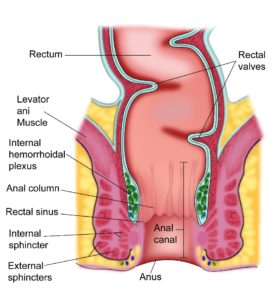
Anus is the lower most part of the digestive tract. The digestive tract comprises the mouth, oesophagus, stomach, small intestine, large intestine, rectum and ending at the anus. The anus can be divided into the anal canal and the anal margin. The anal margin is the outer most extent of the anus and is seen from outside. The upper part of the anal canal connects to the rectum.
The function of the anus is to allow the faeces to be eliminated by the body and to control the mechanism of that function.
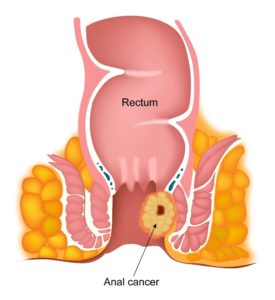
A cancer that arises from the anus is called Anal Cancer. Anal cancer is typically a squamous cell carcinoma and makes up about 95% of all anal cancers. Other types of anal cancer include adenocarcinoma, basaloid carcinoma and skin cancers developing around the anus such as melanomas and basal cell carcinomas. Anal cancer is more common in men than women.
According to Globocan data 2018, there were 4895 new Anal cancers diagnosed in India in 2018, making up 0.04% of all cancers.
Anal Intraepithelial neoplasia or AIN as it is called, is a pre-cancerous condition, that over years can develop into an anal cancer. Infection with HPV or human papilloma virus is the commonest cause of AIN and anal cancer. Other risk factors for development of AIN include multiple sexual partners, anal sexual intercourse, HIV infection, presence of warts around the genital system and smoking.
AIN may not produce any symptoms at all but may cause itchiness, discharge or bleeding from the anus.
If AIN is suspected, a biopsy of the area is taken to confirm the diagnosis. Sometimes, AIN is seen when a diagnosis of anal cancer is suspected. When AIN is diagnosed, it is named as AIN1, AIN2 or AIN3 depending on the amount of involvement of the area by the AIN.
Treatment of AIN depends on the extent of disease present around the anus. Treatment options consist of local creams, infrared radiation, surgical removal or immune modulation treatment.
Prevention strategies for AIN include vaccination for HPV and this is discussed in the prevention of cancer section.
HPV Infection
Infection with HPV or human papilloma virus is a risk factor for development of Anal cancer. HPV is present in up to 90% of patients with Anal cancer. HPV infection is transmitted from one person to another through sexual contact. It is a risk factor for other cancers such as Cervical, Vulval and Vaginal cancers. HPV infection is common and only a small proportion of patients with HPV infection develop a cancer.
Reduced Immune status
Patients with a reduced immune status due to infections such as HIV/AIDS have an increased risk of developing Anal cancer. Reduced immune system due to medications also poses a risk.
Sex
Having anal sexual intercourse increases the risk of developing anal cancer. This is due to increased risk of getting an HPV infection. Having multiple sexual partners also increases the risk.
Smoking
Smoking increases the risk of developing anal cancer and stopping smoking after diagnosis gives a better outcome than when continuing to smoke.
Age
As with many cancers, the risk of developing an anal cancer increases with age.
Anal Intraepithelial Neoplasia (AIN)
Having a pre-cancerous condition such as AIN increases the risk of developing an anal cancer. More detail about AIN can be found in a separate section.
Anal cancer can produce symptoms which are listed below.
Bleeding
Bleeding when passing a motion can be a symptom due to anal cancer. This bleeding can be painful or painless. If bleeding happens, it is important to see a doctor. Not all bleeding is due to cancer and it is due to common causes such as piles etc. but it is important to be checked up.
Itchiness in the Anal region
Persistent itchiness around the anus can be a symptom due to anal cancer. Again, this can happen due to many reasons, but it is important to be checked if the symptoms persist.
Pain
Pain in the anal region or in the lower abdomen can also be a symptom of anal cancer.
Feeling of a lump or a mass in the Anus
A feeling of a lump or a mass in or around the anus or rectum can be a symptom of anal cancer.
When an Anal cancer is suspected, the following tests are done
Clinical Examination and Biopsy
A thorough examination by the doctor, of the area suspected of anal cancer can determine the extent of spread around the anus. Sometimes, the examination is done under anaesthesia to enable the doctor to fully examine the patient without causing any pain. A biopsy of the suspected area is taken to confirm or refute the diagnosis of anal cancer.
In patients with enlarged lymph nodes in the groins, an FNA of these enlarged nodes is done to look for spread of anal cancers into the nodes.
CT Scan
CT scan of the chest, abdomen and pelvis can be done to look for spread of the cancer into these areas from the anus.
MRI Scan
An MRI scan is done mainly to assess the cancer in the anus in more detail particularly to look at spread of cancer locally around the anus. The MRI scan done here is usually an MRI of the pelvis.
PET-CT Scan
A PET-CT scan is the most sensitive scan to look for evidence of spread of anal Cancer from its place of origin to other areas in the body. If this scan is available, it is the investigation of choice in this condition.
Staging of cancer is an important step in the process of management of cancer. The stage of the cancer determines the most appropriate treatment for the cancer. Stage also enables to estimate the chances of cure and the average survival of the patient.
Cancer of the Anus is staged with the TNM staging and the number staging system.
TNM Staging
Primary tumour (T)
| T0 | Primary tumour not seen |
| Tis | Carcinoma in situ (Bowen’s disease, high-grade squamous intraepithelial lesion (HSIL), (anal intraepithelial neoplasia II-III (AIN II-III)) |
| T1 | Tumour 2 cm or less in size |
| T2 | Tumour more than 2 cm but not more than 5 cm in size |
| T3 | Tumour more than 5 cm in size |
| T4 | Tumour of any size invades adjacent organs, eg, vagina, bladder, urethra |
Regional lymph nodes (N)
| N0 | No regional lymph node metastasis seen |
| N1 | Metastasis present in perirectal lymph nodes |
| N2 | Metastasis in unilateral internal iliac and/or inguinal lymph nodes |
| N3 | Metastasis in perirectal and inguinal lymph nodes and/or bilateral internal iliac and/or inguinal lymph nodes |
Distant metastasis (M)
| M0 | No distant metastasis |
| M1 | Distant metastasis seen |
Number Staging
Stage 1
In stage 1 Anal cancer, the tumour is 2cm or less in size and has not spread to nearby lymph nodes or any structures.
Stage 2
In stage 2 Anal cancer, the tumour is larger than 2cm in size but has not spread to any lymph nodes or surrounding structures.
Stage 3
In stage 3, the cancer is of any size and has spread to the lymph nodes in the pelvis or groin area. There could also be spread of tumour into structures around the anus.
Stage 4
Any anal cancer that has spread to other parts of the body beyond pelvic and groin lymph nodes and surrounding structures.
The options of treatment for Anal cancer (Squamous cell Carcinoma) include Chemo-Radiotherapy, Surgery, Radiotherapy alone and Chemotherapy alone.
Chemo-Radiotherapy
This is by far the commonest and best option that is used to treat anal cancer that is not metastatic, i.e, cancer that has not spread to distant sites in the body.
In this option, chemotherapy is added on to radiotherapy which is the main component of treatment. The combination provides the best chance of control and cure. The radiotherapy is given once a day, 5 days a week for up to 5-6 weeks. Commonly used chemotherapy drugs in this setting include Mitomycin and Fluorouracil. The drugs are given in the first and last weeks of treatment.
Alternatively, Cisplatin and Capecitabine are also used. Radiotherapy is given to the anus and the whole of the pelvis including the groins.Radiotherapy techniques such as 3D conformal therapy, IMRT, VMAT or other techniques can be used.
Common side effects of this treatment include redness and soreness of the skin particularly around the anus and groins, tiredness, low blood counts and risk of infection, diarrhoea and burning sensation when passing urine. Long term side effects related to urination, opening of bowels and sexual health may be present in some patients after chemo-radiotherapy.These include continued loose motions, reduced ability to control stool function, pain and lack of sexual interest and inability to get anerection in a male, among others.
Surgery
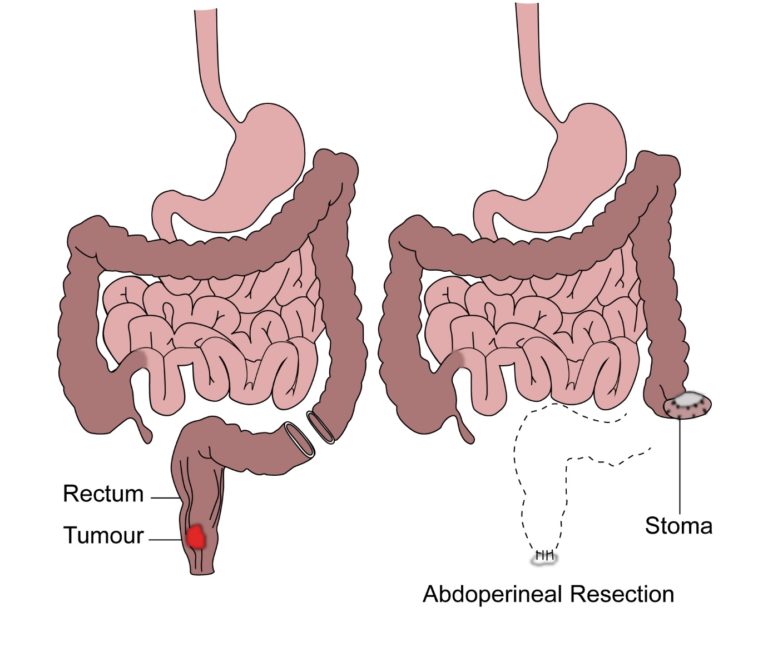
Surgical removal of anal cancer is also a treatment option but is used less commonly than chemoradiotherapy. The surgical removal is an operation called AP resection which involves removal of the anus, rectum and the formation of a colostomy(stoma) which is an opening in the abdomen. Stools or motion is passed through the opening into a bag. As chemo-radiotherapy has an equal chance of curing the cancer as a surgical removal and there is no need for a bag after the former option, this is preferred. Surgery is considered and done in patients where chemo-radiotherapy fails to cure the patient from the cancer. The AP resection can be done either as an open procedure or a laparoscopic procedure. In patients who are due to have chemoradiotherapy but are having difficulty with passing motion due to pain or blockage, a temporary colostomy is done before starting chemoradiotherapy.
Surgery can be considered as an option of treatment for very small and early anal cancer instead of chemo-radiotherapy, but will need strict follow up to look for recurrence.
Radiotherapy
In patients with poor general health who cannot tolerate chemotherapy and radiotherapy together, radiotherapy alone is given as treatment. This type of treatment is inferior in terms of achieving cure as compared to chemo-radiotherapy.
Chemotherapy
In patients where there is spread of cancer from the pelvis region to other parts of the body, treatment then is to control disease rather than cure it. Here chemotherapy alone is used to help control the disease and improve symptoms. Commonly used drugs in such a setting include Cisplatin, Carboplatin, Docetaxel, Paclitaxel, Doxorubicin, Mitomycin, Fluorouracil, Capecitabine and Irinotecan. Immunotherapy with Nivolumab and Pembrolizumab can also be considered.




