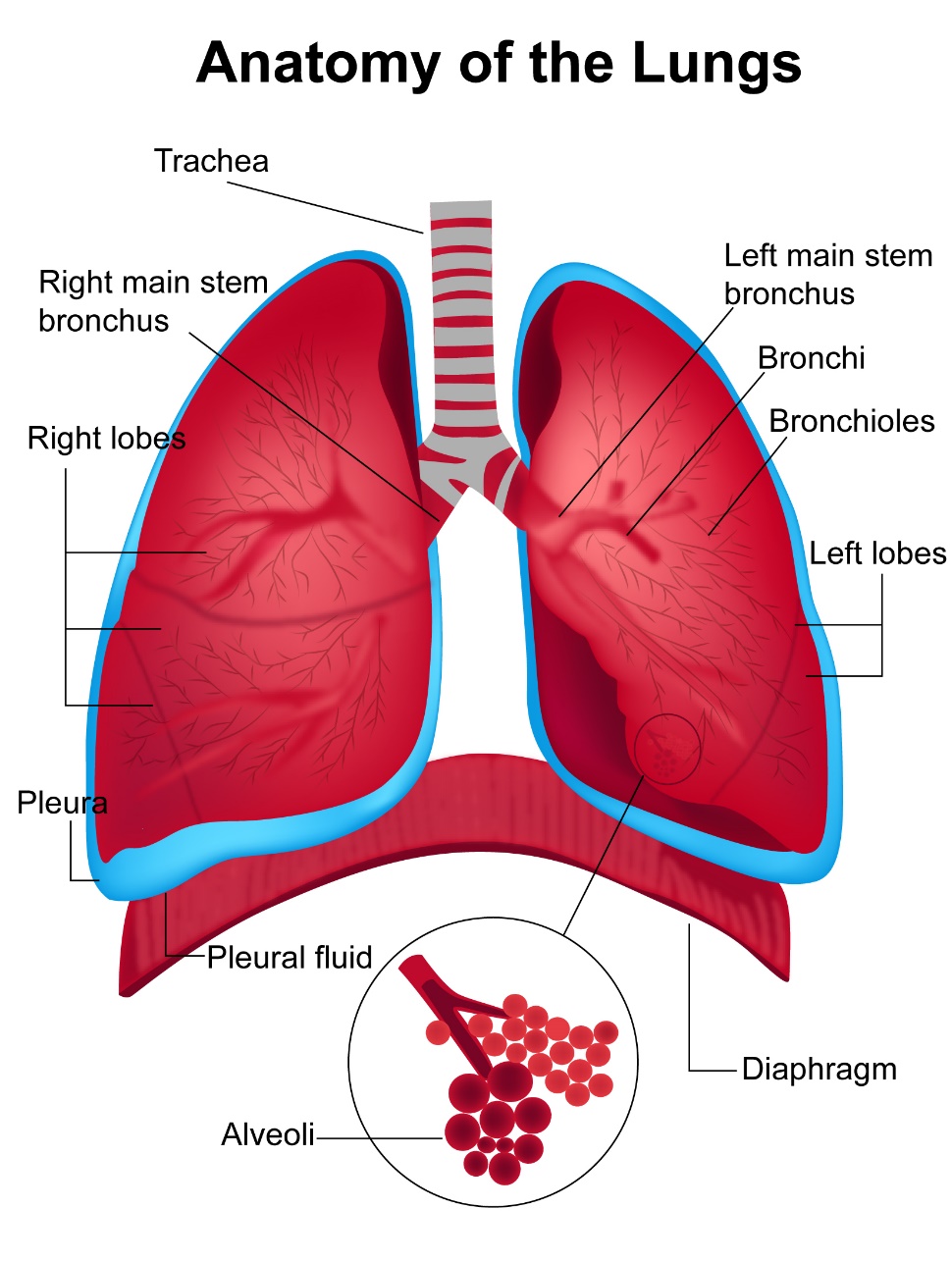
Lungs are organs in the chest that help you breathe. There are two lungs (right and left) which are divided into lobes. The right lung has three lobes and the left lung has two lobes.
The air that we breathe goes from the nose and throat into the trachea or windpipe. The trachea divides into two bronchi which supply the air to each lung. The bronchi divide further inside the lung. As we breathe in and out, air enters the lungs where Oxygen is absorbed into the body and carbon dioxide is released.
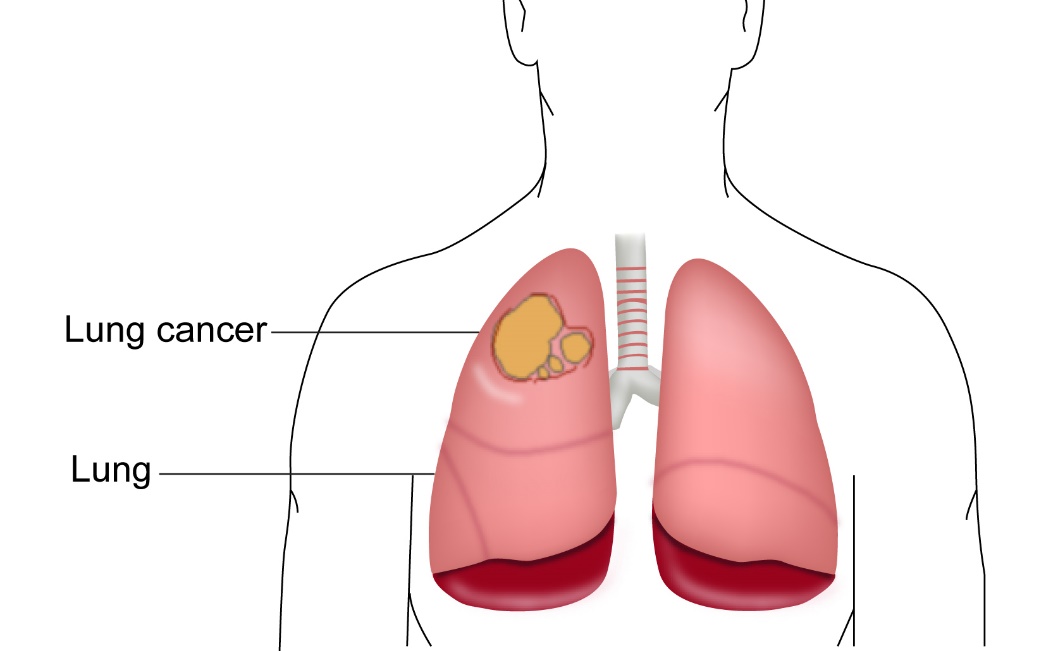
Lung cancer is cancer that has started in the lungs. Usually lung cancer starts in the lining of the bronchi and hence it is also called as carcinoma of the bronchus.
Many cancers that have originated in other parts of the body can spread to the lungs. This is called metastatic or secondary cancer in the lung and is very different from primary lung cancer which is discussed here. For example, if a patient has breast cancer that has spread into the lung, then it is metastatic breast cancer and not lung cancer.
According to Globocan data 2018, there were 67,795 new lung cancers in India in 2018, making up 5.9% of all cancers.
Types of Lung Cancer
There are two main types of Lung Cancers. The commonest type is Non small cell Lung Cancer (NSCLC) which makes up about 80% of all lung cancers. The other type is Small Cell Lung cancer (SCLC) and makes up about 15-20%.
Non Small cell Lung Cancer
This is the commonest type of lung cancer. This type of cancer can be subdivided into Squamous cell carcinoma, Adenocarcinoma and Large cell carcinoma. Squamous cell carcinoma is more common in smokers. It develops from the cells lining the bronchi. Adenocarcinoma develops from the mucus producing glands that line the bronchi. This type is seen in people who smoke and is the commonest type of lung cancer in non smokers. Adenocarcinoma in situ is an early form of invasive adenocarcinoma. This sub type was previously known as bronchoalveolar carcinoma.
Small Cell Lung Cancer
This cancer is almost exclusively seen in smokers. It is called as such because of the look of the cells as seen under the microscope. This type of cancer can grow rapidly.
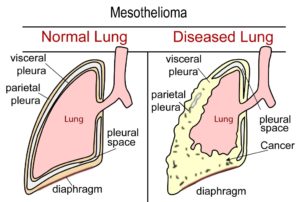
Mesothelioma
Mesothelioma is a cancer that develops on the coverings of the lungs (Pleura). Mesothelioma develops mainly in people who had previous exposure to asbestos.
Carcinoid Tumour
Carcinoid tumour of the lung is an uncommon cancer of the lung. It is generally slow growing and can be managed well with surgical removal.
Others
Other cancers that are rare in the lung are sarcomas and lymphomas.
A risk factor for Lung cancer is one that increases the risk of getting Lung cancer. These are listed here below.
Smoking
Smoking is one of the biggest risk factors for lung cancer. This can be smoking a cigarette, beedi or a cigar. Recent studies have shown that in men there is a 25% chance of developing lung cancer in smokers who smoke more than 5 cigarettes per day. In women this is 18%. The earlier in life smoking begins, the higher the risk of getting lung cancer is. Stopping smoking for 12 to 15 years, reduces the risk of getting lung cancer back to that of a non smoker. Passive smoking (being exposed to cigarette smoke from other smokers) also increases the risk. See section on prevention of cancer for more details about smoking.
Asbestos Exposure
Exposure to asbestos not only increases the risk for developing mesothelioma (cancer of covering of lung) but also that of lung cancer. Exposure to asbestos in a smoker increases the risk further. There can be a long latency period between the exposure to asbestos and the development of lung cancer.
Smoke from cooking
Exposure to smoke from cooking and heating indoors causes inhalation of smoke. This leads to an increase in risk of lung cancer. This risk is more with wood burning stoves.
Industrial exposure
Exposure to industrial agents like arsenic, nickel, chromium, soot, tar, polycyclic hydrocarbons, exposure to diesel exhaust and pollution in general increases the risk of developing lung cancer.
Previous radiotherapy
People who previously had radiotherapy to the chest for other cancers like lymphoma, breast cancer or germ cell cancers have an increased risk of developing a lung cancer. This risk is increased further with smoking.
Lung cancers can produce a varied number of symptoms. Common symptoms are listed here below. Having any of these symptoms doesn’t mean that there is lung cancer, but it is important to see a doctor to have the symptoms investigated.
Cough
Cough is one of the commonest presenting symptoms of Lung cancer. A cough that does not settle in three weeks should be investigated with a chest x-ray. The cough can be associated with other symptoms.
Breathlessness
This is also a common presenting symptom in Lung cancer. The patient notices that their breathing is gradually getting worse over a period of time.
Coughing up of blood
Cough with blood stained sputum or frank blood, is a sign of lung cancer. This symptom should be investigated urgently.
Pain
Some patients can experience chest pain as a result of lung cancer. Any persistent pain that is not settling should be investigated. Sometimes, patients can complain of pain coming down the arm and around the shoulder or pain in the back of the chest.
Change in Voice
Change in voice or hoarseness of voice is present in some patients with lung cancer
Other symptoms
Other symptoms associated with lung cancer are tiredness, loss of appetite and weight and difficulty with swallowing.
If a lung cancer is suspected, the following investigations are done.
Chest x-ray
A chest x-ray is usually the first test that is done for persistent chest symptoms or when there is a suspicion for lung cancer. A chest x-ray is not a very sensitive test and may be normal even in the presence of a cancer when the cancer is small or is present behind normal structures.
CT Scan
A CT or computed tomographic scan is done when an x-ray is normal and there is still suspicion, or an abnormality is found on an x-ray. The CT scan uses x-rays to give detailed images of the chest and can show up most abnormalities in the chest that are bigger than a few millimetres.
It is quick, painless and is available in most centres. A contrast injection is usually given prior to the scan to get better images.
Bronchoscopy
A bronchoscopy is a test where a thin tube is placed up the nose into the throat and lungs. This is done under mild sedation and local anaesthetic spray. With the help of this test, the doctor is able to look for an abnormality inside of the bronchi and take any biopsies if need. It is an outpatient procedure and is painless.
Biopsy
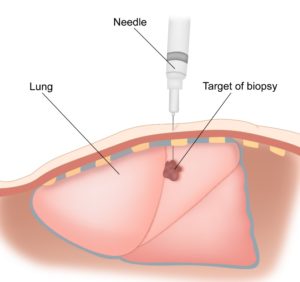
If an abnormality is found on the above tests, the doctor may request for a biopsy. A biopsy is a test where a piece of tissue is removed and looked under a microscope to establish a diagnosis. The biopsy of the lung can be done with the help of a CT scan (CT guided biopsy) or at bronchoscopy. Sometimes a mediastinoscopy or a thoracoscopy may be needed to get a sample for biopsy.
Lung Function Tests
These are tests used to determine how well the lungs are working. The test is done to assess patient’s fitness for surgery or radiotherapy.
PET-CT Scan
A PET –CT scan is a specialized CT scan where a radioactive tracer is injected into the body prior to the CT scan. This tracer lodges in areas within the body where there is high requirement for glucose. As cancers need a lot of glucose to survive, they take up the tracer much more than the rest of the body. The cancer can then be easily spotted on the scan. This test is done after the diagnosis of lung cancer is made. The purpose of this test in Lung cancer is to look for spread of cancer from the lung to other parts of the body. The scan is very sensitive and will help to pick up even small areas of spread.
Mediastinoscopy
This is a test which is done under general anaesthesia. It is not needed in all suspected lung cancer patients. It is mainly done to accurately stage patients who are being planned for lung cancer surgery.
Endobronchial Ultrasound (EBUS)
This is a new type of test that may be done instead of a mediastinoscopy. You’ll either have a general anaesthetic or you may be given a mild sedative to make you feel drowsy. Again, this test is needed only in a small set of patients and is available in some centres in India. This test helps to biopsy any lymph glands in the chest that may be involved with the cancer.
Pathological Diagnosis
Following the biopsy, the pathologist examines the specimen under the microscope. It may be needed for the pathologist to do some special tests on the specimen before a diagnosis is made.
If it is a lung cancer, the report will describe the cancer as small cell or non small cell carcinoma.
If it is non small cell carcinoma, it can be further sub typed into squamous cell carcinoma, adenocarcinoma or large cell carcinoma. Sometimes sub typing is not possible. If it is adenocarcinoma, special testing for EGFR, ALK and ROS status is also requested. PD-L1 testing if feasible.
Next generation Gene Sequencing
This is a recommended test in lung cancer but is expensive. This test looks at the genes of the biopsy sample and will show all the genetic abnormalities present in the cancer. The doctor is able to tailor the treatment based on these tests. This is particularly useful in stage 4 lung cancer patients and does all the above tests described such as EGFR, ALK, ROS and others in one go.
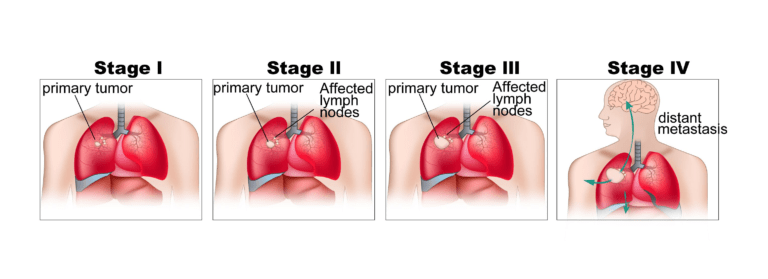
The stage of a cancer is a word used to describe the size and location of the cancer in the body.
Knowing the stage of the cancer helps the doctors to decide on the most appropriate treatment
The staging system is different for Non-small cell and small cell lung cancer. Non-small cell Lung Cancer is staged based on the TNM staging system or the number system. Small cell Lung Cancer has only two stages.
Staging with either system is based on the size of the tumour in the lung, the spread of the cancer locally in the lung and into the lymph nodes, and spread of cancer into other parts of the body.
TNM Staging
TNM stands for tumour, node and metastases.
T Staging
T1a – The tumour is contained within the lung and is smaller than 2cm across
T1b – The tumour is contained within the lung and is between 2 and 3 cm across
T2 – The tumour is between 3 and 7cm across or has grown into the largest airway (the main bronchus) more than 2cm below the part where it divides to go into each lung or the tumour has grown into the inner lining of the chest cavity (the visceral pleura) or the tumour has made part of the lung collapse.
T2 Tumours that are 5cm or smaller are classed as T2a and those larger than 5cm are T2b
T3 – The tumour is larger than 7cm or has grown into one of the following structures – the chest wall the central lining of the chest cavity (the mediastinal pleura), the muscle at the bottom of the chest cavity (the diaphragm), or the outer covering of the heart (the pericardium) or the tumour has made the whole lung collapse or there is more than one tumour nodule in the same lobe of the lung
T4 – The tumour has grown into one of the following structures – the area between the lungs in the middle of the chest (the mediastinum), the heart, a major blood vessel, the wind pipe (trachea), the area where the main airway divides to go to each lung, the food pipe (oesophagus), a spinal bone, the nerve that controls the voice box, or there are tumour nodules in more than one lobe of the same lung
N Staging
N0 – there is no cancer in any lymph nodes
N1 – there is cancer in the lymph nodes nearest the affected lung
N2 – there is cancer in lymph nodes in the centre of the chest (mediastinum) but on the same side as the affected lung or there is cancer in lymph nodes just under where the windpipe branches off to each lung
N3 – there is cancer in lymph nodes on the opposite side of the chest from the affected lung or in the lymph nodes above either collar bone or in the lymph nodes at the top of the lung
M Staging
M0 – There are no signs that the cancer has spread to another lobe of the lung or any other part of the body
M1a – There are tumours in both lungs or fluid around the lung or heart that contains cancer cells – (a malignant pleural effusion) or pericardial effusion
M1b – there are lung cancer cells in distant parts of the body, such as the liver or bones
Number staging
| Stage | T | N | M |
|---|---|---|---|
| Ia | T1a | N0 | M0 |
| T1b | N0 | M0 | |
| Ib | T2a | N0 | M0 |
| IIa | T1a | N1 | M0 |
| T1b | N1 | M0 | |
| T2a | N1 | M0 | |
| IIb | T2b | N1 | M0 |
| T3 | N0 | M0 | |
| IIIa | T1 | N2 | M0 |
| T2 | N2 | M0 | |
| T3 | N2 | M0 | |
| T3 | N1 | M0 | |
| T4 | N0 | M0 | |
| T4 | N1 | M0 | |
| IIIb | T4 | N2 | M0 |
| T1 | N3 | M0 | |
| T2 | N3 | M0 | |
| T3 | N3 | M0 | |
| T4 | N3 | M0 | |
| IV | T Any | N Any | M1a or 1b |
Staging for Small Cell Lung Cancer
Small Cell Lung Cancer has two stages. Limited stage and Extensive stage.
Limited stage is where all the cancer is localized to one side of the chest. If the cancer is present in more than one half of the chest, it is called extensive stage. Treatment options differ between the two stages.
Small cell lung cancer is also staged based on the TNM and number staging as above.
The management of stage III lung cancer is controversial and therefore variable. Based on the exact location of the tumour and involved lymph nodes, the surgeon will give an opinion as to whether the cancer can be removed completely with surgery or not. If it is removable and patient is fit, the patient will usually go for surgery. Following surgery, other treatment options are available to increase the chances of cure. In patients who have surgery and have surgical margins that contain cancer or in those with significant involvement of mediastinal lymph nodes, radiotherapy for 6 weeks may be an option. Other patients can benefit from three months of chemotherapy after surgery.
For patients whose cancer is EGFR positive after surgery, treatment with Osimertinib tablets can be used. This treatment helps with improving progession free survival.
If the surgeon feels that the tumour is not removable, sometimes giving chemoradiotherapy may make it removalbe. The surgeon could then resect the tumour at that time. This option is not practiced in all centres and there, patients not suitable for surgery will have chemoradiotherapy only. In fit patients, this is concurrent chemoradiotherapy, where chemotherapy and radiotherapy are given at the same time. Otherwise sequential chemoradiotherapy may be used where chemotherapy followed by radiotherapy is used.
If chemoradiotherapy is not suitable, then radiotherapy alone can be used to treat patients with this condition. Sometimes, only chemotherapy, immunotherapy or targeted therapy may be used if more aggressive forms of treatment are not feasible due to various reasons.
Treatment of Small cell Lung Cancer is determined by the stage of cancer at diagnosis. Surgery is usually not an option in the management of small-cell lung cancer.
Treatment of Limited stage Small Cell Lung Cancer
Limited stage small Cell Lung Cancer is treated with combination of chemotherapy and radiotherapy. This is called as concurrent chemoradiotherapy. The aim here is to cover all the area of the cancer with radiotherapy. Combination of the two treatments given together provides the best chance of control of the disease.
The chemotherapy is given for 3 days out of every 21 days. Up to four such cycles of such chemotherapy are given with radiation. The radiation is given once daily, five days a week for up to seven weeks. In some centres, radiotherapy may be given twice daily over three weeks. If the fitness off the patient is not very good, then chemotherapy is offered first followed by radiotherapy.
Side effects of chemoradiotherapy can include cough, breathlessness, soreness or pain in the chest, pain or discomfort on swallowing, tiredness, redness of the skin on the chest, sore throat, low counts of cells in the blood, risk of infection, nausea and vomiting. The side effects of radiotherapy can last for up to 4 weeks after completion and then improve.
There is also benefit of treating the brain with radiotherapy even in the absence of disease there. This is called as Prophylactic cranial Irradiation (PCI). This treatment helps reduce the risk of cancer recurring in the brain and can be given after completion of the above treatment. The Oncologist will explain the pros and cons of this treatment.
Treatment of Extensive stage Small Cell Lung Cancer
Extensive stage small cell lung cancer is treated with chemotherapy alone in the first instance. This chemotherapy is usually a combination of 2 drugs and is given for 3 days every 3 weeks. Up to 4 or 6 such cycles and given. A scan is done again after 2-3 cycles of treatment to check for response of the cancer to the treatment. Chemotherapy is continued provided the patient is tolerating the treatment well and the disease is responding to treatment.
Combination of above mentioned chemotherapy with immunotherapy can provide a better response than chemotherapy alone. Immunotherapy drugs such as Durvalumab or Atezolizumab are given along with chemotherapy for 4 cycles followed by continuation of immunotherapy drug as maintenance treatment. This is the preferred option in these patients providing it can be afforded as immunotherapy is expensive.
Following completion of chemotherapy, radiotherapy is sometimes offered to the chest. Prophylactic cranial irradiation (PCI) as described in the above paragraph can also be used here. An oncologist will explain about the pros and cons of that.
The chemotherapy drugs that are commonly used in the treatment of small cell lung cancer are Cisplatin, Carboplatin, Etoposide, Topotecan and Paclitaxel.
Chemotherapy for small cell lung cancer is very effective in reducing the cancer symptoms and shrinking the cancer. However, it can cause some side effects. These are
- Hair loss
- Nausea and vomiting
- Tiredness
- Soreness in the mouth
- Loose motions
- Constipation
- Changes to hearing
- Risk of Infection
- Taste changes
- Tingling in Hands and feet
- Anaemia
- Bleeding
Treatment of relapsed or recurrent small cell lung cancer
If the cancer recurs after initial treatment, the treatment options would depend on the area of recurrence, the extent of recurrence, the patient’s fitness and previous treatment given. Therefore, treatment options can include chemotherapy and radiotherapy. If prior chemotherapy was given and there is a long interval between that treatment and relapse, the same chemotherapy can be used again. If not second-line options are considered. The radiotherapy or chemotherapy used in the setting of recurrent or relapsed cancer is mainly to control symptoms the cancer produces. Radiotherapy used here is given over 1-10 treatments on a daily basis. Sometimes options such as endobronchial brachytherapy are used in this setting. This involves placing a radioactive source into the bronchus where the cancer is causing a blockage.
Immunotherapy
Use of drugs called checkpoint inhibitors are used after failure of chemotherapy for small cell lung cancer. This is called as second line treatment, one which is used after initial chemotherapy. Nivolumab is a drug that is given into the vein once every 2 weeks. Side effects are present with this treatment, sometimes severe but usually lesser than that of chemotherapy.
What is Mesothelioma
Mesothelioma is a cancer that starts from the mesothelium. A Mesothelium is a membrane that lines the chest, abdomen and the organs in them. The mesothelium lining the lung is called the pleura. The pleura is made of two layers, outer layer called parietal pleura and inner layer called visceral pleura. These two layers have a thin film of fluid separating them. A mesothelioma can originate from the pleura or from the lining of the abdomen. This type of cancer mainly occurs due to exposure to asbestos and smoking.
Asbestos Exposure
Asbestos exposure is the main risk factor for mesothelioma. There are many types of Asbestos. Blue asbestos, brown asbestos and white asbestos.
Asbestos is made up of tiny fibres which can be inhaled or ingested. When inhaled they can lodge in lungs and cause lung diseases by causing inflammation in the lungs. Some of these fibres can travel to the pleura causing pleural diseases and Mesothelioma. Asbestos is present extensively in India in various industries. People who are exposed to asbestos include construction workers, plumbers, motor mechanics, electricians, shipbuilders and the general public where asbestos is used for roofing houses.
There is a long latency period between exposure to asbestos and developing illnesses due to its exposure. Asbestos is completely banned in over 50 countries around the world but is still widely used in India.
Symptoms of mesothelioma
Symptoms of mesothelioma can include cough, breathlessness, chest pain, coughing up of blood, weight loss, tiredness, fever, sweating and abdominal symptoms such as swelling of the abdomen. A common problem seen in this cancer is development of pleural effusion where there is accumulation of fluid between the 2 layers of the pleura covering the lung. This leads to progressive breathlessness.
Diagnosis of Mesothelioma
Mesothelioma is diagnosed based on the symptoms of the patient, the x-ray and scan findings and the result on biopsy.
The common investigations done are chest x-ray, CT scan of the chest and aspiration of the pleural fluid and pleural biopsy to look for mesothelioma cells. Occasionally, all these tests will not reveal a diagnosis and therefore special tests are needed. These are
Video assisted Throacoscopy (VATS)
This is a test where a thin tube with a camera is inserted in between the layers of the pleura to look for the presence of a mesothelioma and to get a tissue sample for biopsy. This is usually done by the thoracic surgeon and is a daycare procedure.
Treatment of Mesothelioma
Surgery
VATS Pleurectomy :
As the lung is covered by the pleura, the presence of fluid or a mass in the pleura can cause reduced expansion of the lung leading to breathlessness. This is a procedure where the affected pleura is resected with the help of video assistance. It helps in releasing the trapped lung, thereby improving breathlessness.
VATS Pleurodesis :
In diseases of the pleura, there can be fluid accumulation between the two linings of the pleura. This is called as pleural effusion. Pleural effusion causes breathlessness which can be relieved with removal of pleural fluid. VATS guided pleurodesis is a procedure where the pleural effusion is drained and the two layers of the pleura are fused, so that the effusion does not re accumulate.
Radical Extrapleural Pnemonectomy :
This is an option practiced in some centres. It involves removal of the entire lung with the pleura on the affected side along with the covering of the heart(pericardium) and the diaphragm on that side. This is a very major operation with a lot of side effects and risk of death, that most centres don’t offer it to patients anymore and is only done in the context of clinical trials.
Radiotherapy
Radiotherapy is used sometimes to treat the chest wall in the area where a drain or a tube was put in to take a biopsy or drain the pleural fluid. Radiotherapy here helps to reduce the risk of mesothelioma spreading to the outside of the chest.
Chemotherapy
Chemotherapy is used to reduce the cancer and improve symptoms. Usually combination chemotherapy is used which is effective. Treatment with chemotherapy in mesothelioma is aimed to control the cancer and symptoms only. drugs used for mesothelioma include Cisplatin, Carboplatin and Pemetrexed. These drugs are given as a combination and given once every 21 days for 4-6 times or cycles. Scans are done to check for response of the cancer to the chemotherapy.
Pleurodesis
Most patients with advanced mesothelioma develop pleural effusion which is a collection of fluid between the two outer layers of the lung (pleura). Pleurodesis is a procedure where the fluid is removed, and the two layers of pleura are joined together by injecting a substance into them. For this procedure to be done, the patient will need to remain in hospital for a few days. A chest tube is inserted with the help of a local anaesthetic and the tube remains for a few days to drain the fluid completely and for the substance to be injected into the space. Once done, the drain is removed, and the patient can go home.
Surgery for non-small cell lung cancer involves removal of the cancer and affected lymph nodes around the lung. It is the best option for treating cancers that remain localized to one side of the chest.
Stage 1 and 2 cancers should be treated with surgical resection unless there is a specific reason why surgery should not be done (for example, reduced fitness level, poor lung function etc).
The type of surgical operation done depends on the location of the cancer. A lobectomy is an operation where an entire lobe of the lung, which contains the cancer, is removed. The right lung has three lobes and the left lung has two lobes. Sometimes, when the cancer is present at the junction of two lobes, a lobectomy with segmental resection is done or bi-lobectomy (two lobes) is done.A pneumonectomy, where one entire lung is removed, is needed for some patients.
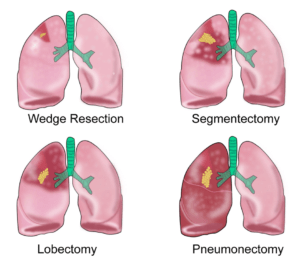
A thoracic surgeon or a surgical Oncologist will explain about the exact type of operation the patient will need. These types of surgeries are all major operations, and the patients need to have a level of fitness for them to cope. Therefore, not all patients may be able to undergo surgery.
Early stage non-small cell lung cancers can be well controlled and cured with surgery. Surgery for stage 3 non-small cell lung cancer is discussed separately. Surgery is not an option in treatment of stage 4 non-small cell lung cancer.
Surgery for lung cancer can be done by the open method where a cut is made on the chest or by a method called VATS (Video assisted thoracoscopic surgery). The VATS procedure involves a smaller cut on the chest and is used to remove early stage cancers. The time taken to recover after surgery is shorter with this procedure. It is not suitable for all lung cancer operations. Robotic assisted surgery is also used in some centres. At the time of surgery, the surgeon also removes lymph nodes in the area to get an accurate staging of the cancer and to decide on further treatment after surgery.
Radiotherapy is the use of high energy x-rays given to kill cancer cells. These x-rays cause damage to the DNA of the cancer cells and thereby kill them. Radiotherapy is a local treatment and has its effect in the area that it is given to. It is given using a large machine (Linear accelerator) which generates the x-rays and delivers the treatment to the patient. This method is called as external beam therapy. The other way to give radiotherapy is to insert radioactive sources into the cancer itself. This method is called Brachytherapy and is used to treat some types of cancers.
Radiotherapy for non small cell lung cancer
Radiotherapy for non-small cell lung cancer is done mainly with external beam radiotherapy.
In stage 1 and 2 non-small cell cancer, radiotherapy is offered to patients who are not fit or don’t want surgery. Radiotherapy is given to the tumour and involved lymph nodes near the lung. A rim of normal lung tissue around the tumour is also treated, so that the target is not missed.
The treatment is given once daily for a period of up to 6 and a half weeks. Each day, the treatment lasts about 10-15 minutes.
Radiotherapy alone is used for patients with stage I cancer and a combination of radiotherapy and chemotherapy is used for patients with stage II to stage IIIB. The chemotherapy can be given along with radiotherapy at the same time (concurrent chemoradiotherapy), or if the patient is not well enough, chemotherapy can be given first followed by radiotherapy (sequential chemoradiotherapy).
Radiotherapy is also used in patients with stage I and stage II who had surgery and the tumour margins are positive (tumour not removed completely and present at the margin). Stage 4 cancers are also treated with radiotherapy, but in that setting, treatment is for a shorter duration and is aimed at controlling symptoms.
There are various technical ways of delivering radiotherapy to patients and these are listed here below.
These techniques mainly differ in the ability to maximize damage to the cancer, and limit side effects.
Some techniques are more convenient than others and there are also significant cost differences between these techniques.
3D conformal Radiotherapy
This is a way of planning and giving radiotherapy, where CT, MRI scans are used to get a three dimensional image of the tumour. This allows the planning process to be made in three dimensions.
It allows the radiation treatment to be more precise than standard 2D radiotherapy.
Intensity modulated Radiotherapy (IMRT)
IMRT is a type of conformal treatment planning and delivery method, where radiation beams can be precisely shaped to fit the shape of the tumour. This helps in minimizing toxicity to surrounding normal structures in the body. The difference between IMRT and 3D conformal radiotherapy is that IMRT can be more precisely shaped to fit the shape of the tumour. Therefore, side effects could be lesser. Also, with IMRT there is the possibility of delivering different doses of radiotherapy to different parts of the same tumour. IMRT is done by using multiple radiation beams directed at the tumour from different angles.
Arc based Treatment
Arc based therapy (Rapid Arc, VMAT) is delivery of radiotherapy with the linear accelerator going around the patient in an arc like fashion. This type of therapy can be more precise than standard IMRT.
Stereotactic body Radiotherapy (SBRT) or SABR (Stereotactic Ablative Radiotherapy)
This is a technique of radiotherapy that is used to treat early stage lung cancers. The treatment involves use of very advanced radiation planning tools and radiotherapy machines. As a result, radiotherapy delivery can be very precise, enabling the oncologist to give very high doses of radiation to the tumour. The treatment duration for lung cancer with SBRT can be very short ranging from one to two weeks as compared to 6 to 7 weeks for standard radiotherapy. SBRT is an option for some early stage lung cancer patients who are not fit or choose not to have surgery. The outcome with SBRT can be as good as surgery in that setting.
Image guided Radiotherapy (IGRT)
Image guided radiotherapy is the use of imaging systems such as x-rays or CT scanners to monitor treatment accuracy. Normally, in standard 3D conformal radiotherapy, a CT scan is done prior to start of treatment for planning purposes. In IGRT, a CT scan or x-ray can be done prior to every radiotherapy treatment to test for accuracy of the treatment.
Side effects of Lung radiotherapy
Lung cancer radiotherapy can produce side effects which usually start in about the third week of treatment. They vary in severity from patient to patient. The side effects will peak in the week after the completion of treatment and will settle a few weeks later. They are
- Tiredness
- Cough
- Breathlessness (can occur or start up to 3-6 months from end of treatment)
- Soreness in the chest
- Difficulty and painful swallowing
- Change in voice
EGFR, ALK and ROS Testing and Targeted or Biological Therapy
All patients with non-small cell carcinoma of the lung should undergo EGFR, ALK and ROS testing. This test is done on the biopsy sample and can take about 7-10 days for the results. This test is particularly useful for stage 4 patients. If any of these tests are positive, the patient can have biological therapy rather than chemotherapy. EGFR is positive in some patients with adenocarcinoma of the lung, particularly non-smokers and women. These treatments are tablets and can be very effective in controlling the cancer and reducing symptoms. They generally have less side effects than chemotherapy.
If the EGFR test is positive in stage IV patients, the first-line treatment can be Gefitinib, Erlotinib, Afatinib or Osimertinib. If ALK or ROS testing is positive, then the patient will benefit from having a drug called Crizotinib as treatment.
In patients with stage 1b to 3 cancers who have had others options of treatment such as surgery, chemoradiotherapy or radiotherapy and are known to be EGFR positive, treatment with Osimertinib is indicated as this will increase the time period where the disease is kept controlled.
Common side effects of these drugs include tiredness, skin rash, pimples on the face, chest and other areas, loose motions, nausea and vomiting, sore mouth, cough and breathlessness. Occasionally, side effects can be severe so as to need to stop the drugs. These drugs are given as long as the cancer is responding to them and is under control. A repeat biopsy is done if there is increase of cancer while on these drugs.
Antiangiogenic Drugs
Antiangiogenic drugs are antibodies that act against VEGF receptor. These drugs stop development of new blood vessels in the cancer and therefore stop the cancer from growing. Bevacizumab is one such drug that is used along with chemotherapy in lung cancer and continued as maintenance after completion of chemotherapy.
Immunotherapy
Immunotherapy in Lung Cancer is the use of drugs that enable the immune system of the patient to act on the cancer cells and kill them. These drugs are called as checkpoint inhibitors and block the PD-1 or PD-L1 receptors on the cancer cells and the cells of the immune system. The drugs used include Nivolumab, Pembrolizumab, Durvalumab and Atezolizumab.
PD-L1 Testing
For patients being considered immunotherapy for stage 4 lung cancer and some patients with other stages, testing for PD-L1 is important. This test will determine whether Pembrolizumab is going to be useful for the patient or not and whether it can be given as initial treatment or after the use of chemotherapy. This test is done on the sample of cancer obtained at biopsy.
Pembrolizumab is used in lung cancer either on its own or in combination with chemotherapy. It is used in the first line setting (first treatment option after diagnosis is made). The drug can be used on its own in patients who have a PD-L1 level of >50%. In patients where PD-L1 is >1% and less than 50%, it can be used along with chemotherapy. After completion of chemotherapy, it is used as a maintenance treatment. Atezolizumab is given along with chemotherapy, also as first line treatment.
The other drugs such as Nivolumab, Atezolizumab and Durvalumab do not need testing for PD-L1. Durvalumab is used in stage 3 lung cancer after completion of chemoradiotherapy.
Overall, immunotherapy in lung cancer is well tolerated and is usually less toxic than chemotherapy but can be associated with side effects some of which can be severe.
Other mutations observed include MET exon-14 mutation, where a drug called Capmatinib can be used and RET reaarangement, where a drug called Selpercatinib can be used. Other drugs such as Alectinib, Vandetanib and Cabozantinib may also be used in patients with RET rearrangement. Next generation gene sequencing, detailed in this website will be able to identify these genetic changes in patients with these cancers.
Chemotherapy plays an important role in the management of non-small cell lung cancer. Chemotherapy can be given at different times of the treatment pathway and these are listed in below
Neoadjuvant chemotherapy
This is when chemotherapy is given prior to definitive radiotherapy or sometimes surgery. This treatment is sometimes given in patients with stage III non-small cell lung cancer who cannot tolerate combined chemoradiotherapy. The chemotherapy given in this setting is usually a combination of drugs and is given for about 3 months.
Adjuvant chemotherapy
Adjuvant chemotherapy is use of chemotherapy after definitive primary treatment. In non-small cell lung cancer adjuvant chemotherapy is given after surgical removal of a stage IB and 2 cancers. This is usually given with a combination of 2 drugs and is given for 4 cycles. Each cycle lasts 3 weeks and the course lasts for 3 months.
Chemotherapy and Immunotherapy for Non small cell lung cancer stage 4
Patients with stage 4 non-small cell lung cancer and are EGFR, ALK and ROS negative, are treated with systemic chemotherapy and immunotherapy if available to the patient.
In patients for whom immunotherapy is not available or not affordable, treatment option is in the form of combination chemotherapy. This is a combination of two drugs. For patients with squamous cell carcinoma of the lung, treatment is given with a combination of a platinum based drug such as Cisplatin or Carboplatin and another drug such as Paclitaxel, Gemcitabine or Vinorelbine. This is given once every 3 weeks for up to 4 cycles. For adenocarcinoma, treatment is with Cisplatin or Carboplatin combined with Pemetrexed, again given for 4-6 cycles depending on response. If good response is present that is seen on CT or PET-CT scans after end of chemotherapy, Pemetrexed can be continued for as long as it works every 3 weeks.
For patients in whom immunotherapy is available and affordable, treatment options will be different and will depend on the PD-L1 status. This is a test done on the biopsy sample and will give a percentage score of the PD-L1 present in the cancer.
For those patients with a PD-L1 above 50%, treatment with an immunotherapy drug called Pembrolizumab is given. This is given as an intravenous infusion once every 3 weeks and used as long as the cancer responds and remains under control with it.
For patients with a PD-L1 status less than 50%, treatment can be in the form of chemotherapy plus immunotherapy. The chemotherapy can be similar to the one described above and the immunotherapy drug Pembrolizumab is added to that. Another option is to add another drug called Bevacizumab to the chemotherapy.
In patients with adenocarcinoma, treatment with chemotherapy such as Carboplatin, Pemetrexed as well as Bevacizumab and an immunotherapy drug called Atezolizumab is an option of treatment also.
In these patients, chemotherapy is given for 4-6 cycles and if immunotherapy or Bevacizumab is being used, these are continued as maintenance treatment.
Fir patients who have relapsed or recurred after initial treatments that have been described above, alternative chemotherapy options can be considered. Immunotherapy with Nivolumab or other drugs can be considered if they were not used the first time.
Patients whose cancers show with EGFR, ALK, or ROS positive mutations and are stage 4, will benefit from biological agents. These drugs are used as treatment instead of chemotherapy or immunotherapy. For patients who are EGFR positive, treatment with Osimertinib, Gefitinib, Erlotinib or Afatinib are options. All of these drugs are available as tablets and can work well in these patients with less side effects than chemotherapy. See section on biological therapy for more details.
Treatment of relapsed or recurrent non-small cell lung cancer
The treatment of non-small cell lung cancer that has recurred or relapsed depends on the location of relapse, the extent of recurrence, the patient’s fitness and previous treatments used.
Chemotherapy and Radiotherapy are commonly used options in this setting. The choice of chemotherapy drugs depends on previous treatments used and the patient’s general fitness levels.
There is an option of endobronchial radiotherapy or cryotherapy in this setting. As the cancer has relapsed, usually most of these treatment options are aimed at controlling the cancer symptoms rather than curing the cancer.
Immunotherapy as described above is also an option of treatment for lung cancer that was treated before and has recurred. Drugs that can be used here include Nivolumab.




