to years after completion. Many childhood leukaemias are potentially curable and therefore it is more important to be aware of these side effects as these children will grow and have many years of life ahead of them. Being aware and recognising these effects at an early stage will help to reduce them and to plan necessary remedies to reduce their impact. Some of these effects are given below. It is important to note that not all patients will get these side effects. Some patients may not get any and others may get some of them.
Learning difficulties
Treatment for leukaemia can impact the development of the brain leading to reduced ability to learn. This can be due to effect of chemotherapy on the brain that is given into the spinal canal or due to effect of radiotherapy that may be given in some patients who have known disease in the nervous system. Children under the age of 5 are most likely to be affected. These problems are mild and should not cause a significant effect on the child’s ability to learn.
Effects on the Heart
Chemotherapy drugs such as Doxorubicin or Daunorubicin can affect the heart by causing reduced function of the heart muscle. This is dependent on the dose of these drugs used and usually the dose given does not exceed the threshold. However, it is important to keep the side effect in mind.
Lung Function
Drugs such as methotrexate given in leukaemia can cause lung toxicity with a risk of fibrosis or scarring of the lung in the long term. This leads to the development of breathlessness in the patient.
Reduced hearing
Radiotherapy to the brain can have an effect on the hearing apparatus in the head leading to reduced hearing.
Reduced fertility
Chemotherapy in boys and girls can lead to delayed puberty and reduced fertility in later life. Radiotherapy to the brain or to the testes in males who have disease in the testes can also develop reduced fertility.
Endocrine dysfunction
Patients who have radiotherapy to the brain can have reduced function of the pituitary gland present in the brain. This can lead to reduced production of hormones from the pituitary gland. Hormones such as the growth hormones produced by the pituitary causes growth of the child and reduced production of that can lead to stunted growth.
Second cancers
Children treated for childhood leukaemia have a small chance of a second cancer in their life as a result of this treatment. Children treated for ALL have a risk of developing AML later in life. The risk with standard ALL chemotherapy is small, about 1% or lower.
Graft versus host disease is a complication of stem cell or a bone marrow transplantation. It is a reaction between the donor’s cells (T cells) that have been transfused into the patient and the patient’s body. The T cells see the host’s (patient) cells as foreign and react to them. The skin, intestine and liver are the organs mostly affected by this condition. GvHD happens in patients with allogenic transplant, where cells that are transplanted from another person. The risk of this complication is lesser if the transplant donor is closely related and there is a good match between the donor and patient. The risk is more if an unrelated donor or a partially matched donor is used.
GvHD can be of two types, acute and chronic. GvHD can also be graded according to its severity.
Grade 1- patient has mild symptoms
Grade 2- moderate symptoms
Grade 3- severe symptoms
Grade 4- very severe symptoms
Acute GvHD is when the complication happens in the first 100 days of the transplant, but it usually happens 2-3 weeks after the transplant. Symptoms of acute GvHD include skin rashes which can be itchy and painful. Other symptoms include loose motions, lack of appetite, vomiting and jaundice (yellowing of eyes).
Chronic GvHD occurs 100 days after the transplant and symptoms of that include skin rashes which can be itchy, skin discolouration, loose motions, dry mouth, jaundice and scarring in the liver. It can affect the lungs leading to cough and breathlessness, eyes causing dryness and pain, aches and pains in the muscles.
A diagnosis of GvHD is made based on the symptoms of the patient and the findings on examination by the doctor. A biopsy of the skin, liver or other area is taken to confirm its presence.
Treatment and Prevention of GvHD is mainly achieved by suppressing the immune system to reduce the reaction between the donor and host cells. Drugs are used to help with this. Commonly used drugs include Infliximab, Etanercept, Mycophenolate mofetil (MMF), Sirolimus, Tacrolimus, Rituximab, Ibrutinib, Azathioprine and Pentostatin. Common supportive treatments such as pain killers, medications to reduce vomiting, loose motions, antibiotics to reduce or treat infections, artificial tears to prevent dry eyes, nutritional and fluid support and other measures are used to help control the condition. Patients who have chronic GvHD can have symptoms that are present over a long period of time and supportive measures for the skin, liver, lungs, eyes, vagina are continued. Necessary precautions




