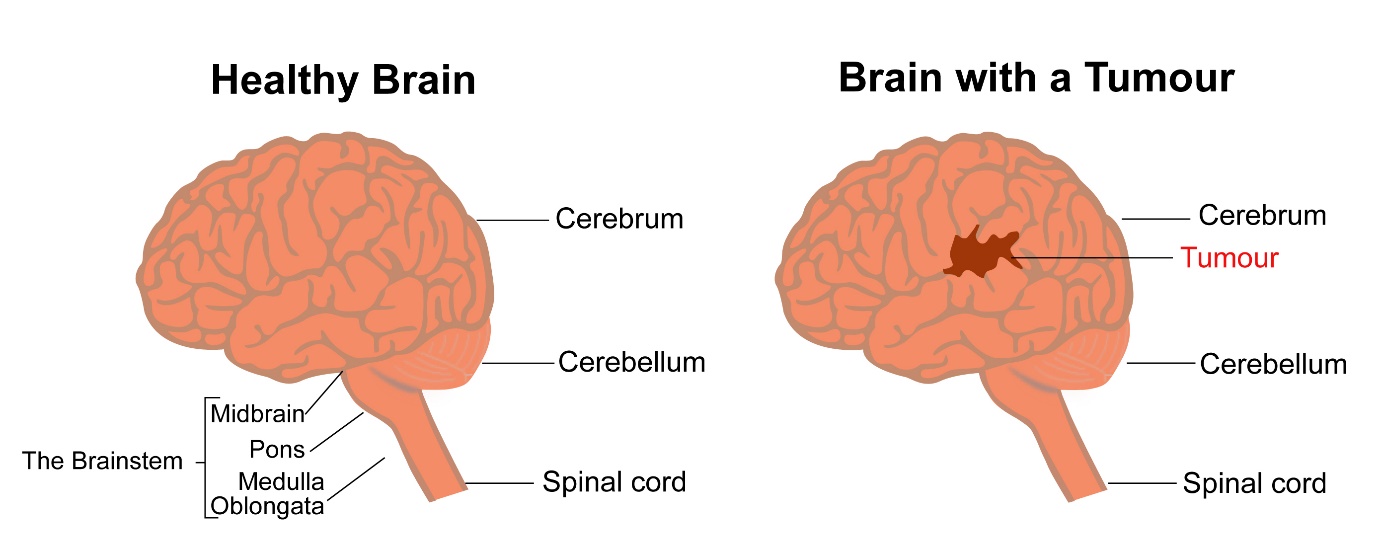
The brain is an organ present in the skull and forms the main part of the nervous system. The brain consists of the Cerebrum, Cerebellum, Midbrain, Pons and Medulla among other parts. The brain can be divided into right and left cerebral hemispheres or halves. The function of the brain is to control all the functions in the body including those under our control and those not.
Brain tumours are tumours or cancers that are present in the brain. Primary brain tumours are those that have started in the brain. Primary brain tumours can be benign or malignant. The benign tumours are not cancerous, which mean they do not have the capacity to spread to other parts of the body. Malignant brain tumours have the capacity to spread to other parts of the brain or body. Secondary brain tumours are those cancers that have started in other parts of the body and spread to the brain. In this section we will be talking only about Primary tumours. Secondary brain cancers are discussed in a separate section.
Primary brain tumours are of various types. These types are classified based on the cell of origin in the brain. The different types of brain tumours are listed below. Please select on them for details about each tumour.
- Meningiomas
- Low Grade Gliomas
- High grade Gliomas
- Lymphomas
- Acoustic Neuroma
- Medulloblastoma
- Pituitary Tumours
- Pineal Tumours
- Spinal Tumours
Primary brain tumours are of various types. These types are classified based on the cell of origin in the brain. The different types of brain tumours are listed below.
Meningiomas
Meninges are outer coverings of the brain. There are three layers of meninges and are called Dura, Pia and Arachnoid. The dura is the outermost cover and the arachnoid the inner most.
Meningiomas are tumours that develop from the meninges and form about 25% of primary brain tumours. Meningiomas are more common in the elderly population and more common in females than males. Meningiomas are usually benign tumours. They can occasionally be malignant.
Low Grade Gliomas
Gliomas are tumours that develop from the glial cells of the brain. There are different types of glial cells. Astrocytomas develop from astrocytes, oligodendrogliomas from oligodendroglial cells, mixed gliomas contain astrocytes and oligodendroglial cells, epndymoma from ependymal cells etc. Low grade gliomas are those gliomas that have a slow growth pattern. Low grade is established based on its behaviour and the look of the tumour under the microscope after biopsy or on the appearance on an MRI scan. Grading levels are given to these tumours. Those given grades 1 and 2 based on biopsy are called as low grade gliomas.
High grade Gliomas
High grade gliomas also arise from glial cells such as astrocytes, oligodendroglial cells and ependymal cells. Their behaviour unlike low grade gliomas, is more rapid and aggressive. The diagnosis of high grade glioma is established based on features on scans, and on biopsy.
Grading levels are given to these tumours. High grade gliomas are grade 3 and 4. A grade 4 glioma is called as a Glioblastoma.
Lymphomas
A lymphoma is a cancer of the lymphatic system. Lymphomas can occur in any part of the body. A lymphoma that starts in the brain is called a primary CNS lymphoma. The behaviour and treatment of this type of lymphoma is entirely different to that of lymphomas in other parts of the body.
Acoustic Neuroma
Acoustic neuromas are tumours that originate on the acoustic nerve in the brain. Acoustic nerve is associated with hearing and balance. This is a benign tumour and grows very slowly. It is also called a Schwannoma.
Medulloblastoma
A medulloblastoma is a malignant tumour that develops from cells that were associated with development of the body at a very early stage. It is a common brain tumour in young children but a rare tumour in adults. It is also called as a primitive neuro ectodermal tumour (PNET).
Pituitary tumours
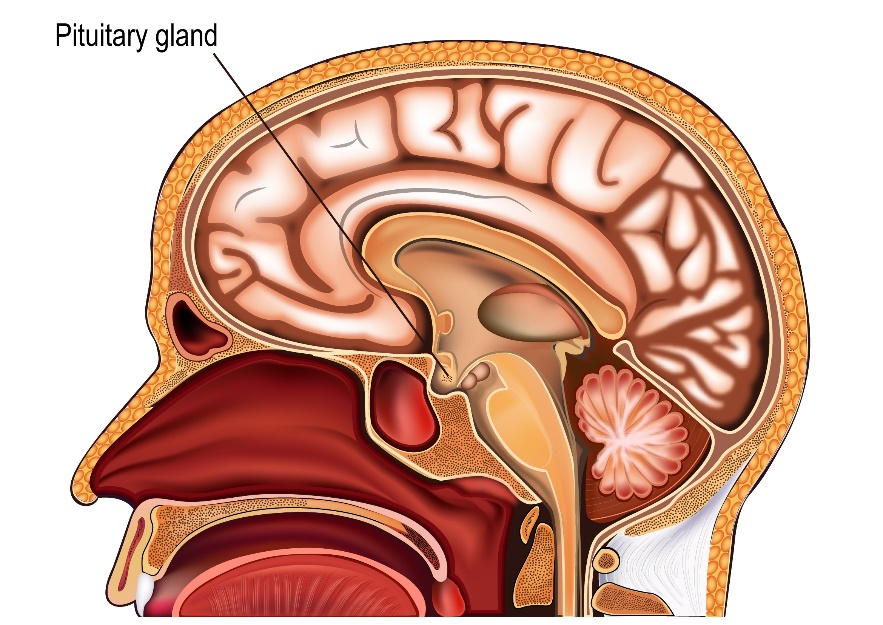
A pituitary gland is a hormone producing gland present at the lower part and middle of the brain.
The gland produces hormones which are chemicals that have effects on other hormone producing glands in the body. A tumour can develop from any of these hormone producing cells. These tumours can be secreting or non secreting. Secreting tumours are those that produce the same hormones as the cells from which they arise from. Pituitary tumours are benign.
Pineal Tumours
Pineal gland is a small gland present in the lower part of the centre of the brain. Tumours arising from it can be varied from teratomas to pineocytomas and pineoblastomas.
Spinal Tumours
Tumours can arise in the spinal canal or spinal cord. The tumours can be varied and include gliomas, meningiomas, chordomas, schwannomas and neurofibromas. Some of these tumours are benign and some are malignant.
Germ Cell Tumours
These are tumours that start in primitive cells from which the reproductive system developed.
Germ cell tumours occur normally in the abdomen and chest but can sometimes start in the brain. They are present close to the pineal or pituitary gland.
Symptoms that occur from brain tumours vary depending on the type of tumour present and its location. Symptoms can be of sudden onset or may develop gradually over weeks or months.
Common symptoms associated with brain tumour include
Headaches
Headaches can be sudden in onset or develop gradually. The headache can be dull aching or throbbing and may be associated with nausea and vomiting. These symptoms are caused by a rise in the pressure in the head. Headache can be present at night and at waking up in the morning.
Reduced Vision
One of the symptoms associated with brain tumours includes reduced or blurring of vision. This can be gradual or sudden and due to pressure on the parts of the brain that are associated with vision.
Seizures
Seizures or fits are involuntary movements of a small part of a body or all limbs at once. This can be associated with biting the tongue, passing urine without control and drowsiness after the fit. These are common in patients with brain tumours and is due to irritation in parts of the brain by the presence of the tumour.
Weakness
Weakness of one limb or one half of the body or face are symptoms seen in this setting. This can be associated with difficulty speaking or swallowing. Tumours present in the spine can cause areas of weakness below that level of spine usually leading to weakness of legs.
Raised Intracranial Pressure
There is increased pressure in the brain particularly when the drainage of fluid present in the brain is blocked by the tumour. This situation causes symptoms such as headaches which are worse in the morning or coughing and moving, nausea, vomiting, raised blood pressure, low heart rate and reduced vision.
Cerebellar Symptoms
When tumour is present in the part of the brain called the cerebellum, specific symptoms such as loss of balance and unsteadiness, difficulty with speech and tremor can be present.
Other symptoms include, memory loss, forgetfulness, change in personality, hearing loss, numbness and loss of sensation, or problems with reading or writing. When a pituitary secreting tumour is present, manifestations from the secreting hormone are present which can include weight gain, tiredness, skin changes, change in periods and increase in size of hands and feet.
It is important to note that a lot of these symptoms are present in normal people and do not always suggest a brain tumour. You would need to see a doctor if these symptoms happen more commonly than before and don’t settle down.
When a brain tumour is suspected, a brain scan is usually the first test done. Listed here are tests that are done to diagnose brain tumours. Not all tests will be needed in each situation.
CT Scan Head
CT scan is usually the first test that is done when the patient presents with symptoms. This is best done with injection of contrast into the vein at the time of the scan as better pictures are obtained with contrast. Generally, a CT scan is inferior to MRI scan in diagnosis and evaluation of brain tumours except in a few situations.
MRI Scan
An MRI scan of the brain and/or spine is done after the CT if needed. Sometimes, an MRI scan may be done before the CT scan. A contrast agent is injected into the vein at the time of the scan as this gives better images. A brain tumour is almost always visible on an MRI scan. Specialised MRI scans such as scans with DWI (diffusion weighted imaging), DTI (diffuse tensor imaging), MRA (magnetic resonance angiography), MRS (magnetic resonance spectroscopy) may be used to get more information from the images.
Biopsy
A biopsy involves taking a small sample of the tissue in question and looking at it under the microscope. To make a diagnosis of a brain tumour a brain biopsy is done after spotting it on the scan. This procedure is done by the neurosurgeon. If the biopsy shows a tumour the neurosurgeon may remove the tumour at the same time.
CSF Analysis
CSF or cerebrospinal fluid is thin water like fluid present in the central part of the brain called the ventricles. This fluid flows through the ventricles and is connected with the CSF that is present around the spinal cord in the spine. In certain types of brain tumours, analysis of the CSF is needed to exclude presence of cancer cells in that fluid.
Myelogram
This is a test that is used to image the spine in a setting when an MRI cannot be done. Here a dye is injected first into the space around the spinal cord and x-rays are taken.
Angiogram
An angiogram is a test done to look at the blood vessels. A cerebral angiogram helps look at the blood vessels in the brain in relation to the tumour. With MRI available these days, this test is not used as much.
PET-CT Scan
A PET scan is not commonly used to diagnose brain tumours. It is done after treatment to differentiate between tumour and scar tissue when there is suspicion of recurrence. It can also be used to differentiate between low grade and high grade gliomas on scan.
What is Acoustic Neuroma
Acoustic Neuroma or vestibular schwannoma is a benign tumour that starts from the schwann cells which make up the protective covering of the 8th cranial nerve present in the brain. They account for about 6-8% of brain tumours and are more common in patients with a genetic condition called Neurofibromatosis type 2.
Symptoms
The common symptoms present in acoustic neuroma include hearing loss deafness or ringing sensation in the ears(tinnitus). These symptoms are usually on one side and can be on both sides too. Other symptoms that can be present include unsteadiness on feet, numbness of face and rarely weakness of the face.
Investigations
The investigation of choice when an acoustic neuroma is suspected is an MRI scan of the brain. If an MRI is not possible, a CT scan is done. Other investigations include audiometry tests to assess hearing function.
Treatment
Treatment options of acoustic neuromas include surgery, radiotherapy or observation
Observation is an option when the tumour is small and is not causing any symptoms particularly in older patients. Treatment can be done when the tumour increases in size or starts to cause symptoms.
Surgery or Radiotherapy offer equal chances of control of the tumour. Which option to select depends on the expertise available at the cancer centre and the choice of the patient.
When surgery is done, complete removal of tumour is aimed for and possible.
When radiotherapy is used, stereotactic radiosurgery, fractionated stereotactic radiotherapy or standard radiotherapy are all options that can be used.Stereotactic radiosurgery (SRS) involves a single high dose of radiotherapy to treat the condition. This can be given with a modern linear accelerator or a gamma knife machine. Fractionated stereotactic radiotherapy (FSRT) is a technique, where the radiotherapy is given or more than 1 treatment and is used when the acoustic neuroma is larger or there are critical organs too close to the tumour to allow SRS to be done. Treatments are given over 5-10 sessions. Standard radiotherapy is over 5-6 weeks. Proton beam therapy is also an option to treat this condition. Side effects such as hearing loss are possible for both surgery and radiotherapy. Overall, the outlook is good with either of these treatments. Patients who had treatment or on observation should have regular scans such as MRI scan, for up to 10 years to look for recurrence.
Pituitary Gland
The pituitary gland is a small gland present at the lower part of the brain. The gland can be divided into an anterior part(front) and posterior part(back). The gland produces a number of hormones that have important functions in the body. Hormones are chemical substances that are produced in one place and are transported in the bloodstream to have an effect in other parts of the body.
Many hormones are produced by the pituitary including-
- Thyroid stimulating hormone
- Follicle stimulating hormone
- Leutinising hormone
- Growth hormone
- Adrenocorticotrophic hormone
- Prolactin
- Melanocyte stimulating hormone
- Oxytocin
- Antidiuretic Hormone
Pituitary Tumour
A pituitary tumour is a tumour or growth that has started in the pituitary gland. A pituitary tumour can be a secreting tumour where it produces one of these hormones or a non-secreting tumour which does not produce any of these hormones. Most pituitary tumours are benign tumours.
Symptoms
Pituitary tumours can produce symptoms due to local effect of the tumour on surrounding brain structures and cause headaches or due to abnormal effects of excess hormones produced by the tumours. These effects that the hormones produce vary greatly.
For example, excess production of growth hormone in a child can lead to excessive height and in an adult can lead to enlargement of bones, muscles and other parts, development of diabetes and increased sweating.
Hormones such as Prolactin can produce milk in the absence of pregnancy or enlargement of breasts in a male patient and sexual problems.
Increased production of Thyroid stimulating hormone, there is excess thyroxine in the blood.
Increased production of ACTH hormone can cause high blood pressure, weight gain and changes on the skin, face(becomes round), mood changes and high sugar in the blood.
Other side effects include difficulty sleeping, excessive thirst and passing large quantities of urine. Symptoms such as excess body hair in women or stopping of periods etc can be present when there is increase in production of FSH and LH hormones.
Visual symptoms
The pituitary gland is very close to the optic chiasm which is an important part of the visual pathway. A tumour there can cause compression of the optic chiasm causing reduced sight, blurring in eye sight or double vision.
Investigations for Pituitary Tumours
Common investigations done when a pituitary tumour is suspected include a CT scan or an MRI scan of the brain. If a secreting tumour is suspected, then the levels of the hormones in the blood are measured to see if there is an excess production of such hormones.
Treatment of Pituitary Tumours
The treatment of these tumours depends on the type of tumour that is present. Some hormone secreting tumours can be treated with drugs that control the production of the hormone.
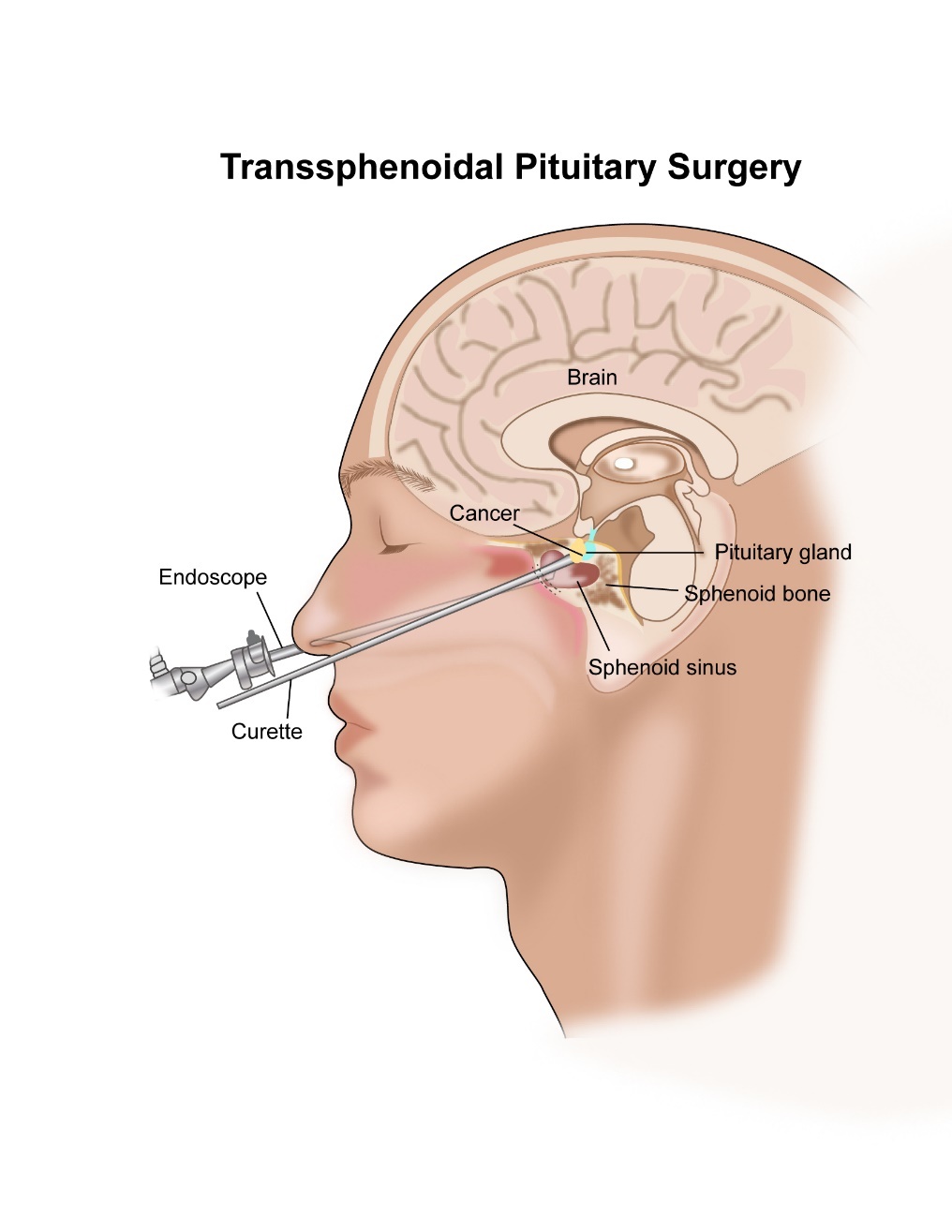
Surgery
Surgery to remove the pituitary tumour is a common option of treatment that is used and is the first treatment that is often used in the treatment of non -secreting tumours. There are two types of surgery that can be done. One is trans-frontal approach and the other and more common is trans-sphenoidal surgery. Usually endoscopic surgery is done where a tube(endoscope) is placed through the nose to get access to the pituitary gland. Surgery is also used if there is a recurrence of tumour after initial treatment. In very large tumours, a craniotomy (opening the skull) may be needed to remove the tumour.
Radiotherapy
Radiotherapy is another option of treatment of pituitary tumours. Radiotherapy is usually an option if there is incomplete removal of the tumour at surgery, presence of tumour after medical treatment. Various modes of radiotherapy can be used in this setting such as Stereotactic radiosurgery, Stereotactic radiotherapy or standard radiotherapy. A course of standard radiotherapy lasts around 5 weeks. The benefit of radiotherapy can take a while to be seen in some pituitary tumours. Type of Radiotherapy that can be used includes Gamma Knife, Linear accelerator based or using Proton therapy.
Medical Management
Some pituitary tumours can be managed with the help of medicines in the form of tablets or injections.
For patients with a tumour called a Prolactinoma, which produces Prolactin, medications such as Bromocriptine or Cabergoline can be used. This drug helps control the symptoms produced by this tumour.
For patients with Acromegaly here there is excess production of growth hormone, medications such as somatostatin analogues can be used in addition to Surgery or Radiotherapy.
For tumours that produce ACTH, medication such as Cabergoline is used to control the effects of the tumour.
Side Effects of treatment of Pituitary tumour
One important side effect of surgery or radiotherapy of pituitary tumours is hypopituitarism. This means that there can be less production of the hormones that the normal pituitary gland would produce after these treatments. Therefore, it is important to be seen by the doctor regularly after treatment to check on the levels of these hormones.
Other potential side effects include headaches, increased thirst and urination particularly after surgery(usually settles), csf leak, tiredness, hair loss, nausea and changes in eye sight.
What is a Meningioma
Meninges are outer coverings of the brain. There are three layers of meninges and are called Dura, Pia and Arachnoid. The dura is the outermost cover and the arachnoid the inner most.
Meningiomas develop from the meninges and form about 25% of primary brain tumours. Meningiomas are more common in the elderly population and more common in females than males. Meningiomas are usually benign tumours which means that they do not have the capacity to spread to other parts of the body. Some meningiomas can be malignant.
Grading of Meningioma
Meningioma is given a grade after a sample of it is examined under the microscope. The grading is from 1-3 with grade 1 meningioma being benign and least aggressive and grade 3 being more aggressive in its behaviour. Treatment options differ slightly depending on the grade identified.
Symptoms of Meningiomas
Meningiomas can grow without causing any symptoms in its early stages. Some meningiomas can grow over a number of years. When they produce symptoms, these are similar to symptoms from any other brain tumour. See the section on symptoms of brain tumours for more information.
Treatment of Meningiomas
Observation
This is an option where treatment is not given, and the patient is monitored over a period of time. This can be done over many years. Treatment is proposed when there is increase in size on serial scans or the patient become symptomatic. This option of management in offered in patients with small tumours not producing any symptoms.
Surgical Removal
In patients with either large or symptomatic tumours, surgical removal of the meningioma is the treatment of choice. This is done with a craniotomy and majority of the times the entire tumour is removed. Surgery is done under general anaesthesia.
Radiotherapy
Radiotherapy is a treatment option in patients with a meningioma that is only partially removed or in patients with grade 2 and 3 meningiomas after complete removal. Radiotherapy is also given to patients who have had a recurrent meningioma removed. In these patients, radiotherapy is given soon after surgery. Radiotherapy can be used as a treatment instead of surgery in patients who are not considered fit to undergo surgery or those where surgery is not possible for other reasons. For more details of Radiotherapy in meningiomas, see section on Radiotherapy for brain tumours.
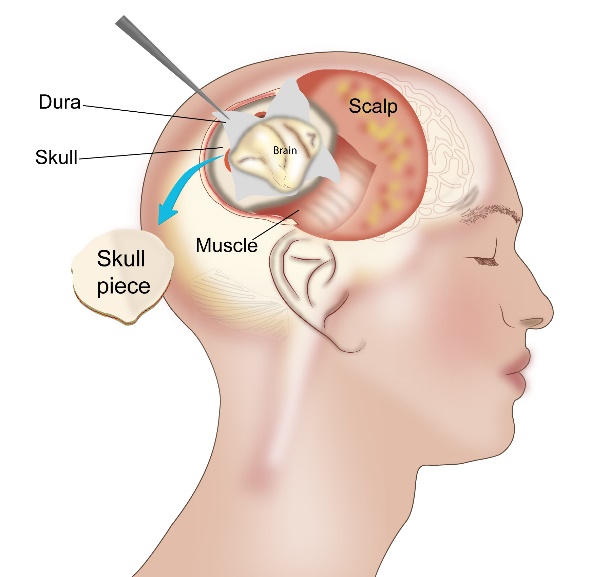
Surgery
surgery forms an important part in the treatment of brain tumours. Brain tumour surgery is done by Neurosurgeons. The type of surgery done is dependent on the type of tumour, its location in the brain and the general condition of the patient. Surgery can be in the form of a complete resection, where all the tumour is removed. It can be in the form of partial resection where only a part of the tumour can be removed. It can also be only in the form of a biopsy where a small sample of the tumour is removed. These surgeries are done under a general anaesthetic.
The surgery can be done in the following ways.
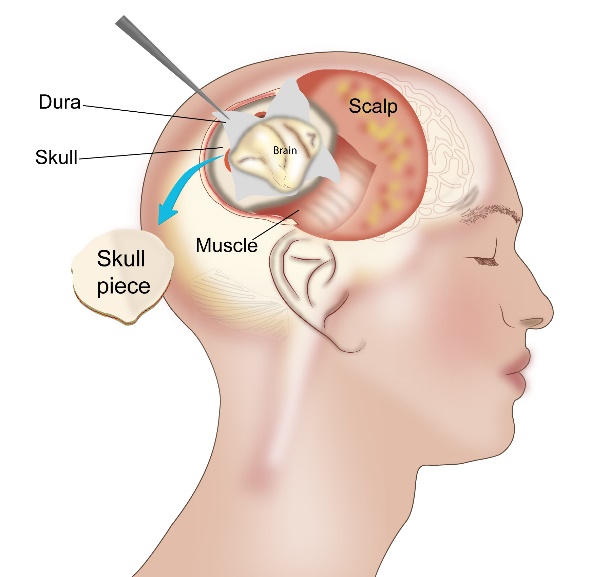
Craniotomy
Craniotomy is a procedure where a piece of the skull is removed to gain access to the tumour. At the operation as much of the tumour is removed as possible without damaging the normal part of the brain. A microscope is sometimes used to get a better view of the area of operation. In some situations, an awake craniotomy is done, where the patient is awake during the surgery and this procedure is employed when the surgeon operates on a part of the brain that controls important functions such as speech movement or sensation. Brain mapping with the help of cortical stimulation helps in identifying areas related to functions on the body. This allows the neurosurgeon to avoid operating on parts of the brain that are associated with critical functions if possible. Other mapping techniques such as speech mapping are used with awake craniotomy as described above. CT or MRI guided surgery can be done with the help of serial scans to assess the progress of the surgery. Following removal of the tumour, the skull bone is fixed back in place.
In the certain type of tumours, there is a blockage of the flow of fluid that is present within the brain. At the time of operation, the surgeon may put in a shunt which is a tube and that helps drain this fluid. The most common shunt that is put in is called a ventriculo-peritoneal (VP) shunt which connects the ventricles of the brain to the abdomen. An ommaya reservoir is a tube that is permanently placed in the brain and is in contact with the skin to allow removal of fluid as and when needed in some patients.
Microsurgery
In certain brain tumours, microsurgery is done where a small keyhole is made in the skull and a thin tube is placed through the hole. This tube is called a neuro endoscope and gives pretty good and magnified views of the inside of the brain. This allows the surgeon to do the operation with precision and with a small incision. The neurosurgeon will be able to cut and remove the tumour with the help of instruments that are present at the end of the microscope.
Biopsy
As discussed above a biopsy may be the only surgical operation that is suitable in some situations. Biopsy can be open biopsy where a small hole is made with removal of a small piece of the bone, and tumour sample taken through that. At other times, a stereotactic biopsy is done which involves use of a CT or MRI guidance at the time of biopsy. Another method called neural navigation is also used which uses a complete device and system to help guide the surgeon to put in a needle for the biopsy.
Pituitary Surgery
Surgery for removal of a pituitary gland tumour is done in a different method as compared to treatment of other brain tumours. The common approach is through the nose where access is gained into the area under the brain where the pituitary gland is located.
Radiotherapy is the use of high energy x-rays given to kill cancer cells. These x-rays cause damage to the DNA of the cancer cells and thereby kill them. Radiotherapy is a local treatment and has its effect in the area that it is given to. It is given using a large machine (Linear Accelerator) which generates the x-rays and delivers the treatment to the patient. Proton therapy is also a form of radiotherapy. These methods are called as external beam therapy.
Radiotherapy forms an important component of treatment for Brain tumours. The type and duration of radiotherapy depends on the type of brain tumour, its location and the fitness of the patient to tolerate the treatment.
The Radiotherapy Process
Having radiotherapy to the brain is a step wise process.
Making the mask
The first part of the treatment process involves making a mask and having scans with the mask in place. The mask is usually made of plastic which can be moulded into shape when heated.
The patient is asked to lie down in the same position as he/she would when having treatment. The treatment radiographers will take a sheet of thermoplastic shell and soak it in warm water. After some time, when the sheet is warm, it is wrapped around the face slowly, moulding the sheet into the shape of the face. The purpose of the mask is to hold the head in the same position during the entire treatment, making treatment delivery very accurate. Therefore, it is important that the mask fits the face very tightly. Once accurately positioned, the mask is removed and allowed to cool. Once cooled, the mask will retain the shape of the face. The mask is worn every day during treatment.
Planning CT scan
A radiotherapy planning CT scan is done after the mask is made. This scan allows the doctor to see the disease and to plan the radiotherapy accordingly. Normally, the patient would have had a CT or MRI before, but a planning scan is still needed as it needs to be done with the patient in the treatment position. An MRI planning scan can also be done in this setting in some patients.
Radiotherapy Planning
Once the scan is done, the doctors and physicists need a few days to plan the treatment only after which will treatment start.
Types of Radiotherapy
As stated above, radiotherapy is use of high energy x-rays. The different types of radiotherapy listed below are different in the manner this treatment is delivered. Radiotherapy can also be given with the use of Protons.
Standard fractionated radiotherapy
Radiotherapy treatment is given over a number of days, usually once a day. Each day’s treatment is called a fraction, as a fraction of the total dose of radiotherapy is given that day. Standard radiotherapy is given daily, 5 days a week for 3-6 weeks depending on the type of brain tumour. This type of treatment is given as 3D conformal radiotherapy, intensity modulated radiotherapy (IMRT) or Arc therapy (Rapid Arc, VMAT), Cyberknife or Proton therapy. This type of radiotherapy is by far the commonest method used.
Stereotactic Radiosurgery (SRS)
Stereotactic radiosurgery is a form of radiotherapy treatment, where all the treatment is given in one fraction in a single sitting. The treatment involves giving a high dose of radiotherapy to a small area with high accuracy. This type of treatment is used to treat some brain tumours such as meningiomas, acoustic neuromas or schwannomas, pituitary adenomas, brain metastases and some others. As all the treatment is given in one fraction only, more accuracy is needed when using this treatment. Therefore, specialist radiotherapy equipment and techniques are used. The total duration of the treatment can range from 20-45 minutes when treated with a linear accelerator (Novalis,Truebeam,Edge systems) or longer 40-120 minutes when treated with a Gamma knife or Cyber knife system.
A Gamma knife is one such specialised radiotherapy machine that is used to deliver stereotactic radiotherapy to the brain. When a Gamma knife is used, a special stereotactic frame is needed to keep the head very still.
Newer radiotherapy machines listed above are able to deliver stereotactic radiotherapy without the need for a stereotactic frame. A mask is used as in standard radiotherapy. This is also known as frameless radiosurgery.
Fractionated stereotactic radiotherapy (SRT)
Here, the radiotherapy techniques, precision and indications are similar to stereotactic radiosurgery. The main difference is that instead of giving the dose in one fraction of treatment, the dose is split up into a few fractions. The decision to use radiosurgery or fractionated stereotactic radiotherapy is based on the type, size, number and location of the tumour as well as potential side effects from treatment.
Side Effects of Brain Radiotherapy
Radiotherapy to the brain is associated with some side effects which are listed below.
Hair loss
This is common with brain radiotherapy and there is loss of hair on the head. The hair loss can be patchy, confined to the areas from where the radiotherapy went into the brain. Hair loss can be temporary or permanent depending on the dose of radiotherapy given.
Skin Changes
The skin on the head can become red and painful. This settles a few weeks after the treatment is completed.
Headaches and Tiredness
These are common side effects of radiotherapy and settle down a few weeks after the end of treatment.
Nausea and Vomiting
These effects can happen in some patients having brain radiotherapy. Taking tablets 30 minutes prior to the treatment can help with the symptoms.
Raised Intracranial Pressure
In patients having radiotherapy to the brain, the pressure in the brain can increase and if the patient is on steroids, the dose of that may have to be increased to treat this side effect.
Increased Sleepiness
This is a potential side effect and happens a few weeks after completion of treatment.
Reduced Concentration and Memory
This is a known side effect of brain radiotherapy and is dependent on the dose of treatment and the area of brain treated.
Reduced Pituitary function
This is a side effect that can happen months to years after radiotherapy to the brain. The function of the pituitary gland has to be monitored in patients who have had radiotherapy to that part of the brain.
Low grade gliomas include pilocytic astrocytomas, oligodendrogliomas, diffuse astrocytomas and gangliogliomas. Treatment options for low grade gliomas include Surgery, Radiotherapy, Chemotherapy and Observation. These options are discussed in detail below.
Surgery for low grade glioma
Surgical removal of glioma forms an important component of its treatment. The outcome is best when a complete resection is done, where all the tumour is removed. In some instances, depending on the location of the tumour, a debulking procedure is done. Here removing all the tumour is not possible and only some part of the tumour is removed. In other situations, a debulking is also not possible, and a biopsy alone is done. Overall, studies have shown that the outcome is better if more surgery is done and this should be balanced against the side effects and functional disabilities that may arise as a result of the surgery. In a small group of patients with small tumours and no symptoms, delaying surgery to a later time may be possible.
Radiotherapy
Radiotherapy or radiation therapy involves use of high energy x-rays for treatment of cancers. In low grade gliomas, radiotherapy is given following surgery to improve outcome and to delay the progression of the tumour. Radiotherapy given in this setting, is done daily, 5 days a week for up to 6 weeks. This treatment can be done soon after surgery(early) or in some patients can be deferred to a time when there is definite increase in cancer again after surgery(delayed). The exact timing of this treatment will be decided based upon the tumour and the symptoms and wishes of the patient. Early radiotherapy has been shown to reduce symptoms in patients but has not been shown to improve survival when compared to delayed treatment.
Common side effects of brain radiotherapy include tiredness, hair loss, nausea, loss of appetite, headaches and aggravation of initial symptoms such as limb weakness or fits. Some long term effects of radiotherapy can include reduced concentration and memory.
Chemotherapy
Chemotherapy involves use of drugs in the form of tablets and injections to treat cancers. Chemotherapy forms an important component of treatment for low grade gliomas.
Here chemotherapy is usually given after completion of radiotherapy. Chemotherapy given after radiotherapy has been shown to be beneficial than compared to radiotherapy alone. The drugs used here are Procarbazine, lomustine and vincristine (PCV) or Temozolomide. In patients with oligodendrogliomas, chemotherapy alone after surgery instead of radiotherapy may be an option. Special genetic tests can be done on the tumour sample that has been removed looking for genetic changes that can predict response to chemotherapy and also survival. This test looks for chromosome 1p 19q codeletion, and if present can give more benefit from chemotherapy.
Chemotherapy is also used again when there is recurrence of cancer after initial treatment with surgery radiotherapy and chemotherapy. Chemotherapy given in this setting is called as second line therapy. Here the options of treatment include drugs such as PCV or Temozolomide among others.
Gliomas are high grade if they are graded as grade 3 or grade 4 at biopsy. High grade gliomas include Anaplastic oligodendroglioma, Anaplastic astrocytoma and Glioblastoma. The management of high grade gliomas is different to that of low grade gliomas. Below are the treatment options for high grade glioma.
Surgery
In most patients, the first treatment option after a diagnosis of high grade glioma is surgical removal of the tumour. For more details about surgery in brain tumours, see section on surgery in brain tumours.
Radiotherapy
Radiotherapy or radiation therapy involves use of high energy x-rays for treatment of cancers. Radiotherapy is an option of treatment in high grade glioma. It is given after surgery is done to remove the tumour. In high grade glioma, it is important to start radiotherapy soon after surgery to prevent the tumour from growing back again. The treatment is given over a period of 6 weeks and is given along with a chemotherapy drug called Temozolomide. This drug is given during and after completion of radiotherapy. In patients who are not fit enough or in the elderly, the radiotherapy is given for a shorter duration and is given with or without chemotherapy.
Common side effects of brain radiotherapy include tiredness, hair loss, nausea, loss of appetite, headaches and aggravation of initial symptoms such as limb weakness or fits. Some long term effects of radiotherapy can include reduced concentration and memory headaches and difficulty managing regular tasks.
Chemotherapy
Chemotherapy is used to treat high grade gliomas. Chemotherapy is use of drugs given in the form of tablets, injections or drips to help reduce and control cancer. In high grade gliomas, chemotherapy with Temozolomide is used along with radiotherapy. This drug is taken as tablets daily during radiotherapy and for up to 6-12 months after completion of radiotherapy. When given after radiotherapy, it is given for 5 days every month.
Treatment given this way helps achieve maximum control of the tumour. The decision to use radiotherapy alone or combination of radiotherapy and chemotherapy will be made by the Oncologist after assessing the fitness of the patient. In elderly patients or those not fit, Radiotherapy or Temozolomide is used on its own after surgery.
Chemotherapy is also used after recurrence of disease following initial treatment. Here the drugs used include Procarbazine, lomustine, vincristine (PCV), Carboplatin, Irinotecan and Bevacizumab.
Bevacizumab is a monoclonal antibody and stops the development of new blood vessels. It is used in the treatment of high-grade gliomas such as Glioblastoma either on its own or in combination with chemotherapy such as Irinotecan and Lomustine. Side effects of Bevacizumab include high blood pressure, risk of bleeding and delayed healing of wounds.
Others
A very small group of patients with high grade gliomas have genetic changes in the tumour such as fusions in NTRK genes. These patients may benefit from newer biological agents such as Larotrectinib and Entrectinib.
Supportive Care for patients with Brain tumours
Patients with brain tumours can have many needs, disabilities and issues hat are different to patients with other cancers. Adequate and planned supportive care is needed to make sure patients have optimum function after completion of their treatment.
Use of Steroids
Steroids are drugs that are commonly used in patients with brain tumours or cancers. The commonest steroid used is Dexamethasone. Steroids help reduce accumulation of fluid around the tumour in the brain, thereby reducing the pressure in the head and improving symptoms. The dose of dexamethasone used is dependent on the condition of the patient. This dose is titrated up and down by the doctor. It is important for the patient to follow the guidance strictly. Steroids should not be stopped suddenly, particularly if they have been taken for more than 2 weeks. The dose of the steroids should be gradually cut down and the doctor will advise regarding this. Side effects of long-term steroid use include weight gain, swelling of face, easy bruising of skin, risk of infection, increase of sugar levels in diabetic patients, increased appetite and weakness in muscles causing difficulty climbing stairs. Despite these side effects, steroids play a vital role in managing patients with brain tumours.
Anti-seizure medications
Many patients with brain tumours are prescribed medications called antiepileptics to reduce the risk of seizures. These could be for patients who had seizures and also those who did not have any seizures. It is important for patients to take these medications, to reduce their risk of getting fits. The doses of these medications need to be changed or alternative medicines used if fits continue to happen despite these medications.
Physiotherapy, occupational therapy and others
Patients with brain tumours can be disabled with reduced mobility, speech, or ability to perform daily activities. During and following completion of treatment, appropriate physiotherapy to help improve mobility of the patient is needed, occupational therapy to help with maintain independence of the patient, speech and language therapy, swallowing assessment etc may also be needed depending on the patient’s symptoms.
Primary CNS Lymphoma is a type of Non Hodgkins Lymphoma that starts in the brain or other structures such as eyes, spinal cord or meninges of the brain. Its features, behaviour and treatment are different to that of lymphomas that begin in other parts of the body.
Symptoms of Primary CNS Lymphoma
This type of lymphoma produces symptoms related to the brain. Common symptoms include headaches, fits, confusion, reduced memory, change in personality, reduced eye sight, vomiting and weakness of different parts of the body.
Investigations for Primary CNS Lymphoma
When this type of cancer is suspected or the patient presents with above symptoms, the following tests are done.
MRI Scan
An MRI scan of the brain is commonly done to look for abnormalities in the brain when a patient presents with above symptoms. A CNS lymphoma is one of the possible causes for these symptoms and is seen on the MRI scan.
CT Scan
In places where an MRI scan is unavailable, a CT scan is used to look for abnormalities in the brain.
CSF Analysis
CSF or cerebrospinal fluid is the fluid that is present in the ventricles of the brain and in the spinal cord. A sample of this fluid is taken and tested for presence of Lymphoma cells as part of investigations.
Biopsy
A biopsy of the abnormal area in the brain is done to confirm the diagnosis of CNS lymphoma.
Treatment of Primary CNS Lymphoma
The treatment of this condition mainly depends on the age and fitness of the patient. Surgery is not an option of treatment generally for this condition.
Chemotherapy
For patients who are young and fit, combination chemotherapy is the treatment of choice for this condition. This chemotherapy includes drugs such as Methotrexate, Cytarabine and Rituximab. This treatment can cause side effects and hence only given in this group of patients. For patients who have a complete response to treatment, no further treatment may be needed. On the other hand, some doctors advise treatment such as stem cell transplant or radiotherapy or consolidation chemotherapy. A course of chemotherapy may also be given into the spinal canal and is called as intrathecal chemotherapy.
For patients that are not fit or are aged more than 50 years, less intensive chemotherapy such as Temozolomide and Rituximab are used to treat the disease.
Radiotherapy
Radiotherapy is an option of treatment for patients with this condition. Radiotherapy is not a curative treatment on its own. Radiotherapy is usually an option of treatment in patients who do not have a complete response to chemotherapy or are not fit enough to have chemotherapy or have recurrence of the cancer after chemotherapy. The course of radiotherapy ranges from 3-5 weeks depending on the situation that it is being used in. For more details on radiotherapy, see the section on radiotherapy in brain tumours.
The follow up process involves patients being seen in the out-patient clinic on a regular basis after completion of treatment. This is important as any increase of disease can be picked up early and acted upon. Also, the doctor will be able to monitor any side effects that have occurred as a result of the treatment. The follow up schedule will be different for different brain tumours. The process involves visiting the doctor every 3 months initially and gradually the interval between visits increases. An MRI or CT scan is done about 2-3 months after end of radiotherapy and this scan is used as a baseline for comparison with future scans. Regular scans every 3-6 months are done initially and every year later to monitor the tumour. Blood tests to monitor the function of the pituitary gland are also done regularly.




