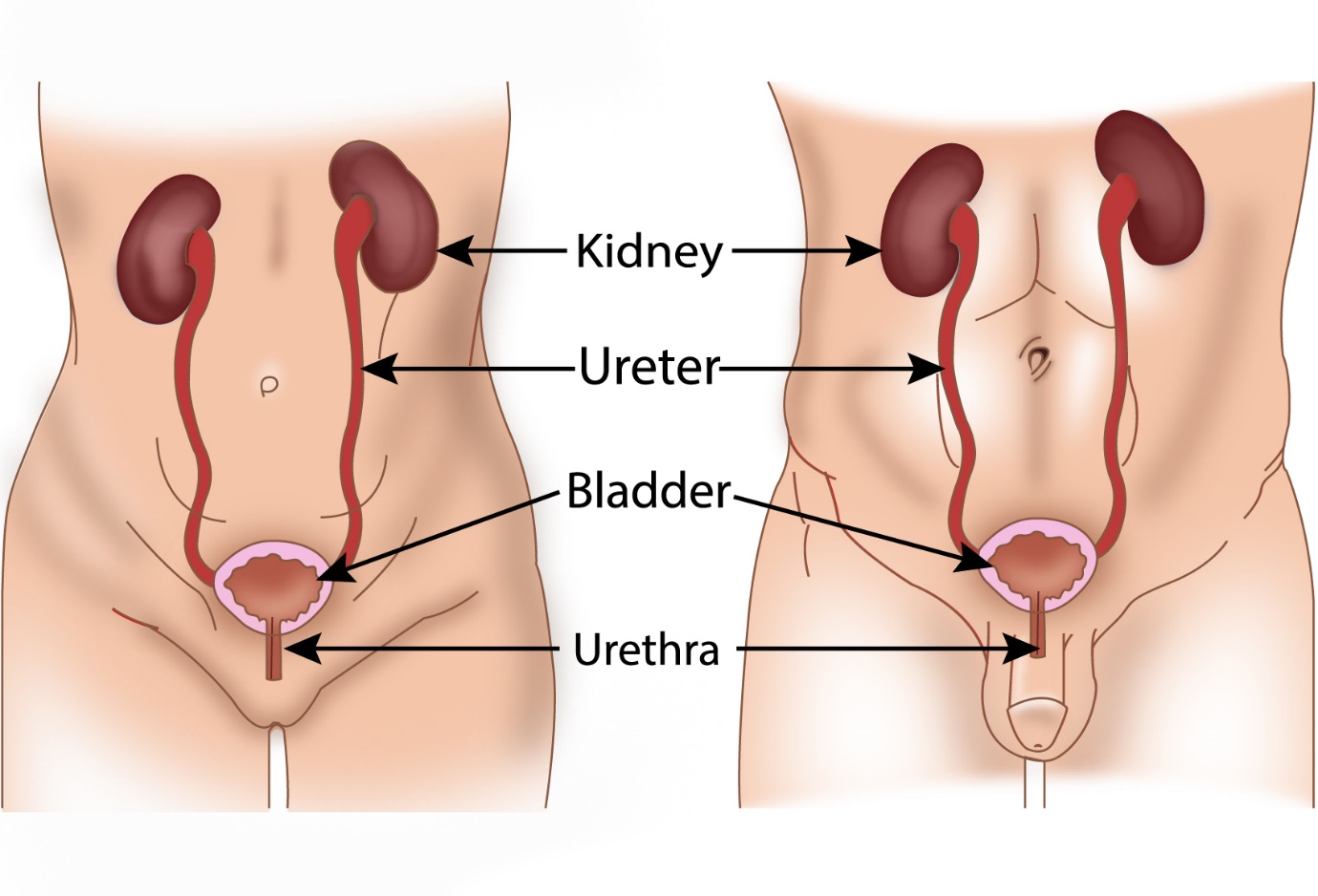
Bladder or urinary bladder is a bag like muscular structure present in the lower part of the tummy called the pelvis. Its function is to collect and store the urine that comes from the kidneys. The bladder is connected to the kidneys by the ureters, one for each kidney.
On the other side, the bladder connects to the outside through the urethra.
The bladder consists of four layers. The inner most layer is called the mucosa or mucosal layer. The other layers from inside out are submucosa, muscle layer and serosal layer.
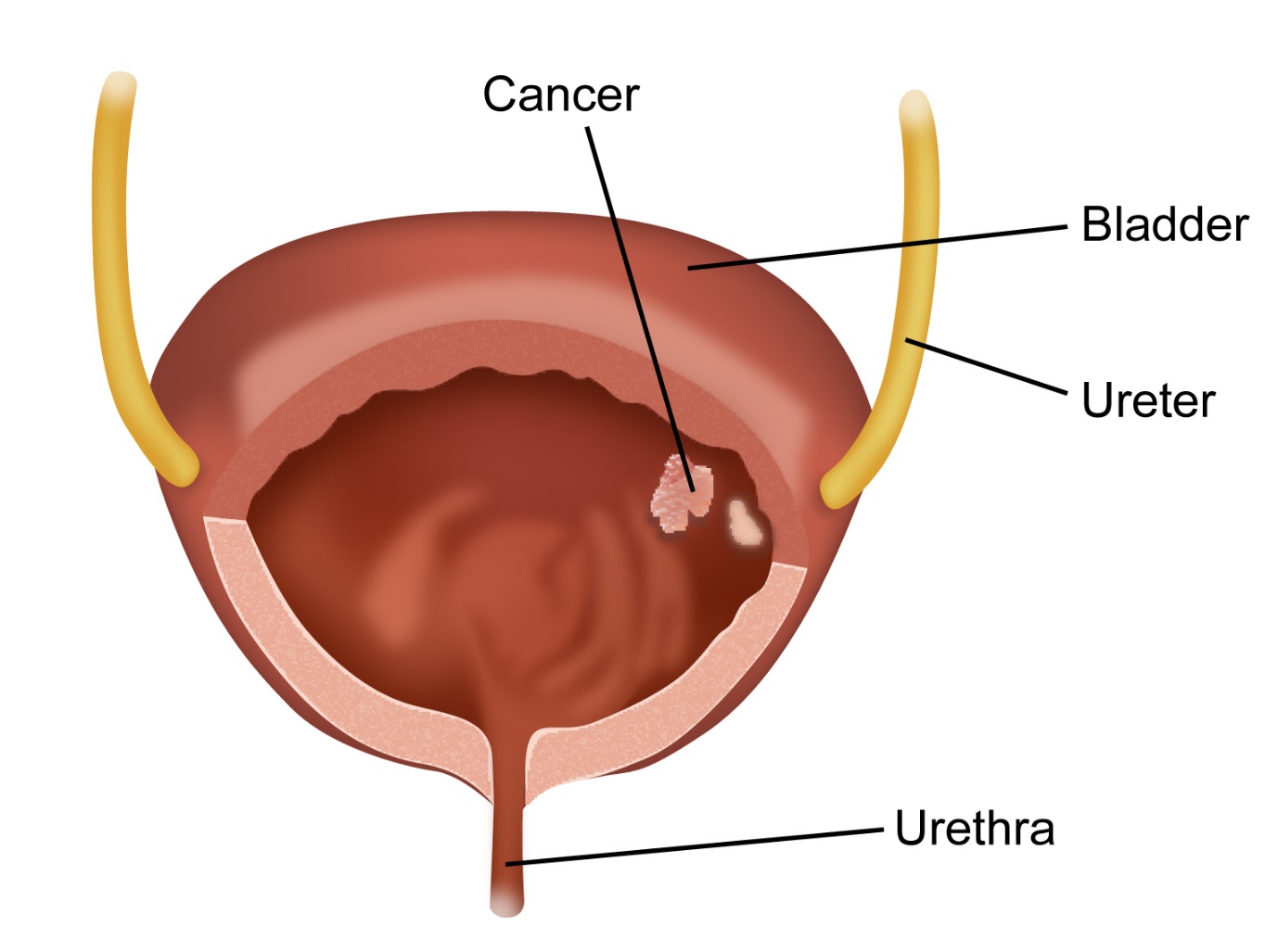
Bladder cancer is cancer that starts in the bladder. The cancer starts in the mucosal layer and can spread to the other layers of the bladder. Bladder cancer is mainly transitional cell carcinoma (TCC) type, which is the most common form and develops from the transitional cells that make up the mucosa. Other types of bladder cancer such as squamous cell carcinoma, adenocarcinoma, and small cell carcinoma are rare.
Based on its features at the time of diagnosis, TCC is termed as papillary (early form), CIS (carcinoma in situ), and muscle invasive (involving the muscle layer).
According to Globocan data 2018, there were 18926 bladder cancers accounting for 1.6% of all cancers.
There are several risk factors implicated in bladder cancer.
Smoking
Smoking is a risk factor for developing bladder cancer. This can be any form of smoking from cigarettes to pipes. Chemicals in the smoke that is inhaled are absorbed into the bloodstream and then excreted by the kidneys into the bladder. These chemicals can cause damage to the cells lining the bladder leading to the development of cancer. The risk increases proportionately depending on the duration and intensity of smoking. Stopping smoking reduces the increased risk of bladder cancer.
Chemicals
Exposure to chemicals in certain occupations leads to an increased risk of bladder cancer.
Occupations implicated are leather workers, painters, metal workers, rubber industry workers, electricians, miners and people working in carpet and plastic industry. The latent period between exposure to chemicals and development of cancer can be very long up to 20 years or more. A lot of the cancer-causing chemicals have been banned and not used anymore in these industries.
Drinking water
Chlorination of drinking can be a risk factor for bladder cancer. Studies have shown that long term use of chlorinated drinking water leads to an increased risk of developing bladder cancer.
Chronic Infections
People who have repeated bladder infections and those people who have regular irritation of the bladder due to presence of long term urinary catheters or bladder stones have an increased risk of developing bladder cancers particularly squamous cell cancers.
Age and Gender
Bladder cancer is more common in the elderly than young people and is more common in males as compared to females.
Family History
The risk of getting bladder cancer is slightly increased if a close relative has had one.
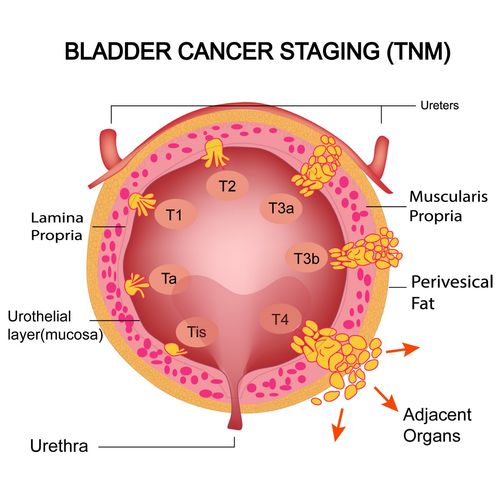
The stage of a cancer is a term used to describe the size and location of the cancer in the body.
Knowing the stage of the cancer helps the doctors to decide on the most appropriate treatment. Bladder cancer is staged based on the TNM staging system or the number system.
Staging with either system is based on the extent of the tumour in the bladder, the spread of the cancer locally in the bladder and into the lymph nodes and spread of cancer into other parts of the body.
TNM Staging
TNM stands for Tumour Node and Metastases.
T Staging
| Ta | non-invasive papillary tumour (tumour does not invade into deeper layers from the mucosa). These tumours are exophytic (grow outwards) |
| Tis | Carcinoma in situ- tumour is flat and present in the mucosa but there is no involvement of the deeper layers of the bladder |
| T1 | Tumour involves the connective tissues below the mucosal layer |
| T2 | Tumour goes beyond the connective tissues and involves the muscle layer of the bladder. T2 is subdivided into T2a when inner half of the muscle is involved and T2b when outer half of the muscle is involved |
| T3 | Tumour involves the fat layer on the outside of the bladder. This can be subdivided into T3a when this involvement is seen microscopically and T3b when the involvement is seen with the eye |
| T4 | Tumour involves other structures outside the bladder. It is T4a when it involves the prostate, uterus or vagina and T4b when it involves the wall of the abdomen or pelvis |
Ta and Tis are non-invasive tumours and T1 to T4 are invasive cancers
N Staging
| N0 | Lymph nodes not involved by bladder cancer |
| N1 | Involvement of one single lymph node in the pelvis by bladder cancer |
| N2 | Involvement of multiple lymph nodes in the pelvis by bladder cancer |
| N3 | Involvement of common iliac lymph nodes by bladder cancer |
M Staging
| M0 | No spread of bladder cancer to areas other than mentioned above |
| M1 | Spread of cancer to other areas of the body than those described above |
Grading of Bladder Cancer
Ta cancers can be divided into low grade and high grade depending on their capacity to grow and spread. Tis cancers are usually classified as high grade. Treatment options are different depending on the grade of cancer.
Invasive cancers are graded from Grade 1 to Garde 3 with grade 1 being least aggressive and Grade 3 being more aggressive. Being more aggressive would mean a higher capacity for the cancer to grow and spread and will usually need a more aggressive treatment plan.
Bladder cancer can present in the following ways.
Blood in the Urine
Passing blood in the Urine(haematuria) is one of the common symptoms of bladder cancer. Most times this bleeding is painless. When bleeding happens, it may be coloured red, pink or brown. It is advisable to see a doctor if there is blood seen in the urine. The bleeding can be continuous or intermittent. Sometimes, there may not be visible blood but only found on microscopic examination when other symptoms are investigated.
Other symptoms
Other symptoms that can be present in bladder cancer include urinary symptoms such as needing to pass urine more often, burning or pain when passing urine, difficulty passing urine or urgency to pass urine. symptoms such as pain in the lower part of the abdomen, tiredness, loss of appetite, weight loss can also be present in advanced stages of bladder cancer.
It is important to know that all the above symptoms can happen due to other causes as well such as bladder stones, infections or prostate enlargement. So, having these symptoms doesn’t mean that there is cancer, but it is advised to see a doctor if these symptoms persist.
When a Bladder Cancer is suspected, the following tests are done.
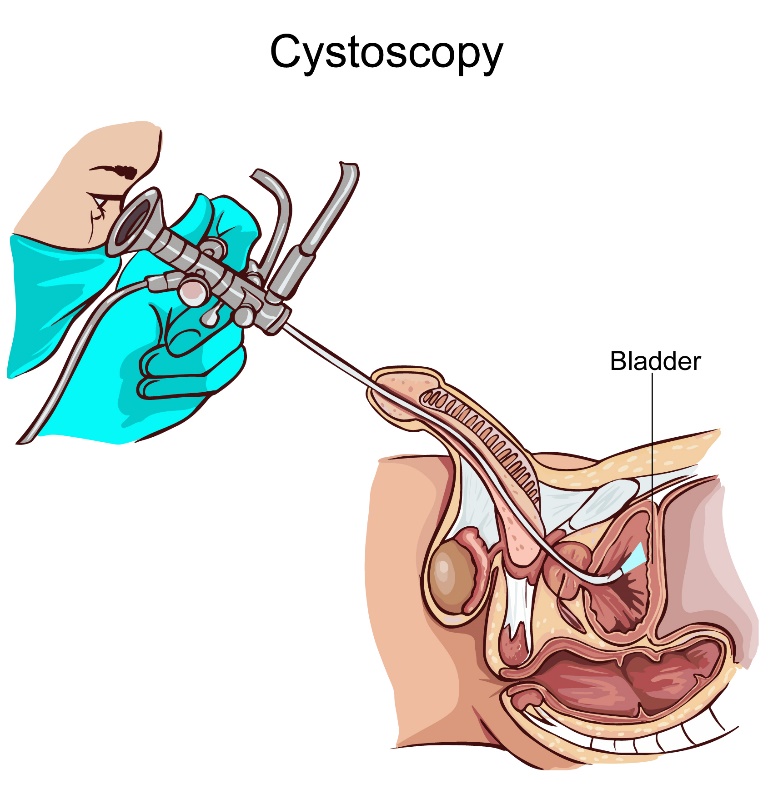
Flexible cystoscopy
This is a test that is usually done by a Urologist where a thin tube with a camera and light (cystoscope) is passed into the bladder through the urethra. The person doing the test will be able to see inside the bladder for abnormalities. The procedure can be done under local or general anaesthesia. If the doctor finds a tumour, a biopsy can be taken of any abnormal areas. Some centres may do a blue light cystoscopy which can help to find abnormal areas more easily. The patient will be able to go home on the day of the procedure. Mild burning or stinging can happen as a side effect of the procedure.
Blood Tests
Routine blood tests are done to look at the general health of the patient.
Urine Tests
Routine urine tests as well as tests to look for cancer cells in the urine can be done.
Ultrasound Scan
An ultrasound scan of the bladder or urinary tract is done to look for abnormalities in the bladder or other parts of the urinary tract. An ultrasound scan uses sound waves to get a picture. The test is done by putting some jelly on the area to be tested and a probe is rubbed against the skin to get the images. Before the test you will be asked to drink water to make your bladder full. It takes a few minutes and is painless.
CT Scan or CT Urogram
CT Scan or computed tomographic scan is a commonly used test for diagnosis and staging of cancer. A CT scan uses x-rays to get a picture of the organs inside the body. A CT Urogram is a CT scan used to look for abnormalities in the urinary tract. Once, a cancer is diagnosed, a CT scan is used to help in staging of the cancer. The scan is painless and is done in 10-20 minutes. A dye is injected prior to the scan to get better images.
PET CT Scan
A PET CT scan is a specialised CT scan in which a special dye is injected into the vein an hour or so before the scan. A PET CT scan is usually done to stage the bladder cancer. It may help to stage a bladder cancer more accurately than a standard CT scan. PET CT scans are only done when more advanced bladder cancers are found. There is no benefit of this scan in early stage bladder cancers.
MRI Scan
MRI scan uses magnetism to get pictures of the inside of the body. This type of scan is not a routine test in the diagnosis or staging of bladder cancer.
Biopsy
A biopsy is a process where a sample of abnormal tissue is taken and looked at under the microscope by the Pathologist. After the sample is taken, it is processed and special stains may be added to it before it is interpreted. All of this can take a few days before a report is issued. Bladder cancer is usually diagnosed from a biopsy taken at cystoscopy.
Surgery
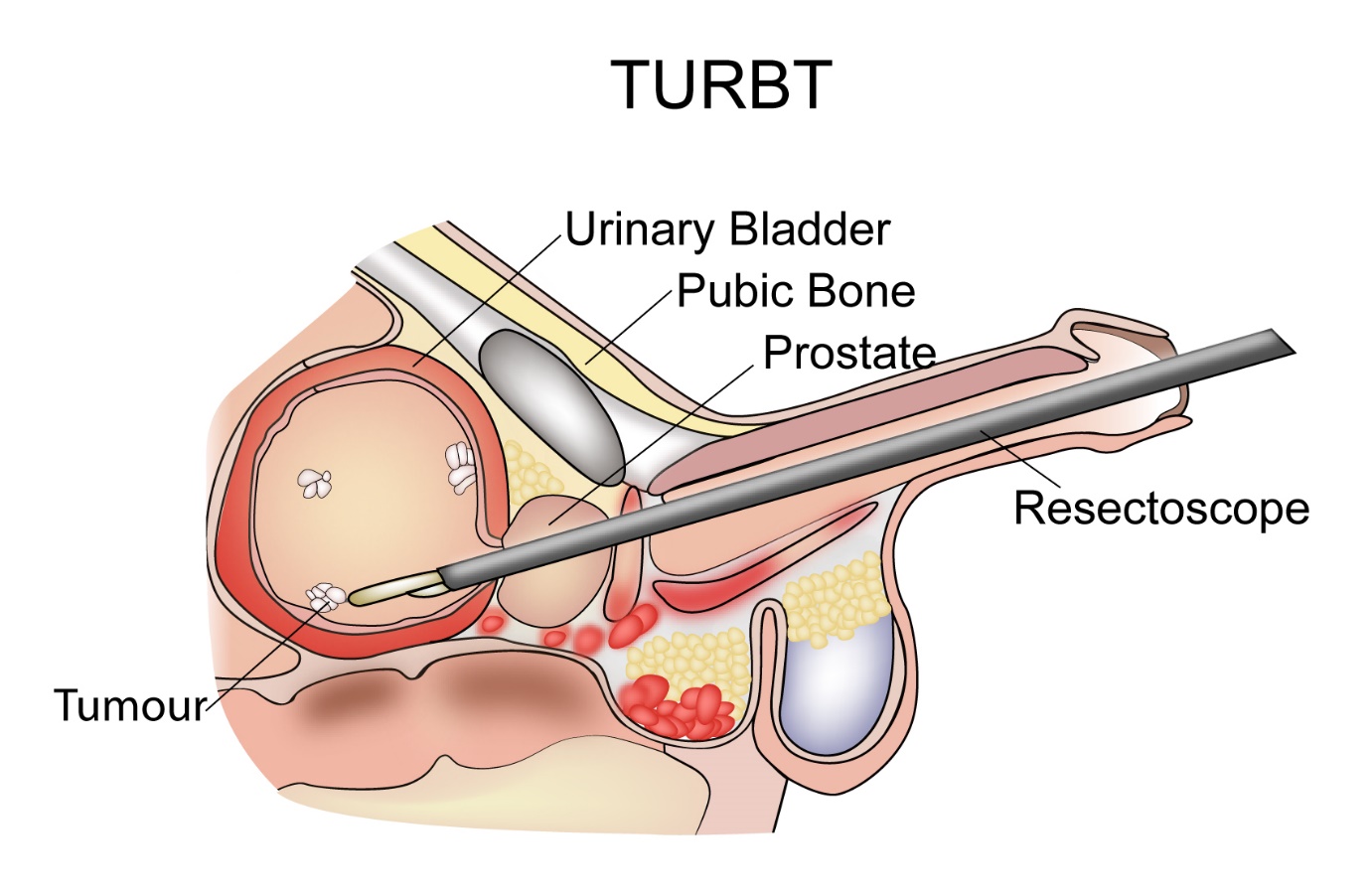
Surgery is usually the first component of treatment for non-invasive bladder cancer. This surgery involves removal of the bladder tumour. This is done under general anaesthetic by the Urologist using a cystoscope. Surgical instruments are inserted through the cystoscope and the bladder tumour is resected. This type of resection is called transurethral resection of bladder tumour (TURBT). Soon after the resection, some surgeons may give local chemotherapy into the bladder. This treatment has been shown to reduce the risk of recurrence. Following this initial surgery, a pathology report will be available which will inform about the completeness of the resection and also the complete stage and grade of the cancer. Decisions will then be made as to whether more surgery or other treatment options are needed.
In some cases, surgery to remove the whole bladder(cystectomy) is needed, if the treatments detailed in this section are not effective and cancer is still present in the bladder. The details of this option are explained in the invasive bladder cancer section.
Intravesical chemotherapy
Following TURBT, there is an option of giving chemotherapy into the bladder. This is called as intravesical chemotherapy. This can be as a single dose immediately after surgery or six weekly courses after surgery. Your doctor will discuss the options with you if appropriate in your circumstance. This treatment is given to reduce the risk of recurrence of non-invasive tumour.
The drugs commonly used for this procedure are Mitomycin-C, Epirubicin, Doxorubicin or Gemcitabine. As these drugs are given in to the bladder only, they are not absorbed into the body and therefore will not cause any general side effects. The only side effects will be local in the bladder in the form of increased frequency of urination, burning or stinging sensation or bleeding when passing urine. These effects will settle in a few days.
Intravesical BCG
In some instances of non-invasive bladder tumours, particularly when the tumour is described as high grade, or there are multiple tumours in the bladder, intravesical BCG is an option of treatment. This involves giving BCG into the bladder. BCG is a bacterium which is used as a vaccine to prevent Tuberculosis. BCG is known to produce a local immune response in the bladder which then helps kill off any remaining cancer cells and reduce the risk of recurrence of bladder tumour.
This treatment is usually given once a week for 6 weeks and then there is a six-week break. After that, it is given again. In some instances, BCG can be continued with a maintenance dose of 1-3 weeks every six months for 1-3 years.
BCG can have side effects which include stinging or burning sensation when passing urine, bleeding, pain and increased frequency of urination and general side effects such as fever and tiredness.
Surveillance
Following above treatments, it is important to have check up by your treating doctor to look for recurrence of this cancer. Your doctor will tell you how often you need to see them to have this follow up. Repeat cystoscopies form part of the surveillance programme.
Surgery
Surgery is one of the main forms of curative treatment for patients with invasive bladder cancer. The operation that is done is called a Radical cystectomy. It is done under a general anaesthetic. This procedure is carried out in patients where the disease is confined to the bladder area and there is no distant spread of disease. A radical cystectomy entails removal of the bladder along with adjacent organs and lymph nodes. These can include the prostate, seminal vesicles and part of urethra. In women it could include the uterus, cervix, ovaries and fallopian tubes. The radical cystectomy can be done as an open procedure (large cut in the abdomen), laparoscopic (see cancer FAQ section) or more recently robotic. A partial cystectomy, where only a part of the bladder containing the tumour is removed is used as an option occasionally.
In patients who have good level of fitness, having chemotherapy prior to surgery has been shown to be beneficial by improving the chances of a cure. This will be for 3 months in duration and will be followed by the cystectomy. This method of giving chemotherapy prior to definitive treatment is called neo-adjuvant chemotherapy.
As the bladder normally stores urine and that is now being removed, alternate arrangements for urine to pass out of the body need to be made.
These options include-
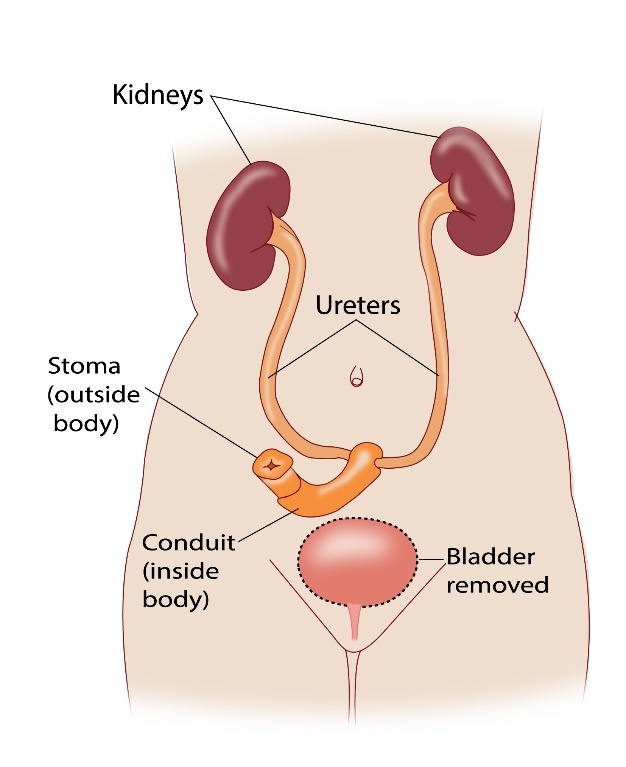
Urostomy
This is the most common option used where the surgeon removes a small part of the small intestine and connects the ureters (connecting the kidneys to the bladder) to one end of this small intestine. The other end of this piece of small intestine is connected to the abdominal wall in the form of an opening. The urine that comes out of this end is collected into a bag which fits this opening tightly.
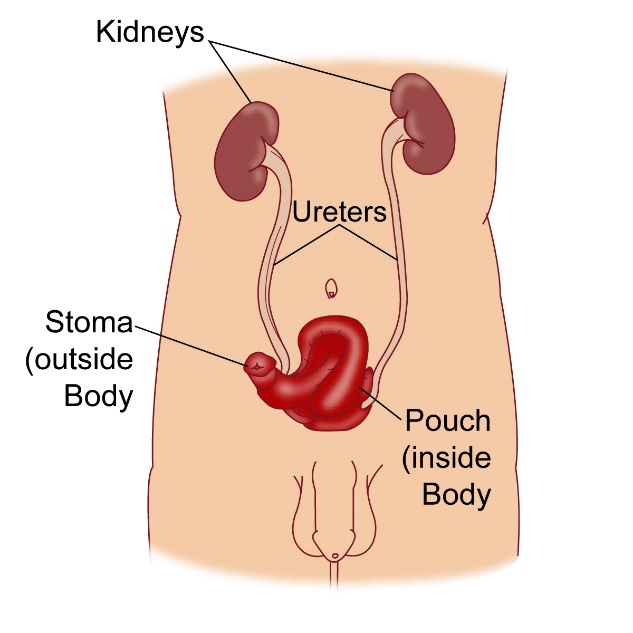
Continent Urinary diversion
In this method a pouch is made from a piece of small intestine. The ureters are connected to the pouch. The other side of the pouch is attached to the abdominal wall through an opening. The benefit of this method over the urostomy is that there is no need for a bag. Instead, the patient needs to place a catheter into the pouch and urine drains outside through that.
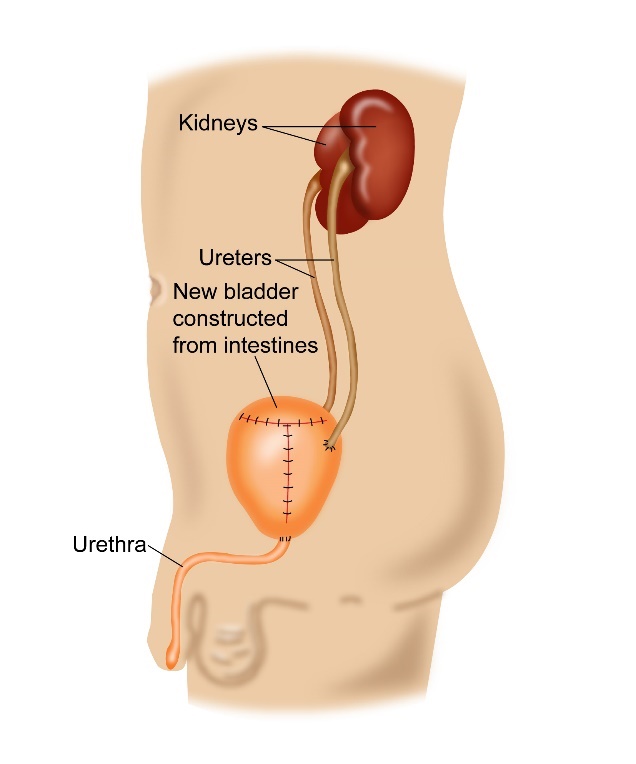
Neo bladder
Here a pouch is again made from a part of small intestine and the ureters are attached to it. But, instead of making an opening in the abdominal wall, the urethra is connected to the pouch and so urine passes in the normal route.
All these methods have their advantages and disadvantages. It is best to weigh the pros and cons of these different methods before a decision is made.
Side Effects of Radical Cystectomy
Potential side effects of radical cystectomy include pain, infection, sexual dysfunction after surgery, blockage of urinary passages or tubes. Passing of blood in the urine is common initially but will settle over a few days to weeks.
Radiotherapy is another curative option of treatment for patients with invasive bladder cancer. Radiotherapy is generally given to patients who are not fit for a radical cystectomy or who do not wish to have a cystectomy. The advantage of radiotherapy is that there is still a functioning bladder after treatment and some patients prefer that over surgery.
Radiotherapy generally is given daily, five days a week for six and a half weeks. The total duration of treatment may vary from centre to centre depending on the type of treatment schedule they use. In fit patients, radiotherapy is given together with chemotherapy (called chemo-radiotherapy) and this has been proven to be more beneficial than radiotherapy alone. Also, having chemotherapy prior to radiotherapy (neo-adjuvant chemotherapy) is known to be beneficial. Therefore, a fit person choosing to have radiotherapy as a definitive treatment will have 3 months of chemotherapy first, followed by a combination of chemotherapy and radiotherapy for up to six and a half weeks.
In patients with stage 4 bladder cancer, where there is distant spread of cancer, radiotherapy is not a curative option but is used to control symptoms such as bleeding, pain etc. Here the treatment is given over a shorter period ranging from 1 to 10 days.
Side effects of Radiotherapy
Side effects of radiotherapy include tiredness which is present mainly towards the latter half and end of treatment. This can last for up to a few months.
Bladder and bowel symptoms
Bladder symptoms are in the form of frequency, burning or stinging sensation, urgency of urination, bleeding. Bowel effects include diarrhoea and passing of blood. These effects settle a few weeks after the treatment finishes. Some of these symptoms may continue into the long term.
Skin changes
The skin over the treated area can get red and sore towards the end of treatment. Occasionally skin can break leaving a raw area. Hair loss on the treated skin will be there and some of it will grow back after some time.
Effects on genital organs
As bladder radiotherapy involves treating the pelvis, the reproductive organs can be affected by radiotherapy leading to infertility, difficulty having an erection and narrowing of the vagina.
Chemotherapy is use of anti-cancer drugs given in the form of injections, drips and tablets. These drugs help kill cancer cells by causing maximum damage to them and at the same time causing some damage to normal tissues. The side effects that happen from chemotherapy are due to the effect of these drugs on normal tissues. There are a number of chemotherapy drugs used to treat cancer. These drugs can be used either in combination or as single agents. Chemotherapy is given as cycles, with each cycle lasting between 1 to 4 weeks, usually 3 weeks. The gap between two chemotherapy cycles is for the body to recover before the next dose. A course of chemotherapy usually lasts for some months.
Chemotherapy in bladder cancers is used at various stages of the disease process.
In non invasive bladder cancer, chemotherapy is given into the b;adder after surgery. See the section on surgery in bladder cancer for more details of this aspect.
In invasive bladder cancer, chemotherapy is used prior to surgery or radiotherapy. This approach is called neo-adjuvant chemotherapy and is given to increase the chances of cure when given in this manner. Usually 4 cycles of chemotherapy are given. In some situations, chemotherapy is not given before surgery but after surgery. This approach is called Adjuvant chemotherapy. In the setting of bladder cancer, neoadjuvant chemotherapy is preferred over adjuvant chemotherapy.
When Radiotherapy is used as a curative option of treatment, chemotherapy is given alongside the radiotherapy. This type of treatment is called concurrent chemo-radiotherapy and this method of treatment has been shown to be better than radiotherapy alone.
It has to be noted though that not all patients will be fit enough to have chemotherapy in these settings, and the Oncologist will determine the fitness and suitability for such treatment.
In patients with stage 4 disease, where treatment options are to control the disease, chemotherapy is used to reduce the cancer and improve symptoms. This method is called palliative chemotherapy. Here chemotherapy drugs are given as combinations or as individual drugs. The treatment is given for up to 6 cycles with scans in between to check for response.
The common drugs used in invasive bladder cancer chemotherapy are-
Gemcitabine, Cisplatin, Carboplatin, Methotrexate, Doxorubicin, vinblastine, Paclitaxel, Docetaxel, Vinflunine. These drugs when given in a combination are usually Gemcitabine and Cisplatin or Gemcitabine and Carboplatin or MVAC(Methotrexate, Vinblastine, Doxorubicin and Cisplatin).
Immunotherapy is use of drugs that alter how the immune system in the body works. This type of treatment has been used in some cancers for a long time, but newer immunotherapy drugs have shown more promise and are being used more often in a number of cancers including invasive bladder cancer.
Newer Generation Drugs
In simplistic terms, the newer immunotherapy drugs called checkpoint inhibitors are antibodies against PD-1 or PD-L1 receptors. These receptors are useful in helping the cancer cell to be identified by the body’s immune system (T Cells) as a friend and prevents the immune system from killing the cancer cells. Cancers can produce more of these receptors and will be able to evade the immune system of the body. By using the antibodies against PD-1 and PD-L1, there is a block of this pathway and this enables the body’s immune system to attack the cancer cells and kill them.
As of now, this therapy is used in stage 4 bladder cancers where the cancer has spread to different parts of the body and the aim of treatment is to control the disease.
The drugs used currently in bladder cancer include Atezolizumab, Pembrolizumab, Nivolumab, Durvalumab and Avelumab. They are used as second line treatments after initial treatment with chemotherapy that contains either Cisplatin or Carboplatin.
These treatments are given as drips into the veins and are given once every 2-3 weeks.
Tests to look for benefit of Immunotherapy
Tests to look for the presence of and level of PD-L1 in the cancer are available and some of these immunotherapy drugs show a better response in patients where there are higher levels of PD-L1 expression. However, in bladder cancer this test is not required.
Side Effects of Checkpoint Inhibitiors
Even though immunotherapy causes less side effects than chemotherapy in general, these drugs are associated with side effects and these are listed below. Some of these side effects can be severe and life-threatening needing to stop the drug.
Common side effects of checkpoint inhibitors include tiredness, cough, breathlessness, loose motions, nausea, vomiting, fever, skin, itching, headaches, confusion joint pains or swelling of joints. Most of these effects are mild and controlled with medications.
These drugs, as they affect the function of the immune system can cause immune system mediated side effects which can affect many organs in the body such as lungs, liver, thyroid, intestine and pituitary gland causing reduced function in those glands and produce symptoms the patient can feel unwell with. Such side effects should be brought to the attention of the doctor.




