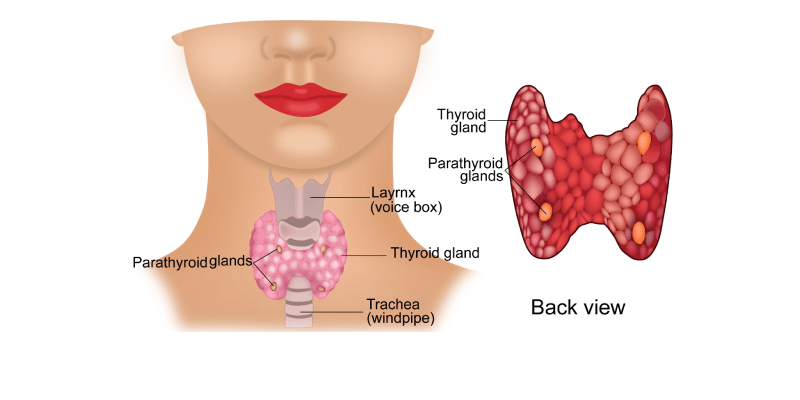
Thyroid gland is an endocrine gland present in the neck. An endocrine gland is a gland that produces and secretes hormones directly into the blood stream. The body has many endocrine glands and thyroid is one of them.
The thyroid gland is present in front of the neck below the Adam’s apple. It is made up of two lobes, right and left on either side joined together by an isthumus.
The thyroid gland produces a hormone called thyroxine. This helps in general growth and development of the body.
Thyroid cancer is cancer that starts in the thyroid gland. According to Globocan data 2018, there were 18688 cancers of thyroid in India making up 1.6% of all cancers.
Thyroid cancer can be of many types. These are listed below.
This is by far the commonest form of thyroid cancer making up about 60% of all thyroid cancers. This cancer is more common in women, usually diagnosed at a younger age and is slow growing.
This is the second commonest form of thyroid cancer making up about 15% of them. This type of cancer is also common in young and middle-aged people. Follicular and papillary cancer together, are known as well differentiated cancers. Majority of these differentiated cancers are curable.
This type of thyroid cancer makes up about 5-10% of all thyroid cancer. About a quarter of these are caused by a faulty gene inherited in the family. The condition is called MEN 2 syndrome and all patients diagnosed with medullary cancer of the thyroid should be tested for this syndrome.
This is an uncommon type of thyroid cancer. It usually presents in the elderly and can progress quite rapidly.
This is a rare form of thyroid cancer. Non-Hodgkin’s lymphoma is a cancer originating in the lymph nodes and lymphatic system. It can originate in any part of the body and occasionally starts in the thyroid.
The following are potential risk factors for the development of thyroid cancer.
Benign Thyroid conditions
People who have benign (non-cancerous) thyroid conditions are at a higher risk to develop a thyroid cancer. These benign conditions could be thyroiditis (inflammation of thyroid), goitre (swelling of the thyroid) or a benign nodule. Having a family history of benign thyroid disease can also increase the risk of developing thyroid cancer.
Exposure to Radiation
Previous exposure of the neck to radiation increases the risk of developing thyroid cancer. This radiation exposure could have been due to treatment of a cancer in the neck region with radiotherapy in childhood. Exposure to radiation from nuclear accidents increases the risk too.
Genetic Cause
Having an inherited faulty RET gene can lead to syndromes such as MEN 2 syndrome. In this syndrome, there is a risk of development of thyroid and other cancers types of cancers too.
Diet low in Iodine
A diet low in Iodine can lead to an increased risk of thyroid cancer. Use of iodised salt in India has reduced the incidence of Iodine deficiency. A diet rich in butter meat and other fats increases the chance of thyroid cancer.
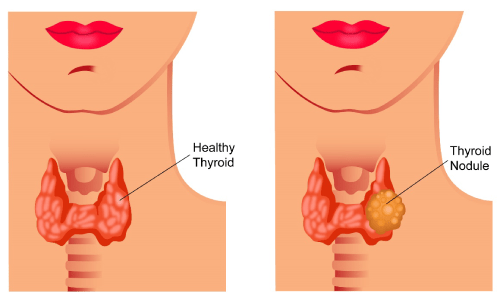
The commonest symptom of a thyroid cancer is the presence of a painless lump in the neck. This lump increases in size slowly. An anaplastic carcinoma presents with a rapidly growing neck lump.
Sometimes, a thyroid cancer can compress the wind pipe or gullet and cause breathlessness or difficulty with swallowing. Other symptoms associated include change in voice or cough. Rarely, the first symptoms of a thyroid cancer can come from cancer that has spread to other parts of the body such as coughing up of blood or pain.. Thyroid cancer may not cause any symptoms at all and may be an unexpected finding after an operation for a benign lump in the thyroid gland.
It is important to know that most lumps arising from the thyroid are benign lumps and not cancers. It is advised strongly however to see the doctor if a lump is felt in the neck.
The following investigations are done for a suspected Thyroid cancer.
Blood Tests
Blood tests are usually done as part of investigations to check for thyroid function (TFT). The other blood tests that can be done include calcitonin levels, calcium and phosphate levels.
Ultrasound Scan of Neck
An ultrasound scan of the thyroid uses sound waves to get a picture of the gland. This test is very good in telling if there is a lump and whether the lump contains liquid, like in a cyst, or is solid, containing cells. The scan is done by putting some gel on the neck and using a handheld probe over it. The test takes a few minutes and is painless.
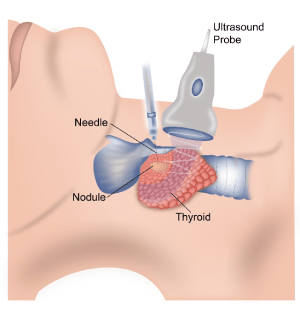
Thyroid FNAC
CT (computerised tomography) scan
A CT scan is a test that uses x-rays to get detailed images of the body. When thyroid cancer is suspected or investigated, a CT scan of the neck and chest is done to identify the cancer and look for spread. This scan takes a few minutes to do and is painless.
MRI (Magnetic resonance Imaging) scan
An MRI scan uses magnetism to get good images of the body. In thyroid cancer, it is used to image the neck. It doesn’t involve any x-rays. Patients who have some types of metal implants or a cardiac pacemaker will not be suitable to have this type of scan. An MRI of the neck can give very detailed images of the neck and is considered better than that of a CT scan.
Thyroid Isotope scan
A thyroid radioisotope scan uses a small amount of radioactive Iodine to help locate thyroid tissue around the neck and body. The scan takes under an hour to do. First, the radioactive Iodine is injected into a vein. This Iodine is taken up preferentially by the thyroid tissue compared to the rest of the body. After a brief wait, a scan is done with the help of a gamma camera which picks up the injected substance.
PET (Positron Emission Tomography) scan or PET-CT Scan
A PET-CT scan is a specialized CT scan where a radioactive tracer called 18FdG is injected into the body prior to the CT scan. This tracer lodges in areas within the body where there is high requirement for glucose. As cancers need a lot of glucose to survive, they take up the tracer much more than the rest of the body. The cancer can then be easily spotted on the scan. This scan is occasionally done in thyroid cancer.
The stage of a cancer is a word used to describe the size and location of the cancer in the body. Knowing the stage of the cancer helps the doctors to decide on the most appropriate treatment.
Thyroid cancer is staged using the TNM system or the number system.
TNM stands for tumour, node and metastases
T Staging
| T1a | The tumour is 1cm or smaller and has not grown out of the thyroid |
| T1B | The tumour is larger than 1cm and smaller than 2cm and has not grown out of the thyroid |
| T2 | The tumour is more than 2cm and less than 4cm and has not grown out of the thyroid |
| T3 | The tumour is larger than 4cm or has just begun to grow out of the thyroid. |
| T4a | The tumour is any size and has grown out of the thyroid into nearby structures of the neck like voice box, windpipe, gullet or nerve to the voice box |
| T4B | The tumour is of any size and has grown into the nearby spine or large blood vessels |
T Staging for Anaplastic Thyroid Cancer
All anaplastic thyroid cancers are considered as T4 cancers at the time of diagnosis
| T4a | The tumour is within the thyroid |
| T4b | The tumour has grown outside the thyroid |
N Staging for Thyroid Cancer
| Nx | The regional lymph nodes cannot be assessed |
| N0 | The cancer has not spread to nearby lymph nodes |
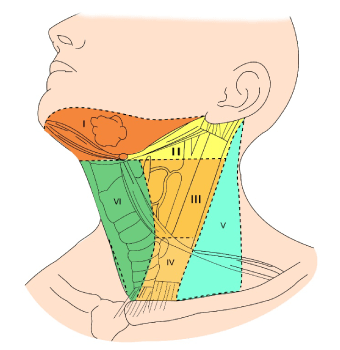
| N1a | The cancer has spread to lymph nodes around the thyroid |
| N1b | The cancer has spread to other lymph nodes in the neck or upper chest |
M Staging
| M0 | There is no evidence of distant spread of cancer |
| M1 | The cancer has spread to other parts of the body such as distant lymph nodes, organs or bones |
Number Staging
The number staging is from 1 to 4. These stages are made up by combining different TNM stages.
Stage 1- Any T stage, Any N stage, M0
Stage 2- Any T stage, Any N stage, M1
Papillary or Follicular Thyroid cancer in patients older than 45 years of age
Stage 1- T1 N0 M0
Stage 2- T2 N0 M0
Stage 3- T3 N0 M0
T1 to T3 N1a M0
Stage 4a- T4a, Any N stage, M0
T1 to T3, N1b, M0
Stage 4b- T4b, Any N, M0
Any T, Any N, M1
Medullary Thyroid Cancer
Stage 1- T1 N0 M0
Stage2- T2 N0 M0
T3 N0 M0
Stage 3- T1 to T3,N1a,M0
Stage 4a- T4a, any N, M0
T1 to T3, N1b, M0
Stage 4b- T4b, Any N, M0
Any T, Any N, M1
Anaplastic Thyroid Cancer
All anaplastic thyroid cancers are considered stage 4
Stage 4a- T4a, Any N, M0
Stage 4b- T4B, Any N, M0
Stage 4c- Any T, Any N, M0
There are different types of treatments available for thyroid cancer. These include
- Thyroid Surgery
- Radioactive Iodine Treatment
- Chemotherapy
- Radiotherapy
- Thyroid hormone replacement
Please see relevant sections for more details.
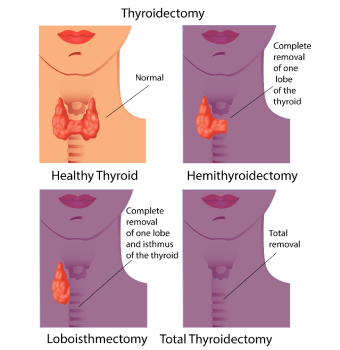
Surgical removal of the thyroid gland is usually the first treatment procedure in the management of papillary, follicular and medullary carcinomas of the thyroid. The type of surgical operation done will depend on the extent of thyroid cancer present in the thyroid gland and outside the gland. Thyroid surgery is done under general anaesthesia and usually involves inpatient stay in the hospital for one or two days.
Partial Thyroidectomy
This is surgery where one part or one lobe of the thyroid gland is removed. This is called partial thyroidectomy or lobectomy or hemithyroidectomy. It is done in some patients with stage 1 papillary or follicular thyroid cancer.
Total Thyroidectomy
Lymph node removal
Complications or side effects of Thyroid surgery
Thyroid surgery is a relatively safe operation and is practiced commonly. However, as with any type of surgery, there can be complications, and these are listed here.
Risk of Damage to parathyroid glands
During surgery, there is a risk of damage to parathyroid glands leading to development of low calcium levels in the blood and the need for calcium supplementation. This risk should be observed for after the operation.
Bleeding
Following surgery, there is a risk of bleeding from the operated site and the need to be taken back to theatre to stop the bleeding.
Damage to Nerve
There is a risk of damage to the nerve that supplies the voice box during surgery. This can lead to a hoarse voice. The hoarse voice usually gets better on its own. The risk of these side effects happening is small and the operating surgeon will explain about it in more detail.
Other Surgeries
For patients with extensive disease in the neck where complete removal of all disease is not possible, debulking surgery is sometimes done to reduce the bulk of disease after which other treatments can be tried.
A tracheostomy is a surgery where there is compression of the windpipe by the thyroid cancer making it difficult for the patient to breathe. In this surgery, a small hole is made in the trachea at the lower part of the neck below the thyroid swelling which will then enable the patient to breathe easily. A tracheostomy tube is placed in the hole.
Radioactive Iodine is a common form of treatment used for papillary and follicular thyroid cancer.
The thyroid gland normally needs Iodine for its function. The Iodine in the blood stream is taken up by the thyroid gland and used to make the thyroid hormone. The Iodine given in radioactive form is taken up by thyroid cells and differentiated thyroid cancer cells. The radioactive Iodine that is taken up emits radiation locally and kills cancer cells but doesn’t affect other parts of the body. The commonly used radioactive Iodine is I-131.
Radioactive Iodine is given after a patient has a complete thyroidectomy (removal of thyroid). It is used to destroy microscopic residual disease that could be left behind after thyroid surgery. It also helps to treat any obvious residual or metastatic disease that is present in some patients. Patients in whom radioactive Iodine is used as treatment include those with papillary cancers more than 1cm in size, follicular cancers more than 1cm in size or involving capsule of thyroid or lymph nodes.
Before Treatment
Radioactive Iodine I131 is mainly given in the form of a capsule. It can also be given in other forms too. The treatment is usually given as an inpatient. Prior to treatment with radioactive Iodine, the patient either has to stop taking thyroid hormone for a few weeks or instead take a type of thyroid stimulating hormone called r-TSH. Either of these methods help to increase TSH (thyroid stimulating hormone) levels in the blood, making the radioactive treatment work better.
Also, the patient will be asked to follow a low Iodine diet for two weeks before the treatment. Foods to avoid include fish and sea food, iodised salt, dairy products and food colourants like E127.
In Hospital
Once in hospital, the patient will be in a single room and will be isolated. The room is a specialised room with thick walls and lead lined doors that will not allow any radiation to go outside the room. This is because the patient will be radioactive for a few days and being isolated in a single room will help prevent other people being exposed to radiation. Once the radiation levels in the body reach safe levels, the patient can be discharged home.
Side Effects
The side effects of radioactive Iodine are few and mild. Occasionally the patient may notice nausea, pain or feeling of tightness in the neck or breathlessness. In the long term, some patients may have a dry mouth. In young males, fertility can be affected and sperm storage prior to treatment could be considered.
After Treatment
A few days to weeks after treatment, an Iodine uptake scan is done to look for any residual disease. If such disease is still present, a repeat dose of radioactive iodine can be given. Otherwise, the patient is followed up closely for up to 10 years.
Radiotherapy is used in thyroid cancer but less commonly than radioactive Iodine. Here we will be talking manly about differentiated thyroid cancer such as Papillary and Follicular cancers. The type of radiotherapy used here is external beam radiotherapy which is given with the help of a machine called a linear accelerator. The treatment given is usually done once a day, 5 days a week for about 5-6 weeks.
Commonly radiotherapy is used in cancer that is advanced locally where there is some residual disease after surgery or there is disease involving multiple lymph nodes or when disease has come back after initial treatment and the disease is not responding or will not respond to radioactive Iodine. Radiotherapy is also used when it is not possible to remove the disease with surgery. The area treated with radiotherapy usually includes the whole neck and areas including the upper chest.
In patients with metastatic disease, radiotherapy is used to control symptoms such as pain or bleeding when the disease has spread to the bones or lung etc. Here the treatment is given for 1-10 days with the aim being to control those symptoms.
Systemic therapy involves uses of substances such as chemotherapy and targeted therapies in the treatment of cancer. In differentiated thyroid cancer, the use of systemic therapy is not common. It is only recommended in metastatic thyroid cancer where the cancer has spread to different parts of the body and radioactive Iodine therapy has been ineffective.
In patients with metastatic thyroid cancer, genetic testing on the biopsy sample is done to look for mutations. These tests help in the decision making process of identifying a type of treatment.
Cancers that have BRAF mutations are treated with an anti-angiogenic tyrosine kinase inhibitors such as Lenvatinib are used. Others include Sorafenib, Dabrafenib and Vemurafenib.
Chemotherapy options are rarely used and the drug used in such a circumstance includes Doxorubicin.
Medullary carcinoma of the thyroid is a neuro endocrine cancer and arises from the parafollicular cells of the thyroid gland. Its behaviour and treatment is different to that of a differentiated thyroid cancer. About 20% of all medullary carcinomas arise as part of the MEN2 syndrome.
Symptoms
This cancer usually presents as single or multiple lumps in the neck. Sometimes, it can present with symptoms coming from other parts of the body due to the cancer having spread there.
Diagnosis
The diagnosis of medullary carcinoma of the thyroid is made on fine needle aspiration cytology (FNAC) of the neck lump. This is where a small thin needle is inserted into the lump and cells are aspirated. These are seen under the microscope by a pathologist.
CT Scan or MRI is done to determine the stage of cancer and look for evidence of spread of cancer to other parts of the body. Blood tests such as Calcitonin, CEA, Calcium and catecholamines are usually done prior to surgery.
Treatment
Surgery
Treatment of medullary carcinoma of the thyroid consists of total thyroidectomy (removal of thyroid). Following surgery, thyroid replacement hormone is started immediately. It is usually recommended to continue to monitor calcitonin and CEA levels in the blood.
Radiotherapy
Radiotherapy is used in some settings when a complete resection of the tumour was not possible in the neck or upper chest. The treatment is given in the form of external beam radiotherapy and is done daily, five days a week for about 5 weeks.
Other treatments
For patients with metastatic disease (cancer spreading to other parts of the body), and definite disease progression, newer agents called tyrosine kinase inhibitors such as Cabozantinib and Vandetanib can be used. Chemotherapy can also be used in this setting, but the benefit from them is small. Chemotherapy drugs used include Dacarbazine, Cyclofosfamide and Vincristine.
Anaplastic Carcinoma of the thyroid is an aggressive form of thyroid cancer. It is usually diagnosed in older people after the age of 60 and makes up about 5% of all thyroid cancers. It tends to grow very quickly, and treatment should be started very promptly.
Symptoms
The commonest symptom for this cancer is a thyroid mass. This can be associated with other symptoms such as neck pain, breathlessness, difficulty swallowing, cough or change in voice.
Other symptoms can reflect spread of cancer to other parts of the body.
Diagnosis
The diagnosis is made with the help of FNAC (fine needle aspiration cytology) or biopsy.
Treatment of Anaplastic Thyroid Cancer
Surgery
Surgery is done if the tumour remains confined to the thyroid gland. Total thyroidectomy is done in such circumstances. However, in most circumstances, surgical resection is not an option as there is spread of disease to other parts of the body. If surgery is done, radiotherapy and chemotherapy are given after surgery to maximise control. Radiotherapy if given is for about 5 weeks, given once daily, 5 days a week. Drugs used as chemotherapy are Doxorubicin, Taxanes and Cisplatin.
If the tumour is inoperable, a combination of chemotherapy and radiotherapy is used to control the disease. In patients who are not fit enough for combination treatment, radiotherapy alone is used.




