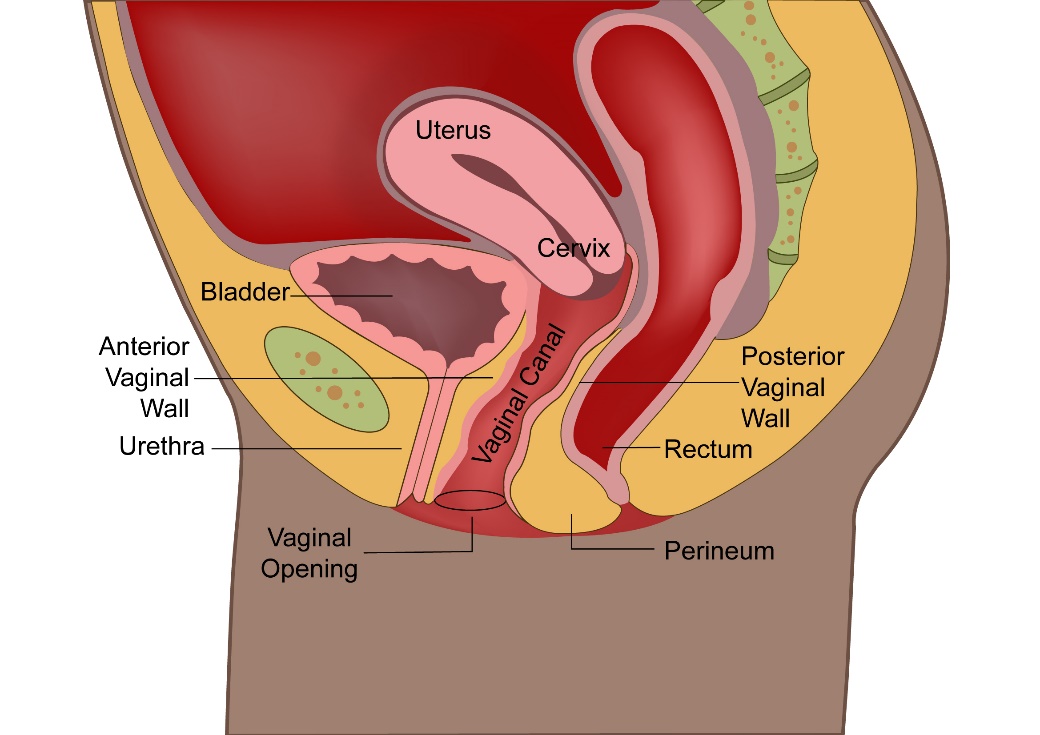
Cervix is the lower part of the Uterus or womb. Along with the Uterus, vagina, Ovaries and fallopian tubes, it makes up the female reproductive system.
The Cervix can be divided into ectocervix and endocervix and these two parts are separated by the transformation zone. This zone is where the cervical cancer most often occurs in.
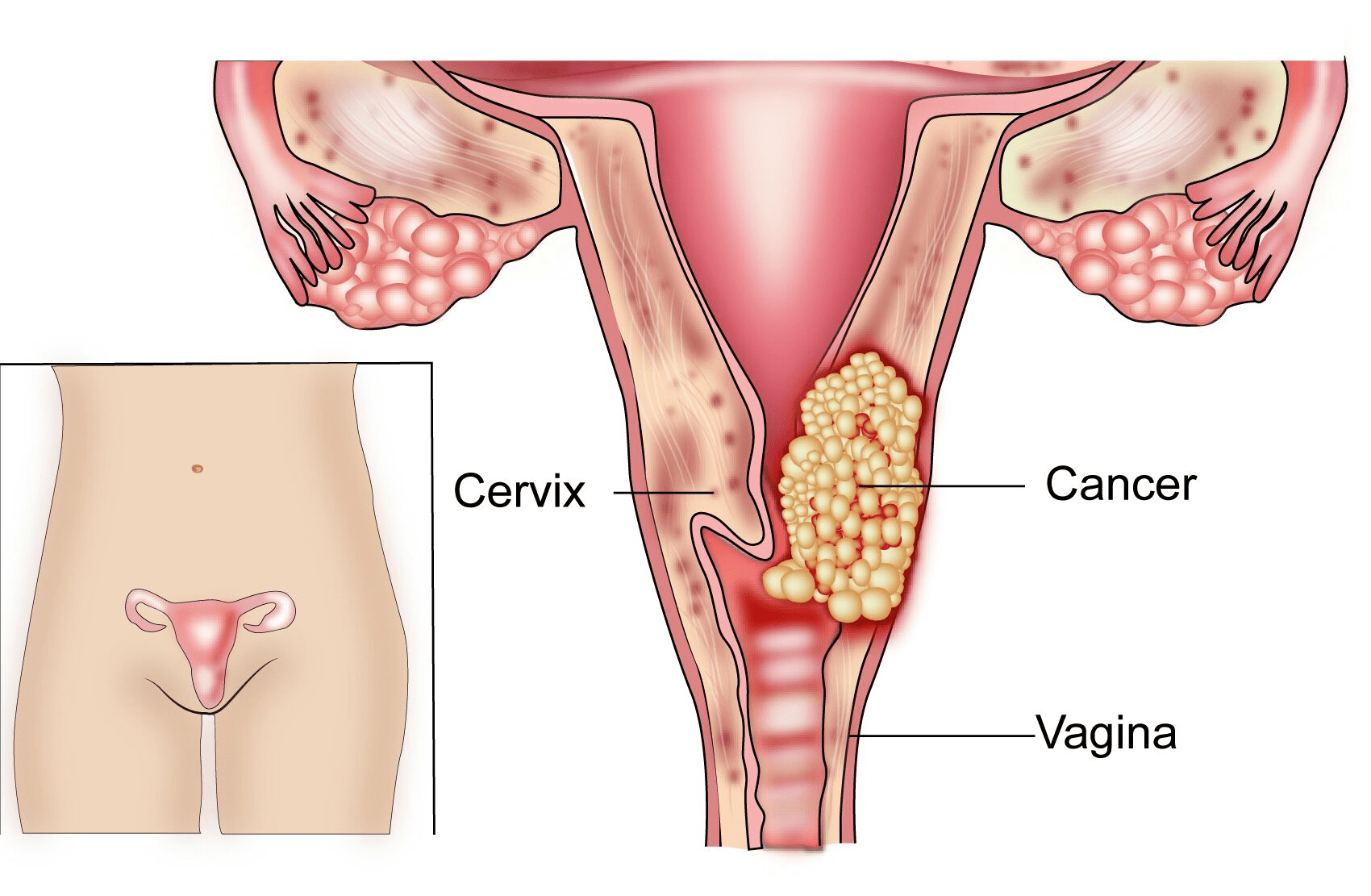
A cancer that starts in the Cervix is called as Cervical Cancer. According to Globocan Data, about 96,922 cases of cervical cancer were diagnosed in India in 2018 and there were 60,078 deaths due to cervical cancer in India in that year.
Cervical cancer can be of many types. The common types are called as Squamous Cell Carcinoma which starts from cells lining the ectocervix and Adenocarcinoma which occurs in the cells lining the endo cervix. Other uncommon types include Adeno-squamous carcinoma, Neuroendocrine carcinoma and Clear Cell Carcinoma.
HPV Infection
HPV is Human Papilloma virus which is acquired sexually and is the main cause of cervical cancer.
There are over 100 different types of HPV but the ones most associated with cervical cancer are HPV 16 and 18. This HPV virus is transmitted through having sex. Other ways of transmission may also be present but have not been definitely identified.
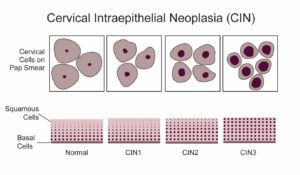
HPV leads to the development of CIN or cervical intraepithelial neoplasia which is a pre-cancerous condition and can go on to develop a cancer if not treated in time. Screening for cervical cancer aims to identify this condition and treat it to reduce the risk of it developing into a cancer.
Smoking
Smoking increases the risk of getting CIN and cervical cancer.
Multiple Sexual Partners
Having multiple sexual partners and starting sex from an early age, history of sexually transmitted infections increases the risk of getting CIN and cervical cancer.
Weak Immune System
People with a weak immune system due to infections such as HIV/AIDS or due to medicines that reduce the immune system are at increased risk of developing cervical cancer.
Cervical cancer can cause symptoms which are listed below. It is important to know that cervical cancer does not cause any symptoms when present in its early stages.
Bleeding
Bleeding through the vagina is a common presenting symptom for cervical cancer. The bleeding can happen in between periods(intermenstrual) or after having sex (post coital) or after menopause (post-menopausal). The bleeding can be irregular or heavy.
Vaginal Discharge
Discharge of fluid from the vagina which is foul smelling or blood stained can be a sign of cervical cancer. Vaginal discharge is a very common symptom in a woman, but persistent symptoms should be reported to a doctor.
Pain
Presence of symptoms of pain in the lower abdomen(pelvis) or pain or discomfort when having sex can also be symptoms related to cervical cancer.
Others
Other symptoms such as weight loss, reduced appetite, blood in the urine or motion or feeling generally unwell can also be symptoms of cervical cancer in an advanced stage.
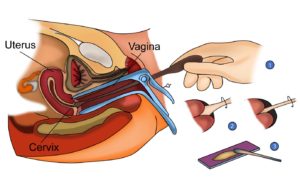
PAP Smear
A PAP smear is a test which the doctor does, to look for cancer or changes that could lead to cancer in the cervix. The doctor will use a small tool to take some cells from the cervix. These cells are then looked at under the microscope for changes. The test can cause a little discomfort but is not painful.
After the age of 30, a Pap smear test is done along with an HPV test. HPV stands for Human Papilloma Virus and if present can increase the risk of cervical cancer. This is a common virus that most women get at some time in their life. The cells that are taken for Pap smear can also be tested for HPV.
The below tests or procedures are done when abnormalities are found on the cervix.
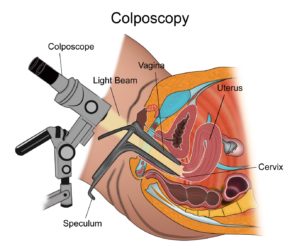
Colposcopy
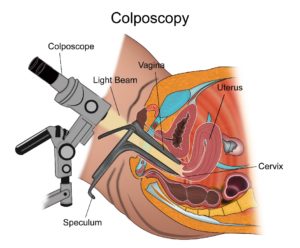
A colposcopy is a test done by a doctor where a magnifying glass is used to have a closer look at the cervix to observe for any abnormalities. This is an outpatient procedure and is done easily.
Loop or Needle Excision
A loop excision is done to remove an abnormal area in the transformation zone, which is at the junction of the ecto cervix and endo cervix. This procedure is done under a local anaesthetic
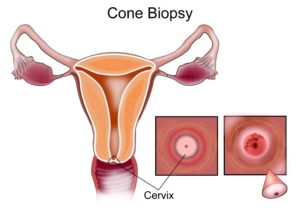
Cone Biopsy
A cone biopsy is a procedure to remove a part of the cervix when an abnormality is found on other tests. This procedure is done with general anaesthesia.
Investigations after Cervical Cancer is diagnosed
Blood Tests
Routine blood tests are done to look for anaemia as well as kidney and liver function.
CT scan
Once a cervical cancer is diagnosed on biopsy, a contrast enhanced CT scan is done of the chest abdomen and pelvis to stage the cancer. This scan is used to look for spread of cancer from its point of origin to other parts of the body.
PET-CT Scan
A PET-CT scan is a PET scan combined with a CT scan. It involves injecting a special radioactive dye into the vein prior to the scan. This special dye will enable to detect cancer better than normal CT scan in certain circumstances. In cervical cancer, PET-CT is recommended for routine staging to identify areas of spread to distant sites in the body as well as local spread around the cervix.
MRI Scan Pelvis
An MRI scan is also routinely used to stage cervical cancer. It is used to assess the pelvis specifically as it can clearly identify areas of spread of cancer in the pelvis.
Examination under Aanaesthesia (EUA)
This is a procedure where the gynaecologist or Oncologist does an internal examination under general anaesthesia to identify and stage the disease locally around the cervix.
Cervical cancer is staged based on the FIGO staging system. This system is based on the findings on examination of the patient and any relevant procedures done but not on any scans done.
Stage 1
In stage 1 Cervical cancer, the cancer is confined to the uterus. This stage is again divided into 1A and 1B depending on the size and its spread.
Stage 2
In stage 2, the cervical cancer outside the uterus but not onto the side wall of the pelvis or the lower one third of the vagina. Stage 2 is further divided into 2A and 2B depending on the extent of spread.
Stage 3
In stage 3 cervical cancer, the tumour extends up to the side wall of the pelvis or the lower one third of the vagina or causes blockage of the ureter leading to hydronephrosis. Stage 3 can be divided into 3A and 3B.
Stage 4
In stage 4 cervical cancer, there is spread of cancer to other organs in the pelvis or to other areas in the body. Stage 4 can be divided into 4A and 4B.
Treatment of Cervical cancer is largely dependent on the stage of the cancer at diagnosis.
Staging is mainly done by the FIGO staging system. The FIGO staging system doesn’t take into account the results seen on the scan, but these results are also considered when a treatment plan is defined.
The different options of treatment include Surgery, Radiotherapy, Chemotherapy and supportive care. Treatment options can be clubbed into different groups. These are
Treatment of Early Cervical cancer
Early cervical cancer would be those that are stages 1A, 1B1 and some 2A cancers. The options of treatment for these stages are
- Surgery
- Radiotherapy
- Chemo-Radiotherapy
Surgery
Surgery for Cervical cancer includes different types of surgery depending on the stage of disease and the characteristics of the patients. Surgery is usually considered as an option of treatment for stages 1A and 1B1. Some stage 1B2 and 2A patients may be treated with surgery also but may need radiotherapy also after the surgery. This is decided based on the findings observed after surgery. Stages beyond that are treated with Chemoradiotherapy. The different options of surgery are listed below.
Radical Hysterectomy
This type of surgery involves removal of the Uterus and the Cervix, a part of the vagina, surrounding tissues(parametria) and lymph nodes present in the pelvis. For patients with very early disease, that is up to stage 1A1, a simple hysterectomy may be enough which involves removal or the uterus, cervix and a small margin of the vagina without removing the parametria and lymph nodes. Another procedure called conization may also be adequate for very early cervical cancer.
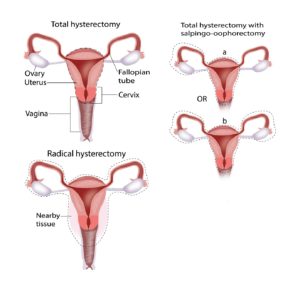
Fertility Sparing surgery
For young patients with early cervical cancer who wish to preserve fertility (want to have a baby later), a conization procedure can be done. This involves removal of a part of the cervix that is abnormal, leaving everything else behind. The other option in this setting is an operation called trachelectomy, where the cervix is removed, and the uterus is left behind.
Radiotherapy
Radiotherapy is the use of high energy x-rays to treat cancer. There are mainly two types of radiotherapy used in cervical cancer. One is external beam therapy, where the radiotherapy treatment is given by a large machine present in a room and the other type is brachytherapy where a radioactive source is inserted into the part of the body that needs treatment.
Radiotherapy in early cervical cancer is used when surgery is not possible due to patient having other medical issues or in a situation where the patient is not fit enough for surgery.
Adjuvant Radiotherapy
Here radiotherapy is given as a treatment after definitive surgical treatment. Not all patients after surgery for cervical cancer need radiotherapy. Only those patients with certain features on the cancer benefit from receiving this treatment after surgery. When radiotherapy is given along with chemotherapy, it is known as chemoradiotherapy and is also used in this setting.
Definitive Chemoradiotherapy
This is one of the main options of treatment for patients with early cervical cancer who cannot have surgery for various reasons. It is an option of treatment for most patients with stage 1B2 and stage 2A. Radiotherapy is given once a day five days a week for 5-6 weeks. In patients who are fit, chemotherapy is given at the same time as radiotherapy. It is done once a week for 5-6 weeks. Radiotherapy is given to the lower part of the abdomen called the pelvis which includes the cervix, uterus, a part of the vagina, surrounding structures and lymph nodes in the pelvis.
After completion of external beam radiotherapy, brachytherapy is given to complete the whole treatment. Brachytherapy as mentioned above, is radiotherapy given with the help of a radioactive source inserted into the part of the body. In cervical cancer, the brachytherapy source is inserted into the vagina and uterus where radiotherapy is delivered. The advantage of brachytherapy is that it gives a high dose of radiotherapy to a small area where it is needed.
The number of brachytherapy treatments needed, and the duration of the treatment will depend on the type of radioactive source and machine used for treatment. Overall 2-6 treatments are needed.
Chemo-Radiotherapy treatment is associated with side effects. The side effects associated with external beam radiotherapy part include tiredness, loose motions, pain in the abdomen, burning sensation while passing urine, soreness and redness around the vagina and surrounding skin. Brachytherapy side effects include, loose motions, soreness in the rectum, long term side effects such as narrowing and stiffness of the vagina. The side effects of chemotherapy include tiredness, risk of infection, thinning of hair, nausea and vomiting. These side effects are variable from patient to patient with some having more side effects than others.
Locally Advanced Cervical Cancer
Locally advanced cancer involves cervical cancer staged 1B2 and above. These cancers are treated with definitive Chemoradiotherapy only as described above. Radiotherapy alone is given to patients who are not fit or cannot have chemoradiotherapy. Surgery is not the preferred option of treatment for these patients.
Chemoradiotherapy consists of 5-6 weeks of external beam radiotherapy followed by brachytherapy as described above.
Types of Radiotherapy techniques used in treatment of Cervical Cancer
As with many cancers treated with radiotherapy, there are many techniques that can be used to treat cervical cancer with radiotherapy and these are briefly described below.
3D Conformal Radiotherapy
This is the minimum standard of radiotherapy that must be used to treat cervical cancer. This technique involves the patient having a CT scan first and all radiotherapy planning process being done with that CT scan.
Intensity modulated radiotherapy (IMRT)
This technique is also commonly used now to treat cervical cancer and can help with reducing the side effects of treatment as compared to 3D conformal radiotherapy.
CT or MRI guided adaptive brachytherapy
This technique uses a CT or MRI (better than CT) to look for disease and planning of brachytherapy with the help of these scans. This helps in better targeting of the cancer with radiotherapy leading to better outcomes.
Brachytherapy is commonly used in cervical cancer as a form of treatment in patients who have radiotherapy to treat it. Brachytherapy is usually given after completion of 5-6 weeks of external beam radiotherapy.
Usually, brachytherapy in cervical cancer is done a week to two after completion of external beam therapy. Depending on the type of radioactive source used, there may be 1-6 treatments in all. A typical brachytherapy treatment is as follows.
First, the patient is taken to the operation theatre or a brachytherapy suite where under sedation or anaesthesia, an applicator is placed in the uterus. The applicator consists of 1-3 tubes which are inserted into the vagina and uterus through the vagina. These are left in place and the patient is then taken for an x-ray or a scan. Some centres may use x-rays in this stage. Others may use a CT scan while some others may use an MRI scan. These x-rays or scans are used to plan the brachytherapy treatment. The patient will be on a bed in the suite or on a ward while the treatment is being planned. The planning part of treatment is done by the radiation oncologist and the medical physicist.
Once the treatment plan is ready, the patient is taken into the treatment room where she lies on the table. A brachytherapy machine is present in the room which contains the radioactive source. The machine is connected to the applicator that was placed in the patient. Treatment is given for a period depending on the dose that is being given and the type of machine used. Once the treatment is complete, the patient can go home and return another day for the next treatment.
In patients who have treatment with a low dose rate machine, the treatment will last many hours and the patient is usually kept on a ward while on treatment. In such a situation there will be only one treatment. In those having high dose rate treatment, short spells of treatment more times are given.
Side effects of brachytherapy for cervical cancer include increased frequency of passing urine, tiredness, loose motions. Long term side effects include narrowing of the vagina, bleeding when passing motion or urine. Vaginal dilators should be used regularly to reduce risk of vaginal narrowing.
Metastatic Disease
Patients with cervical cancer are known to have metastatic disease (stage 4B) when the cancer has spread to different parts of the body and is not amenable to curative treatment options.
The treatment options for metastatic disease include chemotherapy and radiotherapy and sometimes, surgery.
Chemotherapy
Chemotherapy is the main option of treatment for metastatic cervical cancer. The common drugs used as chemotherapy in this setting are Cisplatin, Carboplatin, Paclitaxel, Vinorelbine, Gemcitabine and Bevacizumab, which is a biological agent. These drugs are used alone or in combination.
Immunotherapy
Newer drugs such as Pembrolizumab are used in the treatment of cervical after first line chemotherapy. A PD-L1 test is done on the biopsy sample to see if the patient will benefit from this drug or not. Immunotherapy drugs use the body’s immune system to control the cancer.
Radiotherapy
Radiotherapy in patients with metastatic cervical cancer is used to control symptoms of cervical cancer rather than to cure it as described in above sections. Cure with radiotherapy or chemoradiotherapy is usually not an option in metastatic disease as the disease is too widespread to allow such treatments to be given. Therefore, the radiotherapy here is given for shorter durations lasting from one day up to 15 days depending on the necessity. Occasionally high dose radiotherapy can be used to control cancer if there is a recurrence confined to one area of the body.
Surgery
Surgical removal of cancer is sometimes possible in metastatic or recurrent disease if there is disease present in only one area of the body and this can be removed by an operation. A PET-CT scan is done before to confirm that there is only one area of disease.
Supportive Care
In patients not suitable for any treatment, supportive care can be provided to help with control of symptoms produced by the cancer.
Cervical Cancer is one of the commonest cancer among women in India. Fortunately, there are strategies now available which help in significantly reducing the risk of getting cervical cancer.
Cervical Cancer is caused due to infection with a virus called HPV. This virus is transmitted sexually and is very common. In a large majority of patients, the virus is harmless and does not cause any symptoms. In some people though, it can lead to the development of a pre-cancerous condition called CIN or cervical intraepithelial neoplasia which can in turn develop into cancer.
Cervical cancer can be prevented by giving a vaccine to prevent HPV infection and by screening tests to detect CIN and to treat it before it develops into a cancer.
HPV Vaccines
Vaccines are available to prevent HPV infection which leads to cervical cancer mainly. HPV is a virus that is transmitted from person to person by skin contact through sexual activity.
This vaccine is offered to girls aged 9 to 26 years of age. Ideally the vaccine should be given before the girl or woman becomes sexually active as this provides maximum benefit. The vaccination can also be given after sexual activity has begun but the benefit may be limited at that point as the woman may have already been exposed to the virus by then. Three doses of the vaccine are required to gain full immunity.
Three formulations are available which are given as injections.
Gardasil
This vaccine protects against HPV 6,11,16 and 18
– Two doses for girls aged between 9 to 15 given at 0 and 6 months
– Three doses for girls 15 or over
– If 3 doses, then given at 0, 2 and 6 months
– Benefit seen is 97%-100% before exposure to HPV
– Benefit seen in 44% after exposure to HPV
Gardasil 9
This Vaccine protects against 9 HPV viruses – In adults less than age of 45, 3 doses are given at 0, 2 and 6 months.
Cervarix
– Protects against HPV 16 and 18
– Three doses for girls 45 or less
– If 3 doses, then given at 0, 1 and 6 months
– Benefit seen is 93% before exposure to HPV
– Benefit seen in 53% after exposure to HPV
Cervical cancer is very common in India and screening helps in detecting pre-cancerous conditions and cancer of the cervix. Cervical Intra epithelial neoplasia (CIN 1-3) is a pre-cancerous condition that can develop into a cervical cancer over a period of time. Detecting these conditions early increases the chance of cure.
Who benefits from Cervical Cancer screening
Cervical cancer screening should be offered to all women over the age of 20. This is continued every 3 years until the age of 65.
How is cervical cancer Screening done
Cervical cancer screening is done with the help of a Pap smear test. This is a test which the doctor does, to look for cancer or changes that could lead to cancer in the cervix.
The doctor will use a small tool to take some cells from the cervix. These cells are then looked at under the microscope for changes. The test can cause a little discomfort but is not painful.
After the age of 30, a Pap smear test is done along with a HPV test. HPV stands for Human Papilloma Virus and if present can increase the risk of cervical cancer. This is a common virus that most women get at some time in their life. The cells that are taken for Pap smear can also be tested for HPV.
The results of the test will be available in a day or two. Having an abnormal test doesn’t mean there is cancer and most women who have an abnormal smear test don’t have cancer.
If the test is abnormal, the doctor may advise a HPV test if it was not done or a colposcopy to look at the cervix closer. Sometimes, a repeat Pap smear in 12 months is all that is required.
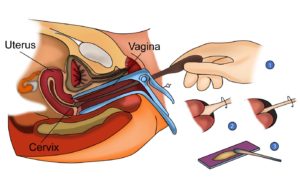
A Colposcopy is a test where the doctor can take a close look at the cervix and take a biopsy if needed.
If the Pap smear is normal, it should be repeated every 3 years. After the age of 30, if an HPV test is added to the Pap test, then screening can be done every 5 years.




