Testes or testicles are male reproductive organs. There are two testes in the male, right and left, and are present in the scrotum. The scrotum is present below the penis. The testes produce a hormone called testosterone. Testosterone enables the development of male characteristics such as the growth of face and body hair, deep voice, and development of muscle. Testes also produce sperm. The sperm that is produced in the testes are transferred into the urethra through a tube called the epididymis and the spermatic cord.
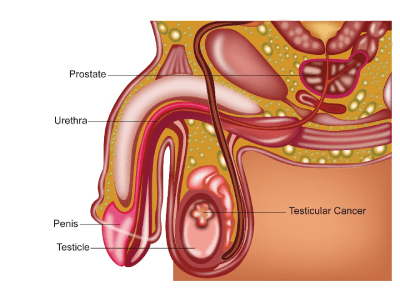
Cancers that start in the testes are called as testicular cancers. The two main types of testicular cancers are seminoma and non-seminomas. These are also called germ cell tumours. Rare forms of testes cancers include lymphomas and other para testicular cancers such as adenocarcinoma.
Testicular cancers are common in young people from the age of 25. They are the most common form of cancer in males aged 25-35 years. Testicular cancers can also occur in older males at the ages of 55 to 65. According to the Globocan 2018 data, there were 4414 testicular cancers in India making up about 0.4% of all cancers.
Testicular cancers can be of many types and are listed below. The majority of testicular cancers are germ cell tumours. These can be cancers or benign tumours.
Germ cell tumours can be divided into different categories and include
- Seminomas
- Teratomas
- Mixed germ cell tumour
- Spermatocytic seminoma
Teratomas can be classified into mature teratoma, immature teratoma, embryonal carcinoma or yolk sac tumour. There can be a mixture of these substitutes in one tumour.
Non-Germ cell tumours that occur in the testis are rare and can include
- Sarcomas
- Lymphomas
- Sex cord/Leydig cell tumours
Testicular cancer is associated with some risk factors which increase the risk of getting such a cancer. These include
Undescended Testes
There is an increased risk of testicular cancer in people who have undescended testes. This is a condition where the testes have not fully descended into the scrotum by the time of birth or after. This risk is minimised if surgical correction of the undescended testes is done by the age of 2 years.
Family History
Patients with a family history of testicular cancers have a small increased risk of getting one. About 2% of all testicular cancers occur in patients with a family history such as father, brother etc.
Genetic Conditions
Patients with genetic conditions such as Klinefelter’s syndrome, Down’s syndrome are at an increased risk. This is likely due to subnormal development of the testes in these patients.
Testicular cancer can present in many ways and the common presenting symptoms are given below.
Lump or swelling in the testes
This is a very common presenting symptom. A feeling of a lump in the testes that is gradually increasing in size. The lump can be painless or painful and is usually not separate from the testes. Sometimes, there is a history of trauma to the testes prior to the lump being noticed.
The lump can be small or large and most lumps in the testes are not cancer. It is important though to have the lump examined by a doctor.
Pain in the testes or scrotum
This can also be a symptom for testicular cancer. Again, only a small proportion of patients with a painful testis have cancer.
Other Symptoms
Other uncommon symptoms that can be seen in testicular cancer include swelling in the legs, cough, breathlessness, swelling in the abdomen, weight loss, infertility, lumps in the neck or difficulty in swallowing. These symptoms are due to spread of cancer from the testes to areas of the chest or abdomen.
When a testicular cancer is suspected, the following investigations are considered.
Ultrasound scan of the scrotum
An ultrasound scan of the testes and scrotum will be able to determine whether the lump in the testes is solid or filled with fluid. Lumps that contain fluid are less likely to be due to cancer. The scan also tells whether the lump in the scrotum is from the testes or other areas in the scrotum.
Blood Tests
Tumour markers are blood tests that are done to check for the presence of cancer. Tumour markers can be raised in certain testicular cancers and therefore these tests are done in all patients who are suspected of having such a cancer. The commonly measured tumour markers are Alfa feto protein (AFP), B Human Chorionic gonadotrophin (b HCG) and LDH. Apart from tumour markers, routine blood tests to assess liver, kidney function are done.
Orchidectomy
An orchidectomy is a surgical operation where the testis is removed. This is done when the above investigations along with clinical examination show the presence of a testicular cancer.
When this cancer is suspected, a biopsy is usually NOT done as this can raise the risk of spread of cancer and therefore surgery is done without biopsy. At operation, a prosthesis (false testis) can be placed in the position of the removed testis.
Staging tests after diagnosis is made
Staging refers to a process that helps to find out whether the cancer has spread from its site of origin to other parts of the body.
Chest X-ray
An x-ray of the chest is done to look for spread of the cancer into the chest.
CT Scan
A CT scan of the chest abdomen and pelvis with contrast is done to stage a patient who is suspected of having an advanced testicular cancer. The scan will give information about whether the cancer has spread to other areas in the body or not and this determines whether further treatment is needed after an orchidectomy is done.
PET CT Scan
A PET CT scan is generally not recommended for initial staging of testicular cancer but is useful in situations when there is concern of spread of the cancer into other parts of the body.
Testicular cancers are staged by the TNM and number staging systems and are listed below. Here the level of tumour markers are also used to determine staging.
T Stage
| T1 | Tumour confined to the testis without lymphovascular invasion |
| T1a | Tumour smaller than 3 cm |
| T1b | Tumour 3 cm or bigger in size |
| T2 | Tumour confined to testis with lymphovascular invasion ortumour invading tissues around the testes |
| T3 | Tumour invades spermatic cord with or without lymphovascular invasion |
| T4 | Tumour invades scrotum with or without lymphovascular invasion |
Clinical N
| cN0 | No regional lymph node metastasis |
| cN1 | Metastases in a single or multiple lymph nodes not more than 2cm |
| cN2 | Metastasis in a single lymph node or multiple nodes more than 2cm in size and less than 5cm in size |
| cN3 | Metastasis with a lymph node mass larger than 5 cm in size |
Pathological N
| pN0 | No lymph node metastasis |
| pN1 | Metastases in a single or multiple lymph nodes not more than 2cm,multiple nodes not more than 5 |
| pN2 | Metastasis in a single lymph node or multiple nodes more than 2cm in size and less than 5cm in size, or more than 5 nodes or extension of disease outside the lymph nodes |
| pN3 | Metastasis with a lymph node mass larger than 5 cm in size |
Metastasis (M)
| M0 | No distant metastases |
| M1 | Distant metastases seen |
Serum markers (S)
| S0 | Tumour marker levels within normal limits |
| S1 | LDH <1.5 x N and B-hCG (mIU/mL) <5000 and AFP (ng/mL) <1000 S2 LDH 1.5-10 x N or B-hCG (mIU/mL) 5000-50,000 or AFP (ng/mL) 1000- 10,000 S3 LDH >10 x N or B-hCG (mIU/mL) >50,000 or AFP (ng/mL) >10,000 |
The number staging system is as follows
Stage 1 Cancer
Stage 1 cancer is one when the cancer is limited to the testis and has not spread outside the testis. Every stage is given an ‘S’ depending on whether tumour markers remain elevated after orchidectomy or not. If tumour markers are elevated, then it will be stage 1S.
Stage 2 Cancer
Stage 2 cancer is one where there is spread of cancer out of the testis into the lymph nodes of the pelvis or abdomen. Stage 2 can again be divided into 2A,2B and 2C depending on whether the N staging above is N1, N2 and N3 respectively.
Stage 3 Cancer
Stage 3 is when there is lymph node involvement beyond the abdomen or involvement of other organs by the cancer or higher levels of tumour markers in the S2 and S3 category.
Testicular cancers are treated with options of surgery, chemotherapy and radiotherapy.
Surgery
Orchidectomy
Surgical management of testis cancer involves removal of the whole of the testis containing the cancer and this procedure is called an orchiectomy or orchidectomy. Here, an incision is made in the groin area to remove the testis. At the time of surgery, a prosthesis can be put in place of the testis that is removed. In early testicular cancers, an orchidectomy is the only operation that is needed.
Lymph node dissection
In some countries, an orchidectomy is the only operation done when there is no disease seen outside the testes. In other countries, an orchidectomy and lymph node removal for the abdomen is done. Your doctor will explain as to which operation is planned.
In patients with enlarged lymph nodes in the abdomen that do not reduce in size after chemotherapy or radiotherapy, surgical removal of lymph nodes can be considered.
This procedure is called as retroperitoneal lymph node dissection and is not needed in patients who have early testicular cancers or those in whom the lymph nodes are not enlarged anymore after treatment.
Other areas
Sometimes, surgery is done to remove lymph node masses from other areas in the body that have not reduced with chemotherapy or radiotherapy.
Other treatments like chemotherapy or radiotherapy may be needed after surgery depending on stage of cancer and this is discussed in their respective sections.
Chemotherapy
Chemotherapy is commonly used in management of testicular cancers. Here chemotherapy is aimed to control and cure the disease. The need for chemotherapy and the choice of drugs used depends on the type of testicular cancer and the stage of the cancer at diagnosis.
Seminoma
Chemotherapy is used in treatment of seminomas. The drugs commonly used in seminomas include Carboplatin, EP or BEP chemotherapy regimens. BEP regimen consists of drugs Bleomycin, Etoposide and Cisplatin. The dugs selected depends on the stage of seminoma and the patient’s general condition and preferences. In early stage seminomas, chemotherapy is considered after surgery and in advanced stages, chemotherapy can be used as a first treatment.
Non-Seminoma Cancers
Cancers other than seminomas are called as non seminomatous germ cell tumours. The treatment options of these tumours depend on the stage of cancer at diagnosis. In early cancers, the use of chemotherapy is not required and only surgery is enough, where as in more advanced cancers chemotherapy is definitely used. The commonly used chemotherapy option here is BEP as described above. Up to 4 cycles are usually given.
Radiotherapy for Testicular Cancers
Radiotherapy is used to treat certain testicular cancers. This treatment is given after completion of surgery.
Seminoma
Radiotherapy can be used as an option of treatment in stage 1 and 2 seminomas. In testicular cancers, usually there is a choice whether to use chemotherapy or radiotherapy in early stages after surgery as both options can help cure the condition. The options can be discussed with the doctor before a decision is made.
Non Seminoma Cancers
Radiotherapy is not usually considered for treatment of non seminomatous germ cell tumours. Here chemotherapy after surgery is the preferred treatment option.
Treatment of Seminoma
Treatment of Seminoma is determined by the stage at diagnosis. Most patients who have a diagnosis of seminoma usually have an orchidectomy as a first step in treatment. This may be with or without a lymph node dissection. Further treatment is determined mainly by stage.
Stage 1 Seminoma
Stage 1 seminoma is a highly curable disease and further treatment following surgery is not always necessary. The following options are considered as options of treatment.
Surveillance is an option where no further treatment is given after surgery and the patient is just regularly seen in the clinic. This is usually frequently up to every 1-2 months in the first two years and less frequently after that along with the use of chest x-rays and CT scan. This option is as good as the other options described below providing the patient sticks to the plan of regular visits to the doctor.
Chemotherapy with 1 cycle of carboplatin is another option of treatment in this stage of cancer. Here one dose of Carboplatin chemotherapy is given to the patient. Potential side effects of this chemotherapy include effect on fertility in young patients, low blood counts and risk of infection, nausea and vomiting, constipation and tiredness.
Radiotherapy is another option of treatment in this stage. Treatment is to target the paraaortic lymph node region and is for 10 days duration and potential side effects include tiredness, small risk of reduced fertility.
Which option to select will depend on the pros and cons of these treatments, the age of the patient and the wishes of the patient.
Stage 2 Seminoma
Patients with stage 2 seminoma may be treated with radiotherapy or chemotherapy after their surgery. Depending on which stage 2 the disease is, chemotherapy can be with single agent Carboplatin or combination chemotherapy with Etoposide and Cisplatin or Carboplatin. Single agent Carboplatin can be combined with radiotherapy as described in stage 1.
Stage 3 and 4 Seminoma
Patients with stage 3 seminoma are treated with combination chemotherapy
Treatment of Teratoma or Non Seminomatous Germ Cell Tumours
Patients with these tumours are treated with combination chemotherapy after surgery depending on the stage of the disease at surgery and the levels of tumour markers such as B-HCG, AFP and LDH after surgery.
Stage 1 Teratoma
Patients with stage 1 teratoma can be treated with surveillance or chemotherapy depending on the presence or not of vascular invasion seen in the pathology sample after surgery. In the absence of vascular invasion, stage 1 tumours may just need surveillance and close follow up rather than chemotherapy. Those with vascular invasion will benefit from 2 cycles of chemotherapy with BEP regimen. BEP consists of drugs Bleomycin, Cisplatin and Etoposide. This is given for 5 days every 3 weeks. Surgical staging with retroperitoneal lymph node surgery or surveillance are also options.
Metastatic Teratoma
Patients with advanced teratoma are usually treated with combination chemotherapy with BEP regimen. This is for 3 or 4 cycles, each cycle lasting for 21 days. The chemotherapy is given for 5 days in each cycle and can also be given over 3 days (3 day BEP). These tumours are very curable with this chemotherapy. Toxicity or side effects of chemotherapy include tiredness, hair loss, low blood counts, risk of infection, vomiting, loose motions, reduced fertility, lung damage.
Relapse or Recurrent or Resistant Disease
For patients with seminoma or teratoma who have disease that has not resolved with initial treatment, or those whose disease has recurred, are treated with chemotherapy regimens such as VIP or TIP. High dose chemotherapy with stem cell support is also considered.
Bleomycin Lung Toxicity
Bleomycin forms part of BEP chemotherapy regimen. This drug can cause long term damage to the lung in some patients and hence the lung function should be monitored closely while on this treatment. Symptoms associated with Bleomycin toxicity include dry cough and breathlessness. Also, this drug is not given to patients who have pre existing lung disease or are smokers.
Sperm Banking
For young males due to have chemotherapy and or radiotherapy for testicular cancers, sperm banking is advised as infertility can be a side effect, particularly with chemotherapy. Sperm banking is a process where the sperm of the patient is stored prior to the patient receiving chemotherapy.




