Breast Cancer
The breast is a structure made up of gland like tissue, ducts, fat and supportive tissue. The gland like tissue is made up of lobes and lobules which produce milk. The ducts are tubes that help transport milk from the lobes to the nipple. The fat and the supporting structures give shape and form to the breast.
The normal breasts can vary in size and shape through a woman’s life. In younger women, breasts are larger and denser, and in older women, breasts are smaller and less dense. Breasts change in size and consistency close to a menstrual period. They can feel lumpy at that time.
The breast and axilla (arm pit) contain lymph nodes as seen in the picture below. The lymph nodes are part of the immune system and help protect against infections. They help drain the lymphatic fluid from the surrounding area back into the blood.
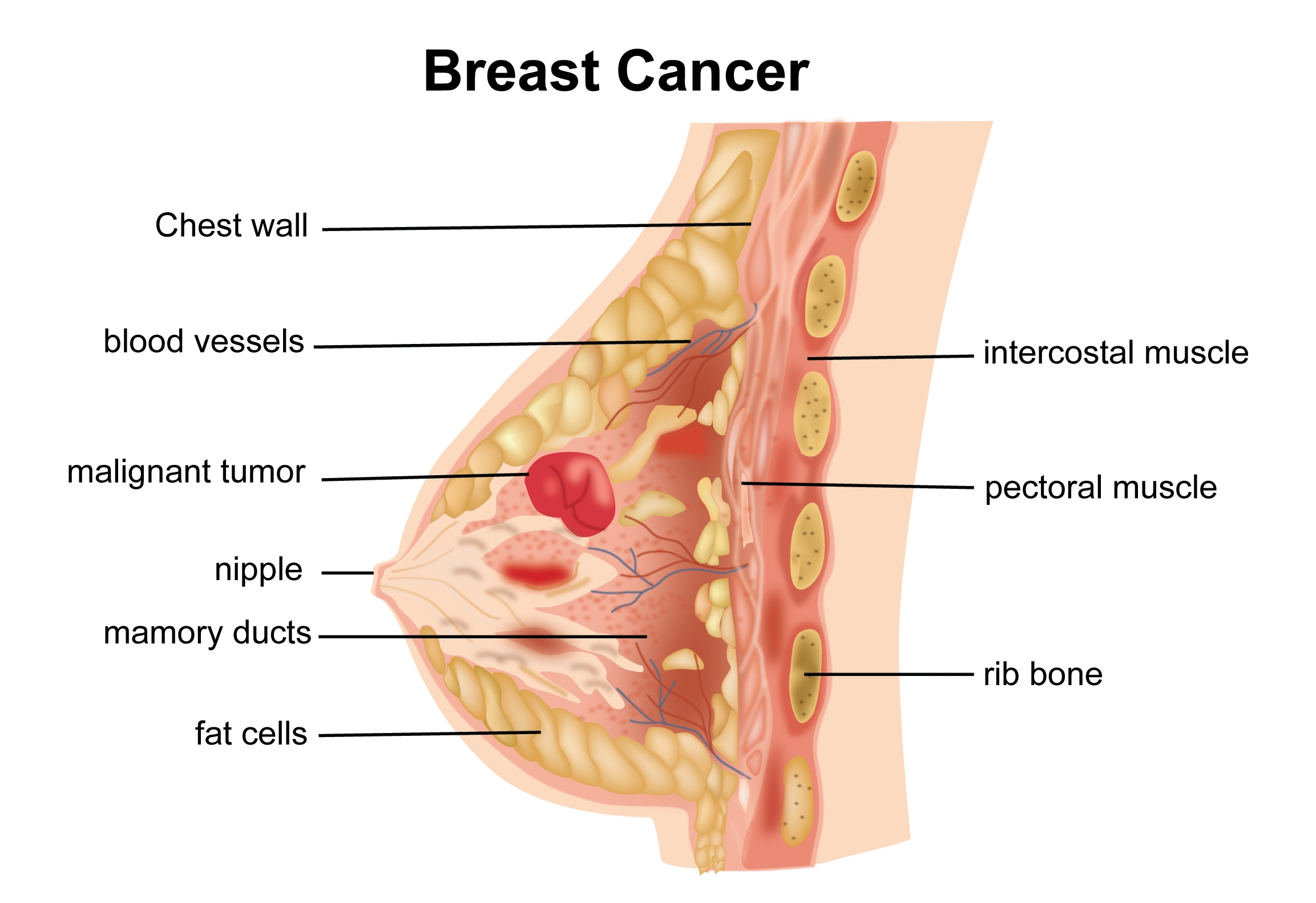

Breast cancer is cancer that has started in the breast tissue. When it starts from the lobules it is called as lobular carcinoma and from the ducts as ductal carcinoma. These types of cancers are called as invasive cancers. Non-invasive cancers of the breast include Ductal Carcinoma in situ (DCIS) and Lobular Carcinoma in situ (LCIS). Non-invasive cancers are so called because they do not have the capacity to invade other structures and spread to distant organs like invasive cancers.
According to Globocan data 2018, there were 1,62,468 new breast cancers diagnosed in India in 2018, making up 14% of all cancers.
There are different types of breast cancer. Here are the common types.
Ductal Carcinoma in situ (DCIS)
This is the earliest form of breast cancer. This is where there are cancer cells within the ducts but have not spread outside into the surrounding tissues. This is called as a pre-cancerous condition or a non-invasive cancer. It means, it has still not acquired the classical feature of a cancer, which is the capacity to spread to other structures. If left untreated, DCIS could develop into an invasive cancer in some patients over some years. DCIS is seen on a mammogram and therefore usually detected when breast screening is done.
Lobular Carcinoma In situ (LCIS)
This is another type of pre-cancerous condition where the abnormal cells are present in the lobules of the breast. It is a non-invasive condition but can develop into a breast cancer over some years.
Invasive Ductal Carcinoma
This is a breast cancer that has started in the ducts and has spread to the surrounding breast tissues outside the ducts. This is the commonest form of breast cancer and makes up 80% of all breast cancer.
Invasive ductal carcinoma can be divided into categories such as tubular, cribriform, medullary, mucinous, papillary or as no special type.
Invasive Lobular Carcinoma
This is breast cancer that has started in the lobules of the breast. It makes up about 10% of all breast cancers.
Inflammatory cancer of the Breast
This is an uncommon cancer of the breast where the cancer cells grow through the small lymph channels in the breast and on the skin surface. As a result the skin and breast can be red and swollen.
Inflammatory cancer can spread quickly and therefore prompt investigation and treatment are required.
Paget’s Disease of Breast
This is a condition where there is a scaly rash on the nipple. Women having this condition may have an underlying breast cancer.
Phyllodes Tumour of the Breast
This is another type of a breast condition which usually presents as a lump. A phyllodes tumour can range from being a benign condition to one that behaves like a cancer. Treatment is based on the type of phyllodes that is found after removal of the lump. Radiotherapy is given after surgery for tumours that behave like cancer.
There are several risk factors that are implicated in the development of Breast cancer.
Age
As with many cancers, the risk of getting breast cancer increases with increasing age. Over 70% of all breast cancers occur in women over the age of 55.
Genetic
Only about 5% of all breast cancers are hereditary. The remaining 95% occur spontaneously. Hereditary breast cancers tend to occur in younger women. If there is a strong family history of breast, ovarian or other cancers (three or more in close family), it is worth speaking to your Oncologist or a Geneticist for further testing. BRCA1 and BRCA2 are two genes, which if abnormal increases the risk of getting breast cancer and other cancers such as Ovarian, Colon, Pancreatic and thyroid cancers. Testing can be done for these abnormal genes if there is suspicion of hereditary cancer.
Family History
Women who have had first degree relatives (sister, mother, daughter) with breast cancer have a higher risk than others of developing Breast cancer.
Radiation to Chest before the age of 30
Having radiation treatment to the chest before the age of 30 increases the risk of developing breast cancer. This type of radiation therapy is used to help treat conditions such as Hodgkin’s Lymphoma.
Overweight and Obesity
Being overweight increases the risk of developing breast cancer especially after menopause. This also applies to women who already had treatment for breast cancer in the past.
Use of HRT
Use of current or recent Hormone replacement therapy increases the risk of getting breast cancer.
Alcohol and Smoking
Drinking alcohol and smoking increases the risk of developing breast cancer
Early menarche and late menopause
Women who started menstruating before the age of 12 and women go into menopause after the age of 55 have a higher risk of developing breast cancer.
Benign Breast conditions
Having certain benign (non-cancerous) breast conditions increases the risk of developing breast cancer. These benign conditions are ductal hyperplasia, papilloma, sclerosing adenosis and complex fibroadenomas. Also, having Lobular Carcinoma in situ (LCIS) increases the risk of breast cancer. LCIS is a pre-cancerous condition and is not a cancer as the name suggests.
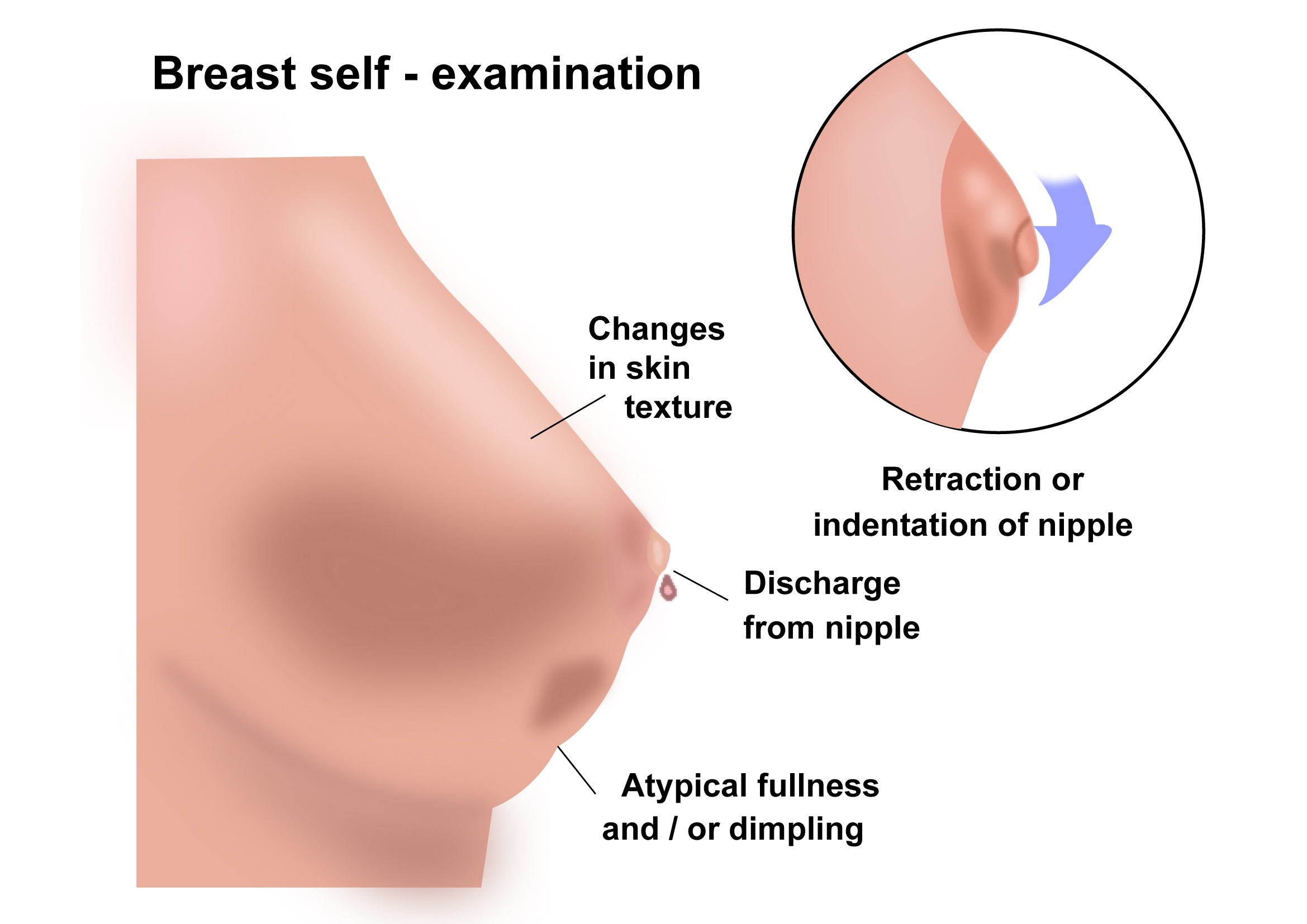
Breast cancers can have a range of symptoms. Early breast cancer may not produce any symptoms at all. As the cancer grows, the following symptoms can occur. Having any of these symptoms does not mean that there is cancer, but it is very important to be checked out by a doctor.
- A lump or thickening in the breast
- A discharge from the nipple
- Rash on the breast or nipple
- A nipple that has turned in
- Dimpling of the skin on the Breast
- Lump in the armpit
- A change in shape or size of the breast
Breast Lumps
A breast lump is a thickening or swelling in the breast.
Most breast lumps are benign (not cancer). They are usually fibroadenomas or breast cysts which can be left alone or treated easily. Infection, injury or trauma to the breast can also present as a lump.
It is strongly recommended to see a doctor if a breast lump is found.
Breast cancer is diagnosed after a clinical examination and investigations.
Clinical Examination
Clinical examination is done by a doctor. It involves a thorough examination of the breasts and areas under the arms(armpits). It also includes examination of other parts of the body such as neck, chest and abdomen. This examination can be done by a family doctor, breast surgeon or an Oncologist.
Initial Investigations
After examination, the doctor may request the following tests.
Mammogram
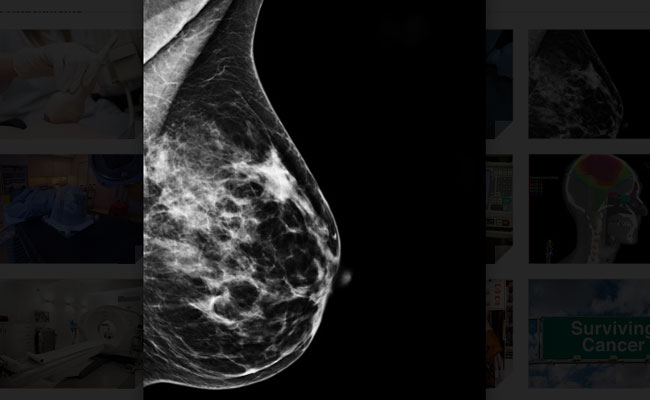

A mammogram is the commonest test used to detect breast conditions. It is a low dose x-ray of the breast. During the test, the breast tissue is compressed with a plate and two x-rays are taken in different angles. Mammograms can detect breast cancers even before a lump is felt. They are usually done in women over 40. Breast tissue is denser in younger women and therefore it makes it harder to get a good picture and see any changes.
Breast Ultrasound

An ultrasound scan of the breast uses sound waves to get a picture of the breast. This test is very good in telling if the breast lump contains liquid, like in a cyst, or is solid, containing cells. The scan is done by putting some gel on the breast and using a hand-held probe over it. The test takes a few minutes and is painless.
Breast MRI
MRI (Magnetic resonance Imaging) uses a strong magnet to get a detailed image of a part of the body. It does not use any x-rays. Breast MRI is used only in selected situations in the diagnosis of a breast cancer. It is not used as a routine test in everyone. It is mainly used in women who have extremely dense breasts, where a mammogram is unhelpful. It is also used in younger women who have an increased risk of breast cancer (BRCA1 and BRCA2).
Breast Biopsy
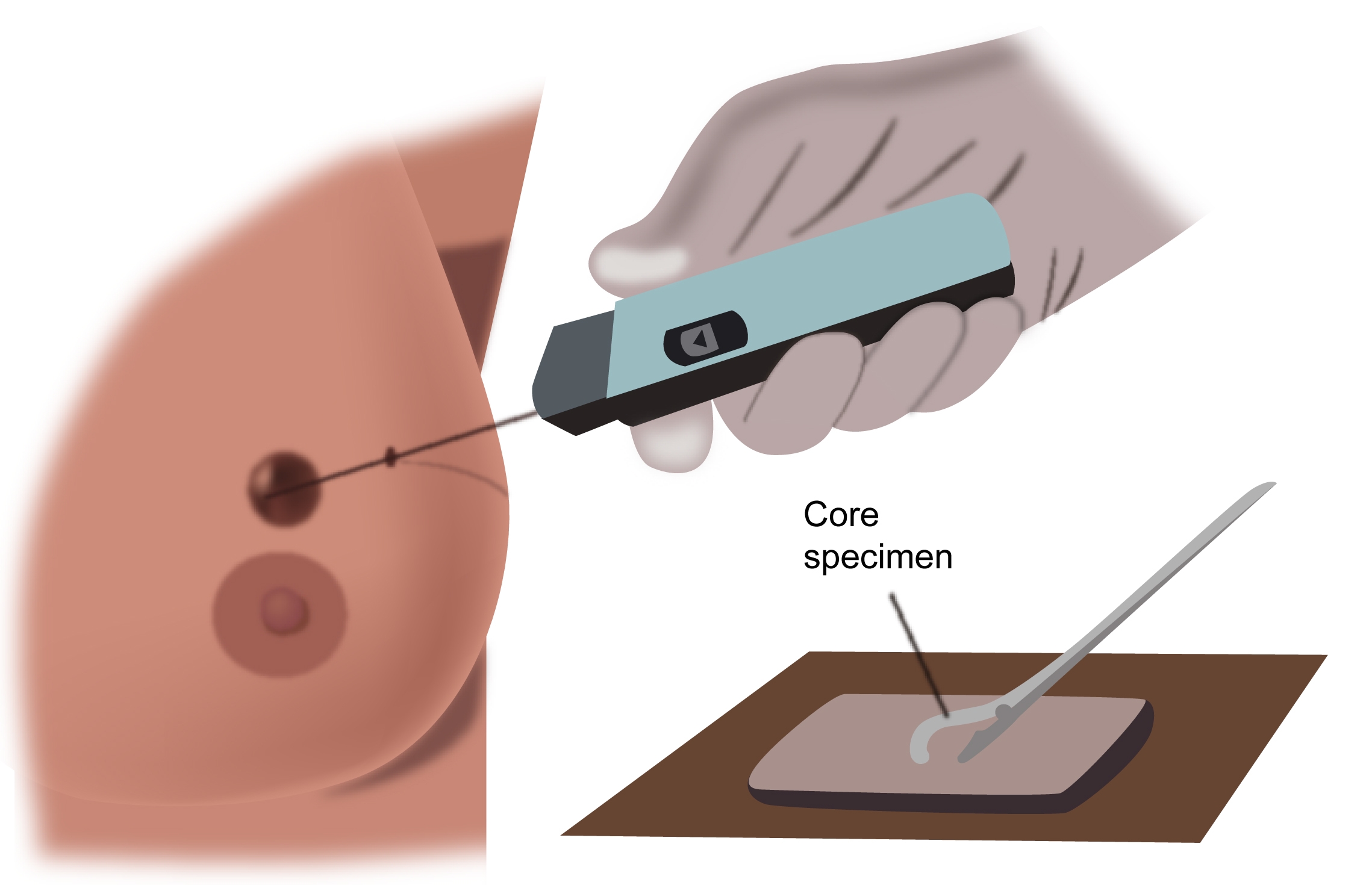
After the examination and initial investigations have raised a suspicion for cancer, the doctor will organize a biopsy of the abnormal area. A biopsy is a test where a piece of breast tissue is removed and looked under a microscope to establish a diagnosis. There are different ways as to how this can be done.
Fine Needle Aspiration Cytology (FNAC)
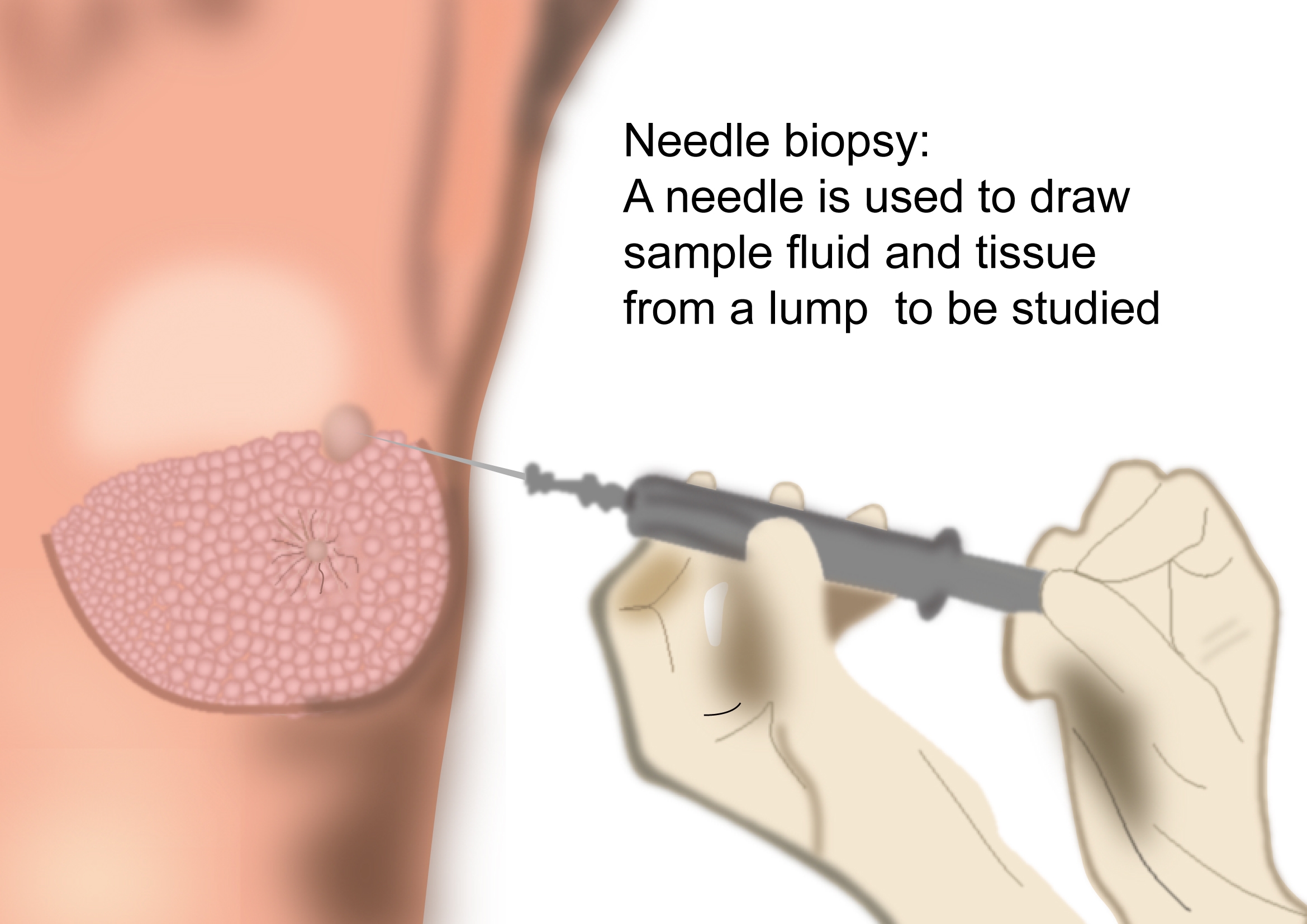
This is a test where a very small needle is inserted into the breast and individual cells or fluid is removed. Further testing is always required when cancer cells are seen to confirm the diagnosis or when a diagnosis cannot be made based on the sample taken.
Core Biopsy
This is a test where a large needle is used to take a bigger piece(core) of tissue. This is a more accurate method of diagnosis than FNAC. The cores can be taken under x-ray(stereotactic), ultrasound or MRI guidance. It is an out-patient procedure and is done under local anaesthesia. This is the standard form of test used in the diagnosis of breast cancer.
Surgical Biopsies
Surgical biopsies are when an incision is made in the breast. They can be excisional or incisional biopsies. This can be done under local or general anaesthesia.
Excisional biopsy
This is where the lump or tumour is completely removed. If the lump is small and cannot be felt, the excision can be done with the help of wire or needle guidance. These are put in prior to the procedure under ultrasound, x-ray or MRI guidance.
Incisional Biopsy
This is done where the mass is too large to remove without causing a deformity of the breast. Only a small piece of the mass is removed.
Diagnosis of Breast Cancer
A diagnosis of the breast cancer is made after the biopsy specimen is processed and looked at by the pathologist. The pathologist will do additional testing on the biopsy specimen to categorize the cancer better which will help guide further treatment. The following results will usually be seen on the pathology report.
Type of breast cancer:
Grade of cancer:
Grade 1 to 3 with grade 3 meaning a more aggressive cancer
Size of cancer:
Size is usually mentioned on the pathology report after removal of the cancer.
Margins:
The report after excision of cancer will tell if the margins around the operated cancer are clear. If margins are not clear, a re-excision may be needed.
ER and PR status:
The report will tell us whether the cancer is positive for Estrogen receptor (ER) or Progesterone Receptor (PR). If either of these is positive, then the patient will benefit from taking hormonal treatment.
HER 2 status:
The report will also tell whether the cancer is positive for HER 2 status. If it is positive, the patient will benefit from having treatment with drugs such Trastuzumab, Pertuzumab and other agents. Sometimes more testing is needed to clarify HER2 status.
Other Investigations
CT Scan
CT Scan or computed tomographic scan is a commonly used test for staging purposes once the cancer is diagnosed. It is done when the doctor feels there is a risk of spread of cancer to other parts of the body from the breast.
PET-CT scan
A PET CT Scan is a more specialised CT scan where the accuracy of picking up spread of cancer is higher. Your doctor may request this scan in some situations.
Bone Scan
An isotope bone scan is a staging scan used to look for spread of cancer into the bones.
It is done in patients when the doctor feels there is a risk of spread of cancer into the bones. Two types of bone scans can be done. One is a Technetium-99 scan which is cheaper and the other one is an F-18 bone scan which is more sensitive but also more expensive.
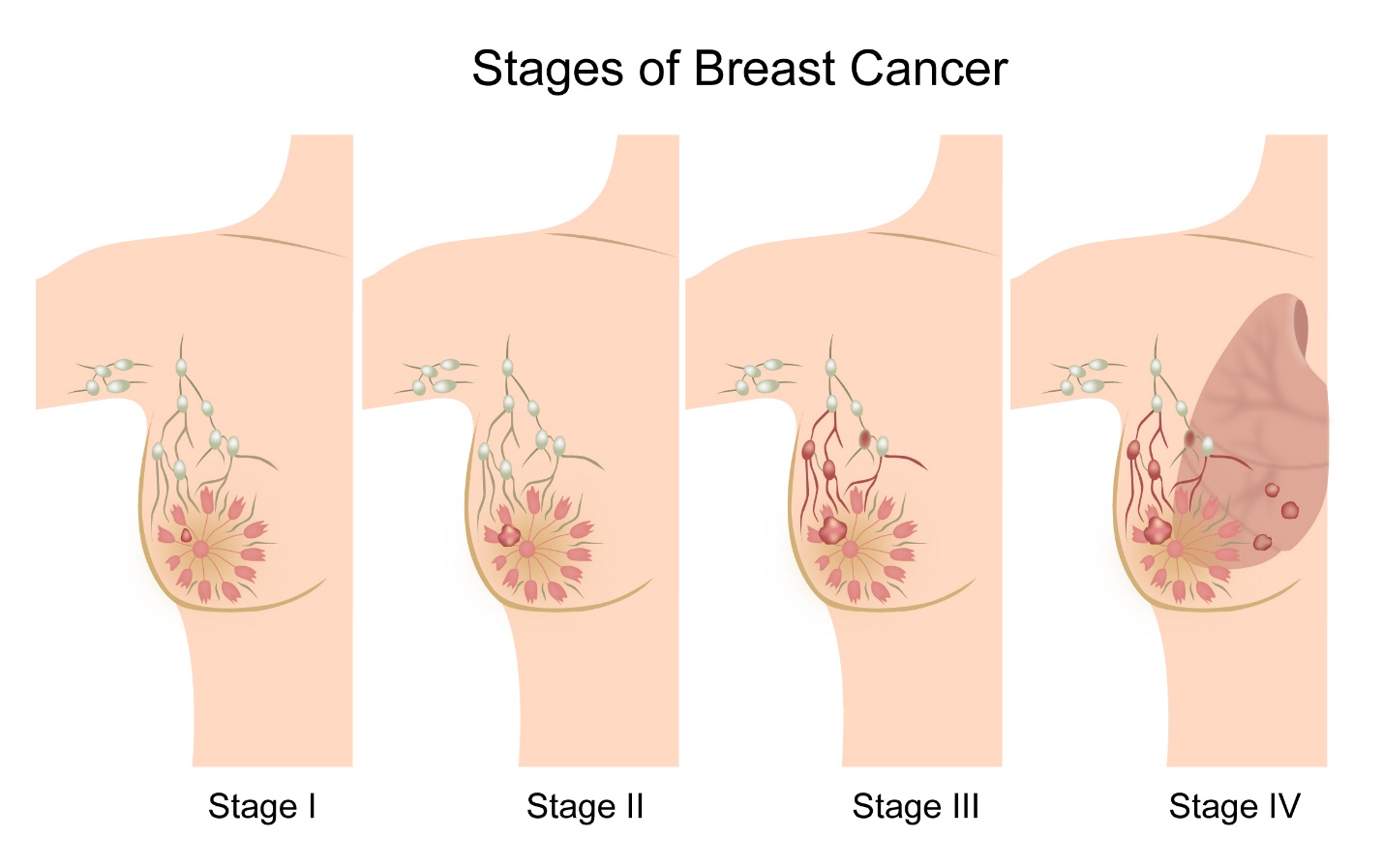
Breast cancer is staged based on the TNM staging system or the number system.
Staging with either system is based on the size of the tumour in the breast, the spread of the cancer locally in the breast and into the lymph nodes and spread of cancer into other parts of the body.
TNM Staging
TNM stands for tumour, node and metastases.
T Staging
T stands for tumour size. T is divided from T1 to T4
| T1 | The tumour size is 2cm in maximum diameter or less. T1 is further subdivided as follows |
| T1mi | The tumour is 0.1cm or less |
| T1a | The tumour is more than 0.1cm but not more than 0.5cm |
| T1b | The tumour is more than 0.5cm but not more than 1cm |
| T1c | The tumour is more than 1.0cm but not more than 2.0cm |
| T2 | The tumour is more than 2.0cm but not more than 5.0cm |
| T3 | The tumor is more than 5.0cm in diameter. |
| T4 | The T4 stage is subdivided into |
| T4a | The tumour has spread into the chest wall |
| T4b | The tumor has spread into the skin |
| T4c | The tumour has spread to both the chest wall and the skin |
| T4d | The cancer involves the skin making it red and swollen (Inflammatory Cancer) |
N Staging
| N0 | No cancer cells found in the lymph nodes |
| N1 | Cancer cells found in the lymph nodes that are movable |
| N2 | Cancer cells found in lymph nodes that are fixed to each other or to other structures |
| N3 | Cancer cells found in lymph nodes near the breast bone |
M Staging
| MX | Spread of cancer outside the breast and regional nodes cannot be assessed |
| M0 | No spread of cancer outside the breast or regional lymph nodes |
| M1 | Presence of cancer cells outside the breast or regional lymph nodes |
Number Staging
Stage 1
| Stage 1 | breast cancer can be subdivided into |
| Stage 1a | The cancer is 2.0cm or smaller and has not spread to the lymph nodes. |
| Stage 1b | The cancer is either 2.0cm or smaller and cancer cells are found in lymphnodes close to the breast |
Stage 2
| Stage 2 | can be subdivided into 2 groups |
| Stage 2a | The tumour is 2.0cm or smaller in the breast and cancer cells are foundin 1 to 3 lymph nodes in the armpit or near the breast bone OR The tumour in the breast is bigger than 2.0cm and not larger than 5.0cm and there is no cancers in the lymph nodes. |
| Stage 2b | The tumour is larger than 2 cm but not larger than 5 cm and cancer cells in 1 to 3 lymph nodes in the armpit only or to near the breast bone OR The tumour is larger than 5 cm and has not spread into the lymphnodes |
Stage 3 breast cancer
| Stage 3 | breast cancer is divided into 3 groups |
| Stage 3a | The tumour is not seen in the breast or tumour of any size is found and cancer cells found in 4-9 lymph lymph nodes in the armpit or near thebreast bone OR The tumour is larger than 5 cm and small groups of cancer cells seen in the lymph nodes OR The tumour is larger than 5 cm and has spread into up to 3 lymph nodes in the armpit Or in the lymph nodes near the breast bone |
| Stage 3b | The tumour has spread to the skin of the breast or the chest wall and made the skin ulcerate or swollen. There are cancer cells in up to 9 lymph nodes in the armpit or lymph nodes near the breast bone. |
| Stage 3c | The tumour can be of any size but there is cancer in the skin causing ulceration and swelling and it has spread to the chest wall. It has also spread to lymph nodes above or below the collarbone, lymph nodes in the armpit and near the breast bone or 10 or more lymph nodes in the armpit. |
Stage 4
In this stage, the tumour in the breast can be of any size, and there may or may not be cancer cells in the lymph nodes but the cancer has spread to other parts of the body like liver, lungs, bone or brain.
Surgery is done after diagnosis of breast cancer is made and is done to remove the cancer and involved regional lymph nodes. It is usually the first type of treatment for breast cancer. Sometimes, the surgeon may recommend the patient to have chemotherapy prior to surgery.
Surgery to remove the breast lump
Breast cancer surgery can be done in many ways. The general idea for surgery is to remove all known cancer and preserve as much normal tissue as possible. Based on this, different approaches are possible which are listed here below.
Wide local Excision
A wide local excision or a lumpectomy is a procedure where the cancer in the breast and a rim of normal tissue around it is removed. The remainder of the breast is left intact and not removed. This surgery is usually done under general anaesthesia but depending on need other methods can be used. Studies have shown that a lumpectomy followed by radiation therapy is as good as mastectomy.
Mastectomy
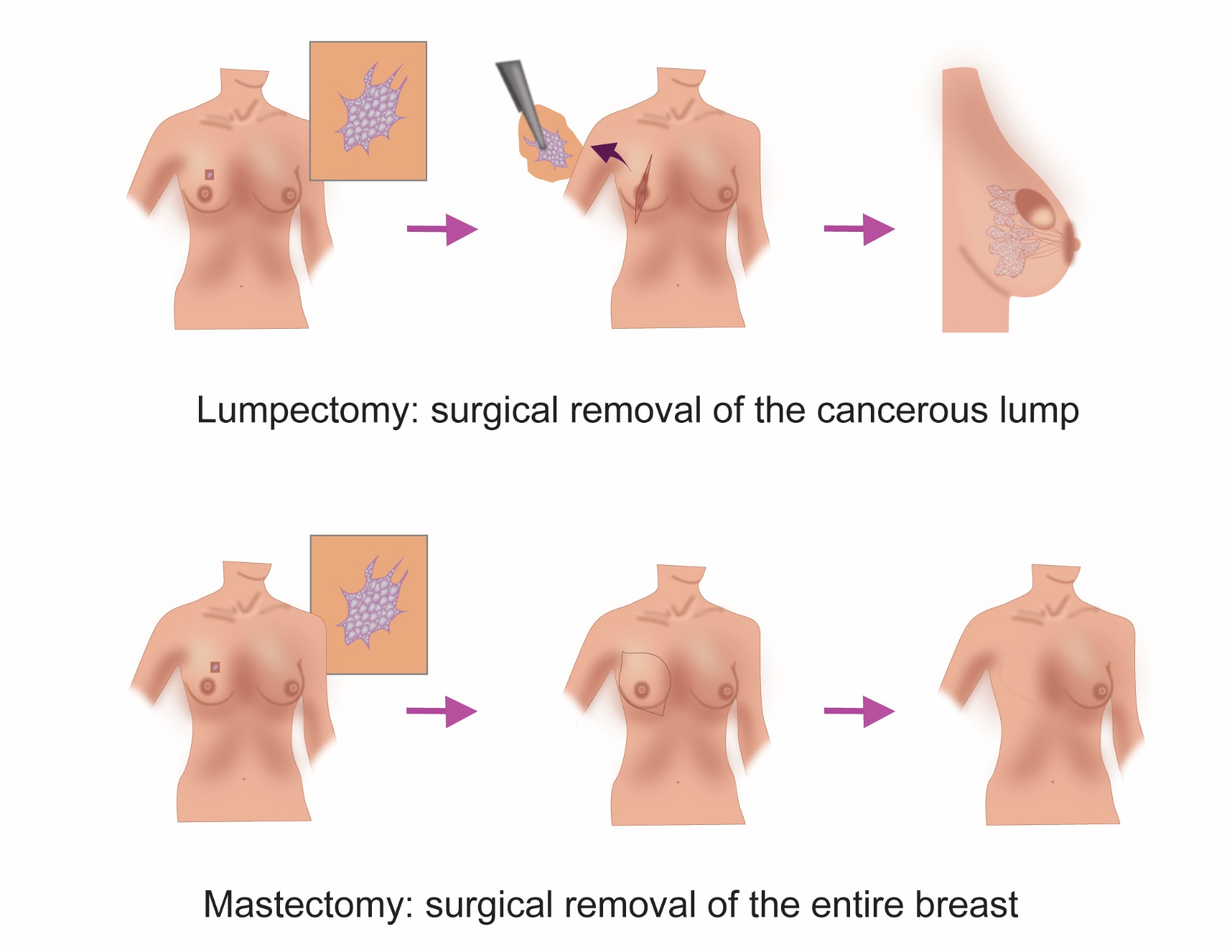
A mastectomy is a procedure where the entire breast is removed.
Mastectomy can be of many types.
A simple mastectomy is an operation where all the breast tissue and the skin covering the breast is removed.
A radical mastectomy is where the entire breast with the skin covering it, the two muscles underneath the breast and the lymph nodes in the axilla(armpit) are removed.
A modified radical mastectomy is like a radical mastectomy except that only one of the muscles is removed.
A skin sparing mastectomy is a procedure when all the breast tissue is removed but the skin on the breast is left behind. This is done when immediate breast reconstruction is being planned.
Which type of breast surgery should be done
The type of breast surgery to have depends on the tumour size and stage at diagnosis, the experience of the operating breast surgeon and personal choice of the patient.
Going for a wide local excision means that only the abnormal lump is removed, and the remaining normal breast is left behind. This procedure is appealing for a lot of women as the whole breast is not removed.
The operative scar is usually small and can become less noticeable over time. The cosmetic outcome of the procedure is quite good.
But by having a wide local excision, the patient will almost always need radiation treatment after the operation. Wide local excision is the most commonly practiced breast cancer operation in the western world. In India, mastectomy is more common.
A mastectomy as described above will remove the whole breast along with the tumour. In some circumstances, because of the size and location of the cancer, or type of cancer, a mastectomy may be the only option for the patient.
Following mastectomy, especially in early stage breast cancer, radiation may not be needed, and the treatment may be complete with a single operation. There is an option of going for an immediate or delayed breast reconstruction after mastectomy.
Lymph Node Surgery
When breast cancer spreads from its original site, it goes into the lymph nodes of the axilla(armpit).
Therefore, axillary lymph node surgery forms an important part of surgical treatment of Breast cancer. Axillary surgery is done in many ways.
Sentinel node Biopsy
Sentinel node is first node or nodes that the cancer can spread to. If there is no cancer in the sentinel node, then the chance of there being cancer in other axillary nodes is small.
A sentinel node is usually found in the axilla after injection of a small dose of radioactive substance or a blue dye into the area around the tumour in the breast. This dye is taken up by the first lymph node/s that the dye spreads to. These substances help the surgeon to locate the nodes at surgery.
The sentinel node biopsy is done at the same time as a wide local excision or mastectomy.
These removed nodes are then examined under the microscope for cancer cells. If there are no cancer cells, there is no further need for axillary surgery. However, if cancer cells are found, then the surgeon may decide to remove all other axillary lymph nodes or consider radiation treatment to the axilla.
Axillary Clearance
Axillary clearance is removal of all lymph nodes in the axilla(armpit). This is done when the sentinel node contains cancer cells or when a sentinel node procedure is not done, and axillary surgery is done along with removal of primary tumour from the breast. Axillary clearance is part of any radical mastectomy procedure. When an axillary clearance is done, on average about 10 to 20 lymph nodes are removed.
After effects of Breast Surgery
Breast Cancer surgery is very commonly done and is a safe procedure. Like all treatments, there are some common after effects associated with this type of surgery, which are listed below.
Seroma collection
This is collection of a small amount of fluid underneath the surgical scar. Normally, a tube is placed after the operation to drain this fluid. Sometimes, fluid may collect after the drain is taken out. This fluid can be taken out easily with the help of a needle and syringe.
Numbness
It is common to feel a numbness under the arm(armpit) and over the shoulder after axillary surgery. This sensation changes over time and can last for many years after surgery. This is a normal effect of surgery and having it doesn’t mean that something went wrong with the procedure.
Lymphoedema
This is swelling of the arm, forearm or hand on the side of the operation. This can happen days to weeks after the operation is done. This is because of the removal of lymph nodes under the armpit. This is a common side effect of breast and axillary surgery, particularly after axillary clearance and can happen to varying extent in up to 25% of patients. Massage and physiotherapy techniques will help reduce the swelling.
Infection
This is a potential side effect of any surgical procedure and can be managed well with appropriate treatment and antibiotics.
Pain or stiffness in the shoulder
Following axillary surgery or a mastectomy, the patient may feel stiffness or pain in the shoulder. It is important to do the arm exercises regularly to help reduce stiffness in the shoulder after surgery. These exercises can be taught to you by the surgeon or a physiotherapist.
Breast Reconstruction
Breast reconstruction is surgery done after mastectomy to reconstruct a new breast shape that matches the breast on the other side.
Reconstruction can be done at the same time as a mastectomy (immediate reconstruction) or can be done at a later period (delayed reconstruction).
Reconstruction can be done by using a breast implant or by using tissue from another part of the body.
Breast reconstruction needs more than one operation usually.
The advantages of immediate reconstruction are there is less scarring, less time period without a breast shape and usually has a better appearance than other types. The disadvantages are that radiation treatment after reconstruction may affect the shape of the reconstructed breast.
The advantages of delayed reconstruction are that the patient has more time to think about whether to go for such a surgery and the patient can finish all their cancer treatments first and then go for reconstruction. The disadvantage of delayed reconstruction is that the patient will have another operation and another anaesthetic for that operation.
Nipple reconstruction is also needed to match the appearance of the other breast. This is usually done at a separate operation some months after the primary reconstruction. Tattooing of the areola is done to match the colour of the other nipple and areola.
Types of Breast Reconstruction
Breast reconstruction surgery can be done by different techniques.
Prosthetic reconstruction involves placing an implant in the place of the breast at the time of removal of the breast. A tissue expander is placed sometimes soon after mastectomy to help expand the space left behind after surgery. A permanent reconstruction procedure is done at a later time.
The other method of reconstruction used is where tissues from other parts of the body are placed in the area where the breast was. Common types of such techniques involve using of flaps (tissue removed from elsewhere).
A TRAM flap is removal of tissue from the lower part of the abdomen and used to reconstruct the breast. A DIEP flap also involves removal of tissue from the lower abdomen but the rectus abdominis muscle is not removed as in a TRAM flap.
An LD flap is one where the tissue is removed from the Latissimus dorsi muscle on the back of the chest and swung forwards to reconstruct the breast.
Breast Prosthesis
Following a mastectomy, a woman can wear a breast prosthesis on that side without having any further reconstructive surgery. This is a false breast that is made of silicone and is worn under the bra. It can match the shape and size of the breast on the other side. Some women prefer to use a prosthesis rather than going for a reconstruction.
Chemotherapy
Chemotherapy is use of anti cancer drugs given in the form of injections, drips and tablets. These drugs help kill cancer cells by causing maximum damage to them and at the same time causing some damage to normal tissues. The side effects that happen as a result of chemotherapy are due to the effect of the drugs on normal tissues. A number of chemotherapy drugs used to treat cancer. These drugs can be used either in combination or as single agents. Chemotherapy is given as cycles, with each cycle lasting between 1 to 4 weeks, usually 3 weeks. The gap between two chemotherapy cycles is for the body to recover before the next dose. A course of chemotherapy usually lasts for some months.
Chemotherapy for breast cancer
Chemotherapy plays an important role in the treatment of patients with breast cancer. It can be given at different stages in the breast Cancer treatment pathway. Chemotherapy is given alongside biological therapy in some settings in breast cancer. See section on biological therapy for more information.
Adjuvant chemotherapy
Adjuvant chemotherapy is when chemotherapy drugs are given following surgery, after the cancer has been completely removed. The purpose of adjuvant chemotherapy is to reduce the risk of cancer coming back.
Not all patients who have their breast cancer removed need chemotherapy. The need is based on the type and stage of the cancer at diagnosis, and by that, the risk of recurrence is assessed. A medical oncologist will be able to discuss the risks of recurrence of cancer and explain the pros and cons of having adjuvant chemotherapy.
Adjuvant chemotherapy for breast cancer can be given with different combinations of chemotherapy drugs. The selection of the ideal combination is based on the stage of cancer at diagnosis and the general condition of the patient. Here are a few combinations that are commonly used.
- FAC-Fluorouracil, Doxorubicin, Cyclofosfamide
- FEC-Fluorouracil, Epirubicin, Cyclofosfamide
- AC-Doxorubicin and Cyclofosfamide
- TC-Docetaxel and Cyclofosfamide
- FAC-T-Fluorouracil, Doxorubicin, Cyclofosfamide and Docetaxel or Paclitaxel
- FEC-T-Fluorouracil, Epirubicin, Cyclofosfamide, and Docetaxel or Paclitaxel
- FEC-TC-Fluorouracil, Epirubicin, Cyclofosfamide, Taxane and Carboplatin
Neoadjuvant chemotherapy
In some breast cancers, chemotherapy is given prior to surgery to reduce the size of the primary tumour. This is called as neoadjuvant chemotherapy. This is commonly done in patients where the tumour is large and breast conserving surgery is not possible. By having neoadjuvant chemotherapy, the tumour size can be reduced and the patient may then be suitable for a wide local excision. It is also considered in patients who are hormone receptor negative or HER2 positive.
The chemotherapy regimens that are used in the adjuvant setting are also used in this setting.
Is chemotherapy given to all patients with Breast Cancer?
The need to have chemotherapy before or after breast cancer surgery, is not present in all patients but is considered and given to those where there is a sufficient benefit from receiving it. There are various tools and methods that are used to say whether one would benefit from having such treatment.
Factors that are important in determining the benefit of chemotherapy include age-younger age has more benefit, size of tumour- the larger the size the more benefit, involvement of lymph nodes with cancer, ER positive or negative-ER negative patients have more benefit, HER2 positive-patients have more benefit from chemotherapy etc.
There are tools and tests available in the market which can estimate the percentage benefit of having chemotherapy in each patient and these are briefly listed below.
Online Tools
Predict version 2.0- This is an online tool developed in the UK and used all over the world to predict the benefit of adjuvant chemotherapy in breast cancer.
Other Tests
- EndoPredict (Myriad Genetics)
- Oncotype DX (Genomic Health)
- MammaPrint (Agendia)
- Prosigna (NanoString Technologies)
These above tests can help to make a decision about the benefits of taking chemotherapy by predicting a risk of recurrence of cancer and the additional benefit the chemotherapy gives in reducing that risk. These tests are expensive but can be useful in certain circumstances to help in the decision making process.
Side effects of chemotherapy
Chemotherapy for breast cancer is associated with side effects. These depend on the drugs that are administered. Some of these side effects can be well controlled with medications. Tolerability of chemotherapy varies from person to person. Some people cope with treatment very well without any side effects, while other may have side effects. common side effects are
Hair loss
This is common with the above mentioned chemotherapy regimens. Hair loss usually starts after the second week of the first cycle. Hair re grows back after chemotherapy is finished. Some centres may offer a “cold cap” service which can reduce the chance of hair loss. A “cold cap” is a very cold cap that is put on the head during administration of chemotherapy.
Nausea and vomiting
This is a well-known side effect of chemotherapy, but with modern medications, these symptoms are very well controlled. Nausea is the sensation of feeling like vomiting.
Tiredness
Tiredness is a common side effect. It is usually more in the first week and then gradually improves after that.
Soreness in the mouth
This is common after chemotherapy and will settle by itself.
Loose Motions
This symptom can occasionally occur after chemotherapy.
Constipation
Constipation is a common side effect of chemotherapy. This can happen as a result of the chemotherapy drug itself but mainly it is due to the effect of the anti nausea drugs that are given along with chemotherapy. Constipation happens in the first few days of chemotherapy.
Risk of Infection
This is an important side effect of chemotherapy. It happens as chemotherapy reduces the capacity of the body to fight infections. Therefore, it is very important to contact your doctor urgently if you have a fever at any time (even if it is in the middle of the night) during chemotherapy.
Taste changes
This is common with chemotherapy and therefore food wont taste as before. Taste will recover after chemotherapy is finished.
Tingling in Hands and feet
Some chemotherapy drugs produce this side effect.
Anaemia
This can happen as a result of chemotherapy. Usually this can just be observed, and it will improve after treatment finishes. Sometimes blood transfusion or other treatment is necessary to improve it.
Bleeding
There is a small risk of bleeding with chemotherapy. If this happens, you need to contact your doctor straight away.
Fertility and Menopause
Chemotherapy can affect the function of the ovaries in the body leading to a menopause. This cause reduced or stoppage of periods completely. In young women, the periods may restart after completion of chemotherapy, but in older women the periods may not start at all. This side effect of chemotherapy can affect the ability of the woman to have children in the future.
For chemotherapy in metastatic or secondary breast cancer, see section on secondary breast cancer.
Radiotherapy
Radiotherapy is the use of high energy x-rays given to kill cancer cells. These x-rays cause damage to the DNA of the cancer cells and thereby kill them. Radiotherapy is a local treatment and has its effect in the area that it is given to. It is given using a large machine (Linear accelerator) which generates the x-rays and delivers the treatment to the patient. This method is called as external beam therapy. The other way to give radiotherapy is to insert radioactive sources into the cancer itself. This method is called Brachytherapy and is used to treat some types of cancers.
Radiotherapy for Breast Cancer
Radiotherapy for breast cancer is done usually after the breast lump is removed. The purpose of radiotherapy here is to reduce the risk of recurrence of cancer in that breast. Majority of patients who have a wide local excision will need radiotherapy. Only a proportion of patients who have a mastectomy will need radiotherapy. External beam radiotherapy is the most common mode of treatment. Here the whole breast, or chest wall in case of mastectomy, is treated. The axilla (arm pit) may also need to be treated depending on the stage of cancer.
The treatment is given five days a week and can last up to three to five weeks in total. On each day, the treatment takes about 15 minutes. It is completely painless and very similar to having an x-ray. The duration of radiotherapy in breast cancer can last from 3 to 6 weeks depending on the method of treatment chosen by the Oncologist. There will be some side effects by the end of treatment which are listed below.
Brachytherapy in Breast Cancer
Brachytherapy, where a radioactive source is used to give radiotherapy is used to treat breast cancer. This treatment is done in patients who have had a lumpectomy where the cancer is removed and the breast remains in place. The brachytherapy source is put in the lumpectomy cavity and treatment is given. This method is quicker than traditional radiotherapy and is available in some centres. This type of treatment is called as intracavitary brachytherapy.
Intraoperative Radiotherapy
This is a technique where the radiotherapy is given at the time of the lumpectomy using a special type of radiotherapy machine that is small and portable.
Stages of Breast or Chest wall Radiotherapy
The Radiation Oncologist will discuss all the pros and cons of treatment. You will then be taken into a planning simulator or a CT scan room. If the centre has a planning simulator, you will have some x-rays taken and marks put around the breast or chest wall. If the centre has a CT scan, a scan of the chest is done after which marks on placed. These help the radiographers to line up the patient in exactly the same position every day of the treatment.
Following this, the Oncologist outlines the area that needs treatment and the physicist plans as to how best to deliver this treatment. The aim of all these procedures is to be very precise, to cause maximum damage to the cancer cells, and avoid radiation to normal structures as much as possible.
Side effects of Breast or Chest wall Radiotherapy
The side effects of breast or chest wall radiotherapy are
Skin changes
The skin on the breast or chest wall can become dry, red and itchy with radiotherapy. Towards the end of treatment, the skin can become flaky, or sometimes the skin can peel leaving a raw area beneath. These skin side effects will peak one week after the treatment is complete and will resolve in two weeks after that. To prevent dryness and itchiness, it is advisable to apply simple moisturizing cream. Do not apply any creams with metals in it(zinc etc) as this can make skin reaction worse. Do not rub the skin vigorously during treatment as this can worsen side effects. Just mop gently with a soft cloth. If skin peels leaving a raw area, speak to your oncologist for special creams and dressings.
Tiredness
Radiotherapy can cause some tiredness towards the end of treatment. This can be partly due to treatment and partly due to travel to and from the hospital for five weeks. Tiredness will settle down in a few weeks.
Pain in the breast or on the chest wall
This can happen at the end of treatment. It is often very mild and doesn’t need any medications. It will settle in a few weeks. A very small group of patients may experience pain for longer needing pain killers to control it.
Swelling in the breast
Some patients can experience swelling of the skin on the breast long after radiotherapy is complete. This is called lymphoedema. It is usually mild and doesn’t cause any significant discomfort.
Swelling of the Arm
For patients who have axillary surgery followed by radiotherapy to the axilla, there is a risk of swelling of the arm. This is called lymphoedema of the arm. It usually settles over a period of many weeks and if it doesn’t settle, it can be managed with gentle massage, exercises and compression bandages.
Firmness of Breast
In the months to years after radiotherapy, the treated breast may feel firmer than the other breast. A small group of patients may notice the treated breast to become slightly smaller than the other breast.
Cough and Breathlessness
Some patients who have breast or chest wall radiotherapy can develop cough and breathlessness as a side effect of treatment. This is usually mild and settles down.
For radiotherapy in secondary or metastatic breast cancer, see section on secondary breast cancer
Hormonal treatment in breast Cancer is the use of drugs usually given in the form of tablets or injections, which help reduce the effect of Oestrogen on the cancer cells. In 80% of breast cancers, the cancer cells tend to grow with the help of Oestrogen that is naturally produced in the body. These hormonal agents either block the effect of Oestrogen on cancer or reduce the production of Oestrogen in the body. By doing so, this treatment reduces the risk of recurrence of cancer after primary surgery or control the cancer that is present.
Who needs hormonal treatment
When a breast cancer is diagnosed with a biopsy, the biopsy sample is tested for the presence of oestrogen receptor and progesterone receptor. If either of these are positive, the patient will benefit from taking hormonal treatment. About 80% of all breast cancers are oestrogen receptor positive and therefore will benefit from hormonal treatment.
Types of Hormonal Treatment
The type of hormonal treatment to take depends on whether patient is pre-menopausal or postmenopausal. This is because some hormonal treatments do not work in premenopausal women.
Premenopausal (women having periods)
Tamoxifen is a commonly used drug in women having their normal periods. It helps to reduce the risk of recurrence of the cancer and is strongly recommended to be taken in premenopausal women who have had their cancer removed by surgery. This drug is given in the form of a tablet. It is taken once daily at a dose of 20 mg. Tamoxifen is generally very well tolerated with minimal side effects. It is very cheap. In some premenopausal women with advanced cancer, the doctor may offer the option of giving injections to stop periods (Ovarian ablation) and make the patient postmenopausal. These injections are called as LHRH analogues. After that medications such as Anastrazole and Letrozole can be used. Suppression of ovarian function can also be achieved by surgery where the ovaries are removed or use of Radiotherapy to the ovaries.
Postmenopausal
In postmenopausal women (whose periods have stopped) there is a wide choice as to which hormonal agent to use. The options are either to take Tamoxifen or other drugs such as Anastrozole, Letrozole or Exemestane.
Anastrozole and Letrozole are called Aromatase Inhibitors and work better than Tamoxifen in the postmenopausal setting. They are not useful in premenopausal women. They are well tolerated.
When Aromatase Inhibitors are given over a prolonged period, it is important to monitor the patient’s bone health. This is because these drugs can cause thinning of the bones (osteoporosis). It is also advisable to take calcium and vitamin D tablets along with these medications.
Timing of Hormonal Therapy
Hormonal therapy should be used after completion of primary surgery when the cancer is removed. If the patient is having chemotherapy, then this treatment should be used only after completion of chemotherapy. It should not be used at the same time as chemotherapy. However, it can be used at the same time as radiotherapy.
Sometimes, hormonal treatment can be used prior to surgery to reduce the size of the cancer. Hormone therapy can also be used in secondary or metastatic cancer. See section on Secondary breast cancer for more information regarding that.
Duration of Hormonal Treatment
In a premenopausal woman, Tamoxifen should be taken for at least 5 years and maybe up to 10 years. In post-menopausal women who take Tamoxifen, it could be used for 5 years after which the patient could switch to an Aromatase Inhibitor. Speak to your doctor regarding the pros and cons of that.
In a post menopausal woman who starts with an Aromatase Inhibitor, it should be taken for 10 years based on current literature.
Side effects of hormonal treatment
The side effects of hormonal treatment are usually mild. They are in the form of mild sweating, hot flushes at night, weight gain, thinning of the hair, aches and pains in muscles and joints.
While on tamoxifen, it is important to see a doctor if there is any sign of vaginal bleeding.
As mentioned above, there is a small risk of osteoporosis with Aromatase inhibitors and therefore the bone health should be monitored with the help of bone density scans on a regular basis. Overall, the side effects from these drugs are very small and the benefits of the treatment clearly outweigh the risks.
Other Hormonal Agents and treatments
Other hormonal agents such as Faslodex are used in patients with metastatic breast cancer when the above hormonal treatments do not work. Faslodex is given in the form of injections once a month.
CDK 4/6 Inhibitors
These are drugs that can be used along with hormonal therapies such as Letrozole and Anastrazole for treatment of metastatic breast cancers. These drugs include Palbociclib, Ribociclib, Abemaciclib. When given in this combination, the response rate and the duration of response of the cancer is better than when hormonal agents are used alone.
mTOR Inhibitors
These drugs such as Everolimus are used when combined with an Aromatase Inhibitor such as Exemestane for treatment of metastatic breast cancer.
Biological Therapy
Biological therapy includes use of drugs such as monoclonal antibodies and other targeted therapies.
These drugs are given either as tablets or as intravenous infusions. The drugs typically target certain specific areas on the cancer cell, thereby helping in cancer reduction and shrinkage.
As these drugs target specific types of cells only, the side effects of these drugs are much less than those of chemotherapy. These drugs are used to control some types of cancers.
Biological Therapy for Breast Cancer
There are four main types of biological drugs available for use in breast cancer and these are listed here below.
Her2 positive Cancers
Her2 is an epidermal growth factor receptor 2, which when amplified in a breast cancer can lead to increase of the cancer making it more aggressive than a breast cancer that is HER2 negative. About 20% of all breast cancers are HER2 positive and this should always be tested for at the diagnosis of the cancer. The HER2 status is tested on the cancer specimen that is got on biopsy or at surgery. Sometimes the initial HER2 test is equivocal, when a further test (FISH) is required.
If HER2 test is positive, antibodies against the HER2 receptor are available and used as treatment for this type of cancer. The following drugs are used in this setting.
Trastuzumab
This is a drug that is commonly used in breast cancer. This drug can be used in the adjuvant setting (after breast cancer surgery) or in the metastatic setting when the cancer has spread to different parts of the body. The drug is used on its own or combined with Pertuzumab or chemotherapy.
When given in the adjuvant setting, Trastuzumab is given for a period of one year. It can be given either once weekly or once every three weeks at a higher dose. In metastatic disease, the drug is continued for as long as it works.
Pertuzumab
This is another Her2 receptor monoclonal antibody that is given along with Trastuzumab in patients with advanced or metastatic cancer and as part of neoadjuvant (before surgery) and adjuvant chemotherapy (after surgery).
Ado-trastuzumab emtansine (TDM-1)
This is a drug which is a combination of trastuzumab and chemotherapy and is used in metastatic breast cancer patients who are HER2 positive and have previously used Trastuzumab.
Lapatinib
This drug is also used in patients whose cancer tests positive for HER2. Lapatinib is given to patients who previously had Trastuzumab treatment. It can be given as a combination with chemotherapy agents or Trastuzumab or on its own. This is an oral medication.
Side Effects of anti HER2 Drugs
These drugs are generally well tolerated except for specific side effects which should be monitored closely. The function of the heart should be monitored using an Echocardiogram every 3 months as these drugs can affect the function of the heart. Any symptoms such as cough, breathlessness, swelling of feet should alert the patient.
mTOR Inhibitors
Everolimus
This drug is used in combination with hormone therapy called Exemestane for treatment of secondary breast cancer. These drugs block the mTOR pathway that the cancer can use to grow.
CDK 4/6 Inhibitors
These are drugs that can be used along with hormonal therapies such as Letrozole and Anastrazole for treatment of metastatic breast cancers. These drugs include Palbociclib, Ribociclib, Abemaciclib. When given in this combination, the response rate and the duration of response of the cancer is better than when hormonal agents are used alone. These drugs are in the tablet form and usually well tolerated by the patients with limited side effects.
PARP Inhibitors
These drugs such as Olaparib, Rucaparib, Talazoparib, Niraparib and Veliparib are useful to treat metastatic breast cancer in patients with BRCA1 and BRCA2 mutations. These are genetic mutations which increase the risk of breast and ovarian cancers.Patients with metastatic breast cancer who have BRCA mutations may benefit from drugs called PARP inhibitors such as Olaparib.
Secondary cancer or Metastatic Cancer
Secondary cancer is cancer that has spread to other parts of the body from its original site. Secondary cancer can also be cancer that has come back after the primary cancer has been treated.
Secondary breast cancer
Secondary breast cancer is cancer that has spread to other parts of the body from the breast. Secondary breast cancer can also be cancer that has come back after the primary breast cancer and the axillary lymph nodes have been treated.
Symptoms of secondary breast cancer
Because secondary breast cancer can appear in any part of the body, the symptoms it produces can be very varied. Following treatment for cancer it is important to notify your doctor of any unusual symptoms which you had not experienced before or common symptoms such as cough etc which are not settling as they should do.
Diagnosis of secondary breast cancer
Following treatment of the primary breast cancer, it is important to be regularly seen and examined by the oncologist. The oncologist may also request routine tests and scans during this follow up process. It is in these tests and scans that secondary cancer can be picked up. Sometimes, the patient presents with symptoms which then leads to investigations and diagnosis of secondaries.
Treatment of secondary breast cancer
The treatment of secondary breast cancer largely depends on the location of the secondaries, the symptoms of the patient, the general physical condition of the patient and hormonal and HER2 status of the patient. Based on these, various options of treatment and available, which are listed below. Once, secondary breast cancer is diagnosed, all treatment options are mainly aimed at controlling the cancer.
Chemotherapy
Chemotherapy is a commonly used treatment in secondary breast cancer. There are a number of chemotherapy options that are available which can be used. These chemotherapy drugs are given as drips, injections or tablets. These drugs can be given individually or as combinations.
The medical oncologist will decide upon which of these drugs to use. The aim is to give maximum benefit with minimal toxicity. Here are the common drugs used to treat secondary breast cancer.
- Taxanes-(Docetaxel, Paclitaxel, nab-Paclitaxel)
- Anthracyclines-(Doxorubicin, Epirubicin, Liposomal Doxorubicin)
- Capecitabine
- Gemcitabine
- Vinorelbine
- Eribulin
- Ixabepilone
- Carboplatin
Radiation Therapy or Radiotherapy
Radiation treatment is very commonly used in management of symptoms of secondary breast cancer. It is a local treatment, where radiation is targeted to a specified area in the body. Radiation treatment is particularly good in controlling symptoms such as pain. Commonly, areas of cancer in the breast, brain, bones such as spine, ribs and other areas are treated with radiotherapy. Radiotherapy can be quite effective in reducing symptoms. A typical treatment lasts 1-10 days.
Hormonal treatment
If the breast cancer is oestrogen receptor positive or progesterone receptor positive, then hormone therapy is used. Most breast cancer patients would have already used some form of hormonal treatment prior to the development of a secondary cancer. There are many hormonal treatments available which can be used. The medical oncologist will decide on the most appropriate hormone treatment. Hormonal treatment is not effective if the tumour is oestrogen receptor negative and progesterone receptor negative. In the setting of secondary breast cancer, these hormonal agents are continued until there is further increase in the disease. The agents that are used are
- Tamoxifen
- Anastrozole
- Letrozole
- Exemestane
- Fulvestrant
- Progestins
Biological treatments
Biological agents are available in the treatment of patients with secondary or metastatic breast cancer. These agents are not chemotherapy drugs and therefore the toxicity is comparatively mild.
Trastuzumab
This drug is used in patients whose cancer shows HER2 positivity on testing. This test is done on the breast cancer sample that was taken to diagnose the condition. If such sample is not present or the test was not done at diagnosis, then a repeat biopsy is needed to test for HER2 status.
If the HER2 test is positive, Trastuzumab will be beneficial. Otherwise it is of no benefit. About 20% of all breast cancer patients will test positive for HER2. Trastuzumab can be given on its own or combined with chemotherapy.
Pertuzumab
Pertuzumab is another drug used in the treatment of secondary or metastatic breast cancer in patients whose cancers are HER2 positive. It is used as a combination with Trastuzumab and/or chemotherapy.
Ado-trastuzumab emtansine (TDM-1)
This is a drug which is a combination of trastuzumab and chemotherapy and is used in metastatic breast cancer patients who are HER2 positive and have previously used Trastuzumab and Lapatinib.
Lapatinib
This drug is also used in patients whose cancer tests positive for HER2. Lapatinib is given to patients who previously had Trastuzumab treatment and the cancer increased despite its treatment. It can also be given as a combination with chemotherapy agents or Trastuzumab or on its own.
Everolimus
This drug is used in combination with exemestane for treatment of secondary breast cancer.
CDK 4/6 Inhibitors
These are drugs that can be used along with hormonal therapies such as Letrozole, Anastrazole and Fulvestrant for treatment of metastatic breast cancers. These drugs include Palbociclib, Ribociclib, Abemaciclib. When given in this combination, the response rate and the duration of response of the cancer is better than when hormonal agents are used alone. These drugs are in the tablet form and usually well tolerated by the patients with limited side effects.
Other Drugs
Fam-trastuzumab deruxtecan is an antibody drug combination compound now available for treatment of metastatic HER 2 positive breast cancer. Tucatinib, an oral treatment can also be considered along with other drugs.
Immunotherapy can be used as an option of treatment in breast cancer patients who have metastatic disease are known to be triple negative, ie, negative for ER, PR and HER2. A PD-L1 test is done for these patients and if found positive, drugs such as Atezolizumab can be given along with chemotherapy. Other drugs such as Pembrolizumab and Avelumab can be considered.
Male breast cancer is a rare cancer and accounts for about 1% of all breast cancers. Risk factors for male breast cancer include older age, usually above 60 years of age. The risk is also present in people with higher oestrogen levels such as in those who are obese or have liver disease. Those male patients who have a genetic condition called Klinifelter syndrome or have a strong family history of cancer or are known to have BRCA1 or 2 mutations in the genes are also at risk of getting a breast cancer.
Symptoms associated with a male person having breast cancer are similar to a female and include seeing or feeling a lump in the breast, noticing an indrawn nipple, or discharge from the nipple or a swelling under the arm. An ulcer or rash around the nipple are also seen.
Investigations for male breast cancer are similar to a female breast cancer and are listed above. Similarly, treatment options including surgery, chemotherapy, radiotherapy, hormonal therapy, and biological therapy are all used as treatment. Most patients have a mastectomy rather than a lumpectomy. When hormone therapy is used, only Tamoxifen is appropriate in male patients.




