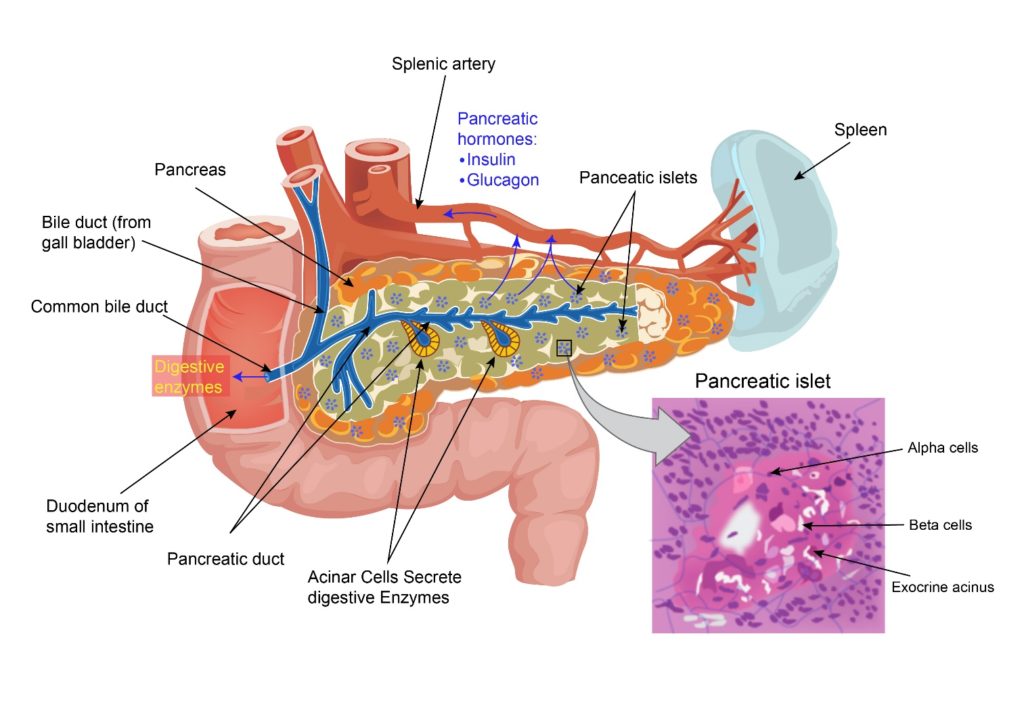
Pancreas is a gland present at the back of the abdomen behind the stomach. It is a leaf shaped organ which is made up of a wide area called the head, a body in the middle and a thin part on the other end called the tail. The head of the pancreas is surrounded by the duodenum which is the first part of the small intestine. The pancreas produces digestive enzymes which help digest food. It also produces insulin which controls the glucose level in the blood. The digestive enzymes produced by the pancreas are secreted into the duodenum. The pancreas also produces other hormones which are released into the blood and help with growth, metabolism and hunger.
Cancer that starts in the Pancreas is called pancreatic cancer. There are different types of Pancreatic cancer. The most common type is called as ductal adenocarcinoma which arises from the lining of the ducts present in the Pancreas. The other types are cystic carcinomas and acinar cell carcinomas which are uncommon. Sarcomas and Lymphomas also occur and are rare. According to Globocan data 2018, there were 10,860 patients diagnosed with Pancreatic cancer in India making up 0.94% of all cancers Other type of Pancreatic cancers which are rare originate from the hormone producing cells of the Pancreas and are called as neuroendocrine tumours of the pancreas (pNET’s). These are Gastrinomas, VIPomas, Insulinomas, Glucagonomas and Somatostatinomas.
There are various possible risk factors for Pancreatic cancer. These are
Age
Pancreatic cancer is usually a disease of older age and risk tends to increase as age progresses.
Tobacco Use
People chewing or smoking tobacco increase their risk of getting Pancreatic cancer. Overall about 20-30% of Pancreatic cancers can be linked to tobacco use.
Obesity
Increased obesity and reduced exercise have been linked with Pancreatic cancer.
Diet
A diet high in processed meat and red meat increases the risk of Pancreatic cancer.
Alcohol
Drinking alcohol in large amounts tends to increase the risk of getting Pancreatic cancer.
Chronic Pancreatitis
Chronic pancreatitis is a condition where there is repeated inflammation of the pancreas. This manifests in the form of abdominal pain and other symptoms. Chronic pancreatitis happens for various reasons including rarely a hereditary form.
Diabetes
Diabetes is a known risk factor for pancreatic cancer.
Genetic risk factors
Genetic factors only account for 5-10% of pancreatic cancers.
People with a faulty BRCA2 gene have a higher risk of Pancreatic cancer. This faulty gene is implicated in Breast and Ovarian cancer too.
People with HNPCC (Hereditary non-polyposis colon cancer) have an increased risk of Pancreatic cancer. Other conditions associated are Peutz-Jeghers syndrome and FAMM syndrome.
Symptoms of Pancreatic Cancer include
Jaundice
Jaundice is yellowish discolouration of the skin and eyes. This can be a presenting symptom in pancreatic cancer and is usually painless. This symptom happens due to blockage of the duct (bile duct) that transports bile from the gall bladder into the duodenum.
Pain
Pain is a common presenting symptom in pancreatic cancer. The pain can be dull aching type and can be present in the back or front of the upper abdomen. Pain may be worse on lying down and relieved by sitting up and can be worse after food.
Weight Loss
This is also a common symptom seen in advanced pancreatic cancer. This can be associated with a normal or reduced appetite.
Other Symptoms
Other symptoms associated with pancreatic cancer include loose motions, feeling of bloating of the stomach, vomiting and nausea.
Investigations for Pancreatic cancer are generally done based on the presenting symptoms.
Blood Tests
Blood tests including complete blood picture, electrolytes, creatinine and urea, liver function tests and clotting tests are the standard tests along with CA19.9 which is s specialised blood test done once a diagnosis is made.
US Abdomen
An ultrasound scan of the abdomen particularly the biliary tract is done first in patients presenting with jaundice. This scan will look for evidence of obstruction of the bile duct. Obstruction of the bile duct can also happen for reasons other than cancer such as gall stones etc. If the ultrasound shows a suspected cancer, then further tests are needed.
CT Scan
A CT scan of the abdomen with a Pancreatic protocol is an important test in the diagnosis of Pancreatic cancer. It helps identify a tumour mass present within the Pancreas and can aid in the biopsy of the abnormal mass. The CT scan that is done here is a triple phase CT scan which is specific to diagnose this condition
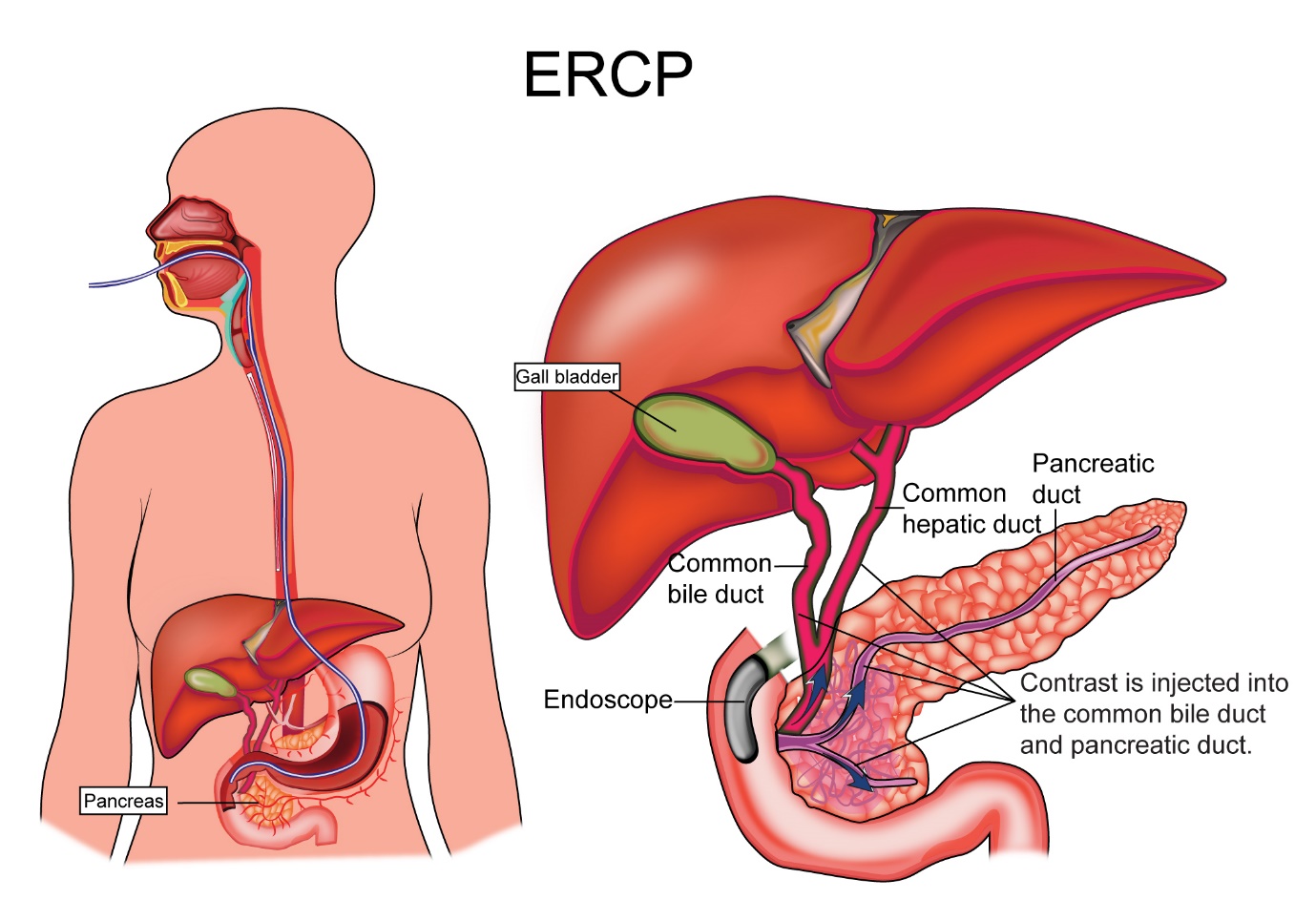
ERCP
An ERCP is endoscopic retrograde cholangio-pancreatography, a procedure where a gastroenterologist passes an endoscope (narrow tube passed into the stomach) into the duodenum and from there gains access into the opening of the common bile duct through which the bile and the pancreatic enzymes drain into the duodenum. Once access is gained into this duct, the cause for the blockage of the duct is found and by injecting a dye and taking x-ray pictures. If cancer is found or suspected, a biopsy can be taken from the site. This procedure is done under sedation. A stent may be placed sometimes to keep the duct open. This helps relieve the jaundice.
MRI
An MRI scan is sometimes done to investigate pancreatic cancer. An MRCP is magnetic resonance cholangio-pancreatography can give the same information as an ERCP about possible causes of bile duct blockage but a biopsy cannot be done, or a stent cannot be placed as this is a non-invasive test.
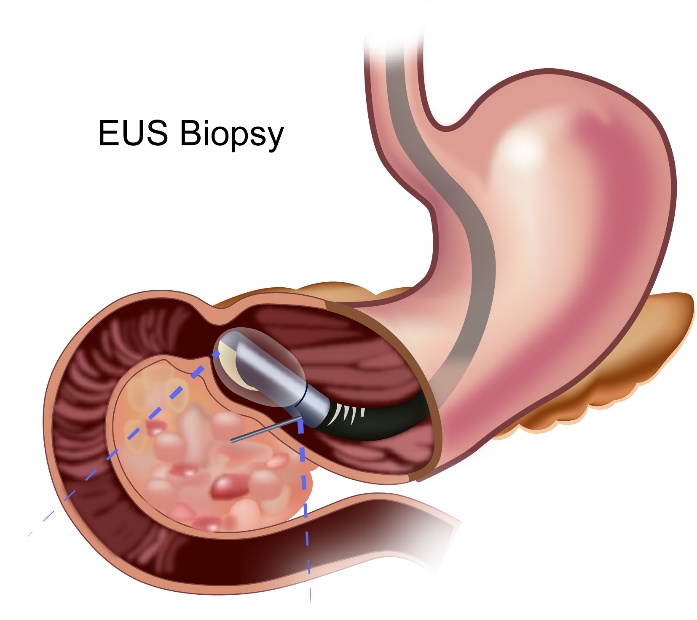
EUS
An EUS is endoscopic ultrasound where an endoscope is inserted into the gullet and stomach. The endoscope has a small ultrasound probe attached to it which helps get an ultrasound image from the inside. This test helps in getting clearer images of small masses or lymph nodes present in the area. The test also guides the doctor to take biopsies accurately.
Staging Laparoscopy
A staging laparoscopy is a test where a laparoscopic procedure is done prior to definite surgery to remove the pancreatic cancer. A laparoscopic procedure involves placing small cuts on the abdomen and inserting long tubes into the abdomen through these cuts. These tubes have a light and camera source attached to them and the doctor can have a look inside the abdomen with them. This procedure is done in some patients prior to definitive operation to exclude any spread of tumour from the Pancreas to other parts of the abdomen.
PET-CT
A PET-CT scan is not routinely recommended as a standard investigation for pancreatic cancer but can sometimes be used in addition to standard CT discussed above.
Biopsy
A biopsy is not always done prior to surgery if all investigations suggest definite Pancreatic cancer. It is recommended though in advanced tumours when other forms of treatment such as chemotherapy or radiotherapy are planned prior to surgery. A biopsy can be done with the help of ERCP or EUS or CT guided. Some clinicians advocate a biopsy prior to any treatment.
The stage of a cancer is a term used to describe the size and location of the cancer in the body.
Knowing the stage of the cancer helps the doctors to decide on the most appropriate treatment. Pancreatic cancer is staged based on the TNM staging system or the number system.
Staging with either system is based on the extent of the tumour in the gallbladder, the spread of the cancer into the lymph nodes, and spread of cancer into other parts of the body.
TNM stands for Tumour, Node and Metastases. T stands for tumour and in gallbladder cancer represents depth of spread into the wall of the gallbladder. N stands for nodes and spread of cancer into nodes. M stands for metastases and spread of cancer to distant sites in the body.
T stage
| T1 | Tumour less than or equal to 2cm in maximum size |
| T1a | Tumour up to 0.5cm in maximum size |
| T1b | Tumour more than 0.5cm and less than 1cm in maximum size |
| T1c | Tumour more than 1 and less than 2cm in maximum size |
| T2 | Tumour more than 2 and up to 4cm in size |
| T3 | Tumour more than 4cm in maximum size |
| T4 | Tumour involves other structures such as coeliac axis, superior |
mesenteric artery and/or common hepatic artery
N Stage
| N0 | No regional lymph node involvement |
| N1 | Spread of cancer to 1-3 lymph nodes |
| N2 | Spread of cancer into 4 or more lymph nodes |
M Stage
| M0 | No distant metastasis |
| M1 | Distant metastasis |
Treatment of Pancreatic cancer depends on the stage of cancer at diagnosis and the fitness of the patient. The options of treatment include Surgery, Radiotherapy, Chemotherapy.
Surgery is the treatment of choice in a patient with a cancer that is operable. This will be determined on the results of the scan. In instances where the status is borderline as to whether surgery is possible or not, other options such as Chemo-Radiotherapy or Radiotherapy or Chemotherapy may be used first.
If surgery is not an option of treatment, then other options are considered as discussed in the relevant sections.
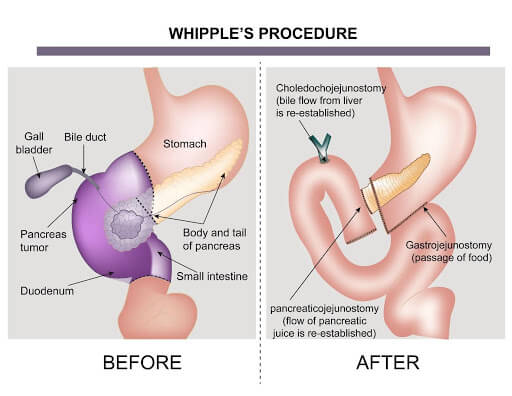
Surgery for pancreatic cancer is a curative treatment option in early Pancreatic cancer. It is done when the surgeon is confident of being able to remove all the disease seen on investigating scans. The surgery involves removal of the part of the pancreas along with the duodenum, gall bladder, bile duct and surrounding lymph glands. This operation is called pacreatico-duodenectomy or whipple’s procedure. This operation is done in patients with cancer in the head of the pancreas. Sometimes, the whole pancreas needs to be removed and this procedure is called a total pancreatectomy.
If the tumour is present at the tail of the pancreas, a distal pancreatectomy is done where the tail and part of the body of the pancreas is removed. The surgeries can be done as open surgery (large incision on the abdomen) or as a minimally invasive technique such as laparoscopy or robotic assisted laparoscopic surgery.
Following surgery, supplementation of digestive enzymes and insulin may be needed.
In some patients, a staging laparoscopy is done prior to going for surgical removal of Pancreatic cancer to exclude any spread of tumour from the Pancreas to other parts of the abdomen. This procedure helps see small areas of cancer that can be present in the abdomen and are not seen on the scans. A laparoscopic procedure involves placing small cuts on the abdomen and inserting long tubes into the abdomen through these cuts. These tubes have a light and camera source attached to them and the doctor can have a look inside the abdomen with them to exclude any spread of tumour from the pancreas to other parts of the abdomen.
Surgery is sometimes needed in patients with very advanced pancreatic cancer where there is blockage of the intestine(duodenum) due to tumour compressing on it or tumour growing into it. Here surgery is used to bypass the blockage. This type of surgery is used to improve symptoms only and is not aimed to remove the cancer completely.
Boderline Resectable Pancreatic Cancer
Some pancreatic cancers may not be resectable or operable at the time of diagnosis as there may be a s=risk of not getting clear margins at surgery. These are called as borderline resectable pancreatic cancers. Here other treatments such as chemotherapy, radiotherapy or chemo-radiotherapy may be given prior to surgery to make the cancer resectable. Once they become resectable, the above mentioned surgeries can be done.
Radiotherapy either alone or in combination with chemotherapy (chemo-radiotherapy) is an option of treatment for patients with locally advanced cancer or when patients have early pancreatic cancer but are not medically fit to undergo surgery. Curative surgery is not done in advanced cancer when there is involvement of major blood vessels or other structures by cancer which cannot be removed by surgery.
In the above situation, radiotherapy or chemo-radiotherapy is given over 5-6 weeks with the aim of getting rid of the cancer completely. In some situations, this option is used to help shrink the cancer down to make it operable. This type of treatment is called as neo-adjuvant chemo-radiotherapy.
In patients with very advanced or metastatic pancreatic cancer, radiotherapy is used to control symptoms such as pain, bleeding, blockage in the intestine or other symptoms. Here the treatment is given over a shorter period ranging from one day to three weeks. This type of treatment is called as palliative radiotherapy.
Chemotherapy is used in multiple settings in the treatment of pancreatic cancers. It may be used prior to definitive surgery to increase the chances of getting clear margins at surgery in select patients. It is recommended after surgery in patients who did not have chemotherapy prior to surgery. This type is known as adjuvant chemotherapy and is given for up to 6 months.
For patients who have borderline resectable disease, which means there is a doubt as to whether clear margins at surgery are achievable or not, chemotherapy first or chemoradiotherapy combination can be used as treatment.
In patients with locally advanced disease not suitable for surgery, chemotherapy is used initially for 3 months and then followed up by the same treatment for another 3 months or use combination of chemotherapy and radiotherapy. Which option to select will depend on the patient’s condition and choice.
In patients with stage 4 cancer, chemotherapy remains the mainstay of treatment in controlling the pancreatic cancer and to improve symptoms and survival of the patient.
When chemotherapy is used, the choice of drugs is dependent on the stage of cancer, the age and fitness of the patient and patient choice.
For patients who are young and fit, chemotherapy with FOLFIRINOX is an option which is a combination of Oxaliplatin, Irinotecan and Fluorouracil. This is given once every 14 days. For patients who are less fit, a combination of two drugs are used which can include Oxaliplatin or Irinotecan with Fluorouracil or Capecitabine. Gemcitabine and Nab Paclitaxel is another option. For elderly patients, treatment with a single drug is an option.
Genetic studies on the biopsy sample for BRCA or PALB mutations or mutations on the homologous recombination repair (HRR) can help decide on the best chemotherapy drugs to select in patients with stage 4 pancreatic cancer. These types of genetic tests can be accomplished with next generation gene sequencing tests.
Immunotherapy with Pembrolizumab can be used in patients with microsatellite instability (MSI-H).
Patients with BRCA mutations can benefit from PARP inhibitor drugs such as Olaparib after completion of chemotherapy.
Supportive Therapy
Pancreatic cancer can cause various symptoms or issues that may need to be dealt specifically. Some of these are listed below.
Jaundice
Jaundice is a common symptom associated with pancreatic cancer. This usually happens due to blockage of the bile duct leading to accumulation of bile. Jaundice is more common in carcinomas of the head of the pancreas. This jaundice can be managed by placing a stent(tube) through the blockage and this allows the bile to flow again. The stent can be placed by ERCP (Endoscopic retrograde cholangio-pancreatography) or PTC (percutaneous transhepatic cholangiopancreatography).
Pain
Pain is a common symptom in advanced pancreatic cancer. Apart from pain killing medications, radiotherapy is used as an option to control pain.
Coeliac plexus block is a procedure where nerves present close to the pancreas are damaged by injecting alcohol into the nerves. This stops the nerves from sending pain signals to the brain thereby improving the pain.




