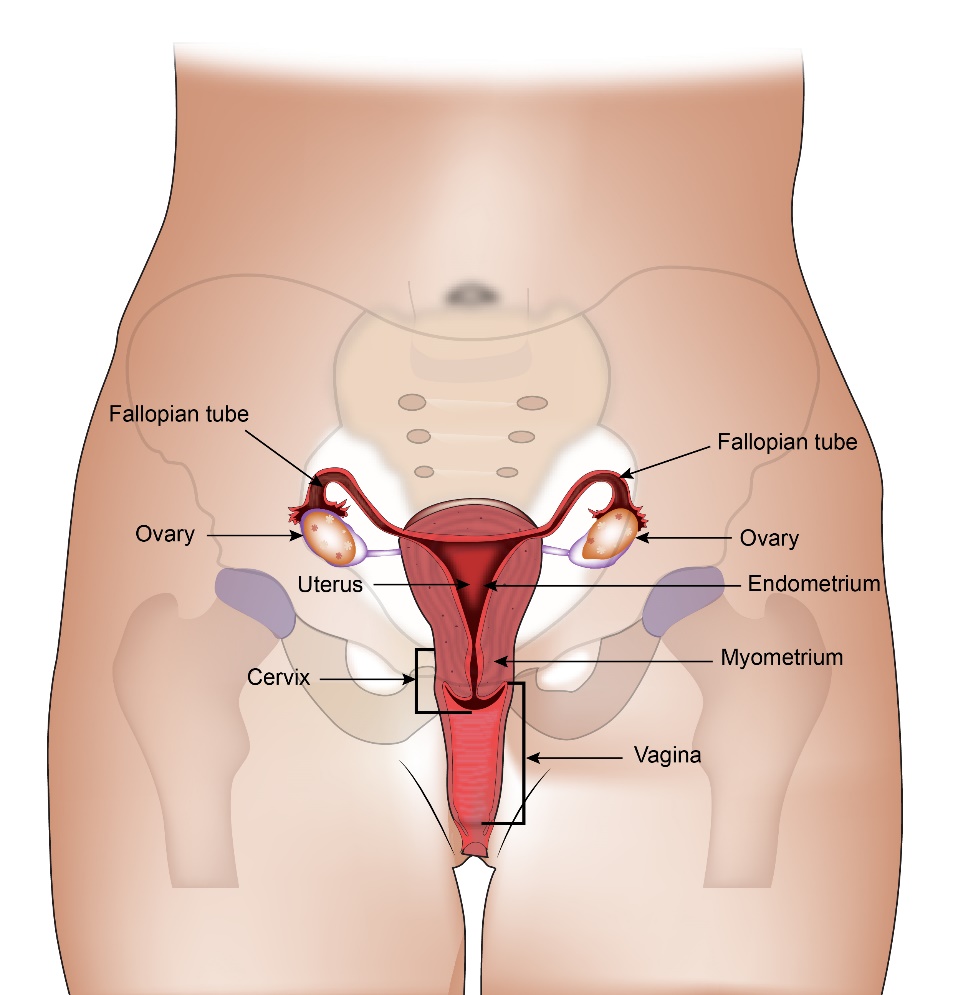
Ovaries are female reproductive organs present in a woman. There are two ovaries (right and left) present on each side of the pelvis (lower most part of the abdomen). The ovary consists of epithelial cells on the outside, germ cells and stromal cells on the inside.
The function of ovaries is to produce an egg every month in women of child- bearing age. This egg is produced in the middle of the menstrual cycle. This egg travels into the womb and can get fertilised by a sperm. The ovaries also produce hormones called Oestrogen and Progesterone which control the menstrual cycle and are responsible for the development of breasts and other body characteristics in a woman. The ovarian function begins at puberty and ends at menopause.
Ovarian cancer is cancer that has started in the ovary. Ovarian cancer can be of many types depending on which part of the ovary the cancer arises from. These are listed below in types of ovarian cancer. According to Globocan data 2018, there were 36,170 ovarian cancers in India, making up 3.1% of all cancers.
Epithelial carcinomas are the most common cancers of the ovary. They constitute about 95% of all ovarian cancers. The epithelial cancers can again be of various types. The commonest one is serous carcinoma of the ovary. This makes up about 75% of all epithelial cancers. The other epithelial cancers include mucinous, endometrioid, clear cell, mixed and undifferentiated carcinomas.
The other 5% of ovarian cancers include teratomas, dysgerminomas, endodermal sinus tumour, embryonal carcinomas, mixed germ cell tumours, choriocarcinomas and sarcomas.
The cause of Ovarian cancer is not completely known but there are some risk factors which are given below. Having a risk factor does not necessarily mean that a cancer will develop but the risk is increased when compared to others who do not have the risk factors.
Age
The risk of getting ovarian cancer increases with increasing age. 4 in 5 ovarian cancers occur in women over the age of 50.
Child bearing History
Women who never had children are at a higher risk of ovarian cancer than women who have given birth.
Hormones
Either starting periods at an early age or a late menopause increases the risk of getting ovarian cancer. Using hormone replacement therapy (HRT) slightly increases the risk. This risk is reduced again once the HRT is stopped.
Diet and Weight
Being overweight can increase the risk of getting ovarian cancer. A diet high in animal fats and less vegetables can also increase the risk.
Endometriosis
Having a condition called endometriosis can increase the risk of getting ovarian cancer.
Genetic factors
A family history of breast of ovarian cancer increases the risk of getting an ovarian cancer. About 5%-10% of all ovarian cancers are due to a genetic defect that runs in the families. This is called a BRCA mutation. BRCA1 and BRCA2 are two genes, which if abnormal increase the risk of getting breast cancer and other cancers such as Ovarian, Colon, Pancreatic and Thyroid cancers. Testing can be done for these abnormal genes if there is suspicion of hereditary cancer.
The presence of a faulty gene should be suspected if
- there is a history of ovarian cancer in two close relatives (sister, mother, daughter)
- there is a history of breast or ovarian cancer in two close relatives
- three close relatives with colon, endometrial and ovarian cancer
Protective factors for Ovarian cancers
There are some factors which can be termed as protective as they reduce the risk of getting ovarian cancers. These are
- Breastfeeding
- Having children
- Use of oral contraceptives
- Surgical removal of ovaries and fallopian tube
- Removal of uterus
Ovarian cancer may not cause any symptoms when it is in its early stages. In early stage cancer some patients may notice symptoms which include
Pain in the lower abdomen
Bloated feeling or feeling of fullness in the abdomen
Ovarian cancer in the later stages can cause a variety of symptoms. Most of these symptoms are very non-specific and can mimic common conditions. These symptoms are listed below.
- Irregular menstrual periods
- Bleeding in between periods
- Pain or a lump in the abdomen or pelvis
- Increased frequency of urination
- Constipation
- Pain during sex
- Bloated feeling or feeling of fullness in the abdomen
- Loss of appetite
- Back pain
- Swelling of abdomen or legs
- Breathlessness
If Ovarian Cancer is suspected the following investigations can be done.
Clinical Examination
A gynaecologist or Oncologist will do an examination of the pelvis. This will help detect any large masses present in the pelvis (lower most part of tummy).
Pelvic and abdominal ultrasound
An ultrasound scan of the abdomen and pelvis is good at picking up masses around the ovary or other masses in the pelvis. It is usually the first investigation after clinical examination if ovarian cancer is suspected.
Chest x-ray
A chest x-ray is done to look for presence of cancer in the lungs or the presence of fluid that can occur in the covering of the lung. An x-ray is not needed if a CT scan is being done.
CT Scan
A CT or computed tomographic scan is done when ovarian cancer is suspected or diagnosed. The CT scan uses x-rays to give detailed images of the chest, abdomen and pelvis and can show up most abnormalities that are bigger than a few millimetres. It is quick, painless and is available in most centres. It helps in staging the cancer. (give a stage to the cancer).
Blood Tests
Blood tests including CA125 are done at diagnosis. CA125 is a marker in ovarian cancer. It is elevated above normal in most ovarian cancers. CA125 can be elevated in other conditions too. In a patient with definite ovarian cancer, CA125 is used as a marker to look for response to treatment or to look for recurrence of cancer. Other blood tests that are done include complete blood picture, liver and kidney function tests.
Biopsy
If early ovarian cancer is suspected on a scan a biopsy is usually not done. The patient goes straight to surgery. This is because, there is a risk of ovarian cancer spreading to other parts of the abdomen at the time of biopsy. In patients where there is evidence of spread of cancer to other parts of the body already, a biopsy can be done to confirm the presence of ovarian cancer.
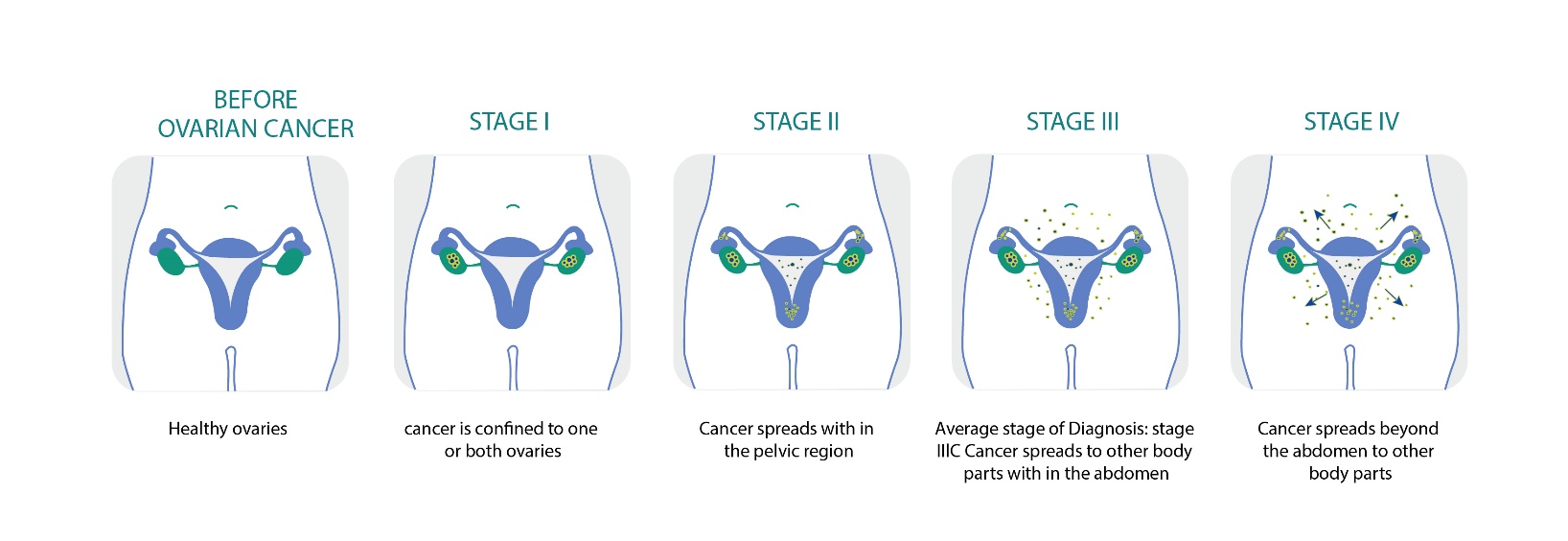
The stage of a cancer is a word used to describe the size and location of the cancer in the body. Knowing the stage of the cancer helps the doctors to decide on the most appropriate treatment.
Ovarian cancer can be divided into 4 stages from stage 1 to stage 4 depending on the extent of spread of cancer from the ovary. The staging is listed here below.
Stage 1
Stage 1 Ovarian cancer is when the cancer is confined to the ovary. This stage can be subdivided into three groups.
Stage 1a-
This is when the cancer is confined to one ovary only
Stage 1b-
This is when the cancer is present in both ovaries only
Stage 1c-
This is when the cancer is either 1a or 1b and there are cancer cells on the surface of the ovary or there are cancer cells in the fluid taken from the abdomen during surgery or the ovary has ruptured before or during surgery.
Stage 2
Stage 2 Ovarian cancer is when there is evidence of cancer spreading from the ovary into other areas in the pelvis. This can again be subdivided into three groups
Stage 2a-
This is when the cancer has spread to the uterus or fallopian tubes.
Stage 2b-
This is when the cancer has spread to areas in the pelvis other than uterus or fallopian tubes.
Stage 2c-
This is cancer at stage 2a or 2b and there is presence of cancer cells in the fluid taken from the abdomen during surgery.
Stage 3
Stage 3 Ovarian cancer is when the cancer has spread beyond the pelvis to the lining of the abdomen, the bowel or the lymph nodes in the abdomen . This stage can be subdivided into three groups.
Stage 3a-
The cancer has spread into the abdomen but is small and can only be seen under the microscope.
Stage 3b-
The cancer that has spread into the abdomen can be seen and is 2cm or smaller in size.
Stage 3c-
The cancer that has spread into the abdomen is larger than 2cm or have spread to nearby lymph nodes.
Stage 4
The Cancer has spread to other parts of the body such as liver lungs etc
Grading of cancer
Ovarian cancer is also given a grading by the pathologist when the cancer is seen under the microscope. The grading is from 1 to 3 with grade 1 being least aggressive and grade 3 being more aggressive type of cancer.
Grade 1 (low grade) – the cancer cells are growing slowly, look quite similar to normal cells (are well differentiated) and are less likely to spread than high-grade cancers.
Grade 2 (moderate grade) – the cells look more abnormal and are growing slightly more quickly.
Grade 3 (high grade) – the cancer cells are growing more quickly, look very abnormal (are poorly differentiated) and are more likely to spread than low-grade cancers.
Surgery is an important and a common mode of treatment for Ovarian cancer.
It is usually the first method of treatment after a diagnosis of Ovarian cancer is made. The type of surgery done can vary depending on the stage of the cancer at diagnosis.
The standard operation for ovarian cancer is total abdominal hysterectomy and bilateral salpingo-oophorectomy. This surgery involves an incision in the abdomen and removal of both ovaries, fallopian tubes, uterus, cervix and removal of some abdominal lymph nodes, omentum and any other cancer deposits present in the abdomen. At the time of operation, the surgeon collects a sample of fluid from the abdominal cavity for analysis. This is known as peritoneal washing.
In advanced cancer when there are lots of deposits of cancer present in the abdomen, a debulking surgery is done where the surgeon removes as much cancer as possible but not all of it.
In young women who have very early cancer (stage 1a) and wish to preserve fertility, the normal ovary and the uterus could be left behind so that she may be able to have children in the future.
Many times, chemotherapy is given before surgery. This is called as neo- adjuvant chemotherapy and is considered in patients with advanced cancer. This type of surgery which is done with chemotherapy before and after is called as interval debulking surgery. The purpose of neo-adjuvant chemotherapy is to reduce the amount of cancer present in the abdomen prior to surgery to enable near complete removal of all cancer at surgery.
Following the operation, women will be able to go home within 10 days. Once they have recovered from surgery, chemotherapy is given to most women.
Chemotherapy forms an important form of treatment for Ovarian Cancer. Chemotherapy is used in different settings for the management of this condition.
Neo Adjuvanvt chemotherapy
In patients diagnosed with advanced Ovarian cancer, chemotherapy can be given prior to surgery. This is called as neoadjuvant chemotherapy. The method of treatment is chosen in patients who may not be fit enough for surgery at the time of diagnosis of cancer or in settings when it is believed that better surgical results can be achieved after chemotherapy. This treatment is given for 3-6 months duration after which surgery is done. Common drugs used in neoadjuvant and adjuvant settings include platinum drugs such as Carboplatin and Cisplatin and Taxanes such as Paclitaxel. These can be used alone or in combination. These chemotherapy drugs are given once every 21 days for up to 3-6 cycles. In patients who are not fit, a weekly option can be used.
Adjuvant Chemotherapy
Here, chemotherapy is given after surgical removal of Ovarian cancer. This is usually the most common approach used to treat Ovarian cancer. The chemotherapy is given for up to 6 months depending on the response of the cancer to treatment and the tolerance of the patient to the treatment.
Chemotherapy in Recurrent Disease
In patients who have disease that has come back after initial surgery and chemotherapy, further chemotherapy is used to control disease. Many drugs are available for use in this setting and have a good effect in control of cancer and improve symptoms. For patients whose disease has recurred more than 6 months after completion of initial chemotherapy usually have a repeat of the platinum drug. For others, a different drug or drugs are used.
Common drugs used in this setting include Gemcitabine, Topotecan, Liposomal Doxorubicin, Bevacizumab and Etoposide.
Targeted Therapy
Olaparib and Niraparib are drugs that are used in patients who have ovarian cancer due to genetic mutations such as BRCA1 and BRCA2. They are given by mouth as tablets and can be given as maintenance treatment after chemotherapy in patients with and without BRCA mutations.
Bevacizumab is a monoclonal antibody that stops the growth of new blood vessels in the cancer. It is effective in Ovarian cancer and is given in combination with chemotherapy or on its own.
Symptom Management
In patients with recurrent Ovarian cancer, one symptom that is commonly present is the development of Ascites (fluid) in the abdomen. This can be removed by putting a tube into the abdomen and can be done repeatedly if needed. Some centres may place a catheter in the abdomen for continuous drainage with which the patient may be able to go home.
Intraperitoneal Chemotherapy (IP)
Intraperitoneal chemotherapy is the administration of chemotherapy directly into the space of the abdomen. This type of chemotherapy options is for patients who have stage 3 Ovarian cancer and had good debulking surgery, where only limited amount of disease is present in the abdomen after the operation. A catheter or a tube is placed at or after surgery into the abdomen and chemotherapy with Carboplatin and/or Paclitaxel can be given into the abdomen. Some studies have shown that giving chemotherapy this way may work better than when given into the vein. Not all patients are suitable for this treatment and it not commonly used.




