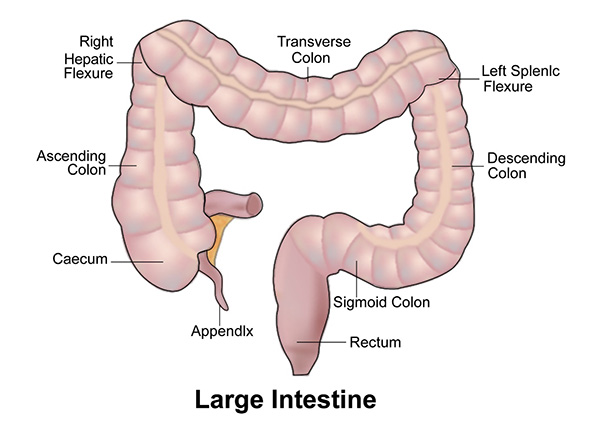
Colon is the part of the body called the large intestine. It is present in the abdomen and connects to the small intestine at one end and rectum at the other. It can be divided into the caecum, ascending colon, transverse colon, descending colon and sigmoid colon. The sigmoid colon continues as the rectum.
The food that is eaten is digested in the stomach and intestine. All the nutrients are absorbed in the small intestine and the digested food that is not required passes into the colon. Water that is present in this digested food is absorbed in the colon and the remaining waste passes into the rectum where it is stored before being excreted.
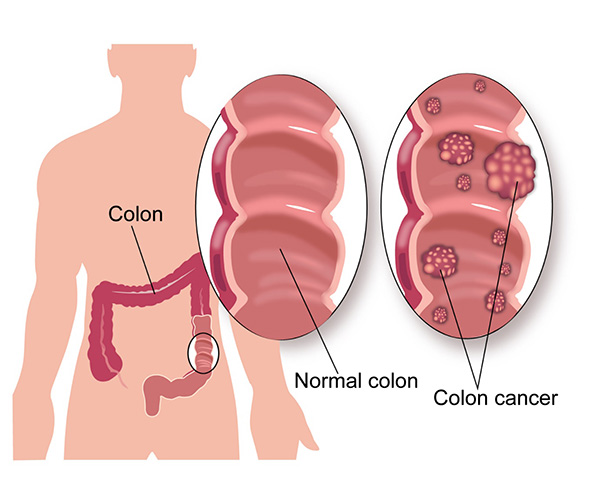
Cancer that starts in the colon is called as colon cancer. By far the commonest type of colon cancer is an adenocarcinoma. This type of cancer starts in the innermost lining of the colon called the mucosal layer. Colon cancer can spread from the mucosal layer into other layers of the colon and then to the outside of the colon. This type of spread is called direct spread. It can also spread through the lymphatic channels into the lymph nodes around the colon and to other parts of the body. The cancer also spreads through the blood stream to other parts of the body such as liver and lungs.
According to Globocan data 2018, there were 27605 new colon cancers diagnosed in India in 2018, making up 2.4% of all cancers.
Adenocarcinoma
There are various types of colon cancer, but the most common is adenocarcinoma which makes up around 95% of colon cancers. Adenocarcinomas originate from the lining of the mucosa layers present on the inside of the wall of the colon. The mucosa layers have gland-like cells from which this cancer arises.
Squamous cell carcinoma
These types of tumours are quite rare in colon cancer but seen. They arise from the squamous cells also present on the bowel wall.
Lymphomas
Lymphomas are cancers that develop from the lymphatic system such as lymph nodes. Lymphomas can arise from lymphatic tissue in any part of the body including the colon.
Carcinoid tumours
These are rare tumours that arise from the neuroendocrine cells present in the lining of the colon.
Sarcomas
Sarcomas are rare cancers that arise from the supporting structure cells in the body such as muscle, bone. The common type of sarcomas seen in the colon arising from the muscle cells present on the wall of the colon.
The treatment options for squamous cell carcinomas, lymphomas, carcinoid tumours and sarcomas are different to that of adenocarcinoma.
Age
Like all cancers which are more common in older age, the risk of colon cancer is more in patients in the older age group with the majority of cancers occurring in those aged over 60.
Genetic Factors
5% of colon cancers are passed on in families due to an abnormal gene. Genetic link to colon cancer is suspected if more than one close family member is affected with colon cancer at any age or one close relative had cancer diagnosed before the age of 45. A close family member is a first degree relative who could be a parent, child, brother or sister.
In the 5% of colon cancers that are due to faulty genes inherited from the family, the two conditions commonly seen are Familial adenomatous polyposis (FAP) and Hereditary non polyposis colon cancer(HNPCC). FAP leads to development of polyps in the colon at a young age which over time can turn into cancer. In those with confirmed FAP, surgery is recommended to remove the colon to reduce the risk.
HNPCC is a condition associated with colon cancer as well as other cancers such as pancreas, bladder, uterus and ovarian cancers.
Obesity and Physical Activity
Being obese is a risk factor for colon cancer. Also, lack of physical activity seems to increase the risk.
Diet
Diet rich in red and processed meat increases the risk of colon cancer. Rich diet of red and processed meat involves eating these foods on most days of a week. Consumption of red meat once or twice a week doesn’t increase the risk. A diet rich in fruit and vegetables reduces the risk of getting colon cancer.
Alcohol
Alcohol consumption increases the risk of developing colon cancer and the risk increases proportionally to the amount of alcohol taken.
Inflammatory Bowel Disease
Patients with a long history of inflammatory bowel disease such as Crohn’s disease and Ulcerative Colitis have a higher risk of developing colon cancer. This risk is increased after 10-20 years from diagnosis of inflammatory bowel disease.
Abdominal Radiotherapy
Adults who received abdominal radiotherapy as a child for cancer, have a higher risk of developing a colon cancer in adulthood.
Colon Cancer can present with a variety of symptoms and these are listed below
Change in bowel habit
Change in bowel habit is a common symptom seen in colon cancer. This change can be in the form of unexplained loose motions or constipation or alternating loose motions and constipation. These symptoms present for more than three weeks warrants investigations.
Blood in the motions
Passing blood from the anus or blood in the motions can be a symptom related to colon or rectal cancer. Most times, passing blood in the motions is not due to cancer and due to piles or other causes but it is important to see a doctor to have it checked out.
Abdominal Pain
Abdominal or tummy pain can be a symptom of bowel cancer. Again, there will be a number of causes for this symptom and tests need to be done to look for a cause if the symptom persists.
Other Symptoms
Other symptoms such as weight loss, tiredness, anaemia, distension of abdomen, vomiting can all be associated with colon cancer.
If colon cancer is suspected, the following investigations are usually done. Not all investigations are needed in every case.
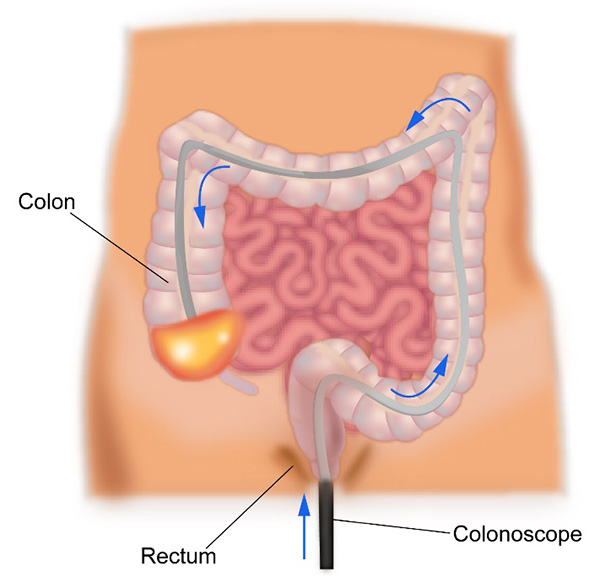
Colonoscopy
A colonoscopy is an endoscopic test where a thin tube with a light and a camera at its end is inserted into the anus and passed up into the rectum and colon. The doctor doing the test will be able to look at the inside of the colon on a screen and will be able to identify any abnormalities present in the colon. The whole of the colon can be seen through this procedure.
It is an outpatient procedure and is done under mild sedation to reduce the discomfort. If the doctor finds anything abnormal, a sample of the tissue can be taken(biopsy) for tests.
Also, sometimes small abnormal areas like polyps can be removed completely with this procedure. Before the colonoscopy, the patient is given medicines to take the day before to help empty the colon and rectum.
Flexible sigmoidoscopy
This test uses a similar tube as a colonoscope but is used to examine only the lower part of the colon and rectum. This is done as an outpatient procedure and usually does not need any sedation. An enema is given prior to the test to empty the rectum and lower colon.
Virtual Colonoscopy or CT Colonography
This test involves looking inside the colon with the help of a CT scan. The patient is given medicines the day before to empty the colon and advised regarding a specific diet for a few days before the scan. A CT scan is done to get detailed images of the colon. Any abnormalities present in the colon can be seen. The drawback of this test is that a biopsy cannot be done, and a colonoscopy needs to be done again to get a biopsy.
CT scan
Once a colon cancer is diagnosed on colonoscopy and biopsy, a contrast enhanced CT scan is done of the chest abdomen and pelvis to stage the cancer. This scan is used to look for spread of cancer from its point of origin to other parts of the body.
PET-CT Scan
A PET-CT scan is a PET scan combined with a CT scan. It involves injecting a special radioactive dye into the vein prior to the scan. This special dye will enable to detect cancer better than normal CT scan in certain circumstances.
In colon cancer, PET-CT is not recommended for routine staging but is recommended in settings when surgery is being considered to the liver or other organs or when standard CT scan is unable to determine clearly the presence or absence of cancer.
MRI Scan
An MRI scan is not routinely used to stage or diagnose colon cancer. It is used to assess the liver specifically when abnormalities present in the liver are suspicious for cancer or when liver surgery is being contemplated.
The stage of a cancer is a term used to describe the size and location of the cancer in the body.
Knowing the stage of the cancer helps the doctors to decide on the most appropriate treatment. Colon cancer is staged based on the TNM staging system or the number system.
Staging with either system is based on the extent of the tumour in the colon, the spread of the cancer in the colon and into the lymph nodes and spread of cancer into other parts of the body.
TNM stands for tumour, node and metastases. T stands for tumour and in colon cancer represents depth of spread into the wall of the colon. N stands for nodes and spread of cancer into lymph nodes around the colon. M stands for metastases and spread of cancer to distant areas in the body.
Number staging system
Based on the TNM stage of the cancer, colon cancer can be divided into stages 1 to 4 as below. Duke’s staging is another classification of Colon cancer. Duke’s staging is from A to D.
Stage 1
In stage 1, the cancer is limited to the colon and involves the part of the colon called the submucosa and muscularis layers. There is no involvement of the lymph nodes.
Stage 2
In stage 2, the cancer involves into the areas outside the colon or into surrounding organs without any involvement of the lymph nodes.
Stage 3
In stage 3 cancer, the tumour can involve any layer of the colon but there is definite involvement of the lymph nodes.
Stage 4
In stage 4, the cancer has spread to different parts of the body such as liver, lungs etc.
Overview of treatment of Colon Cancer
The treatment of colon cancer is dependent on the stage of cancer at diagnosis. The staging process will divide the colon cancer into non- metastatic, where disease is confined to one area of the colon and lymph nodes with no evidence of spread to distant sites in the body and metastatic cancer where cancer has spread from its site of origin to distant parts of the body.
Treatment also depends on the symptoms present at diagnosis irrespective of the cancer being metastatic or non-metastatic.
By and large, colon cancer that does not show distant spread is treated with surgical resection, where the part of the colon with the cancer and surrounding lymph nodes are removed. Details of surgery are given below. Following surgery, chemotherapy is advised based on the pathology results from the surgery. Chemotherapy given in this setting is called adjuvant chemotherapy where the purpose of it is to maximise the chances of a cure. In a few instances, adjuvant radiotherapy can be considered but this is not very common.
In patients with metastatic cancer, chemotherapy is usually the first treatment of choice. Here chemotherapy can be given on its own or along with biological agents, the details of which are discussed below.
In patients with metastatic disease but with symptoms suggesting of obstruction in the colon or a perforation in the colon, surgical resection is done first followed by chemotherapy. Patients with limited metastatic disease confined to parts of liver or lung are treated with surgery to remove the cancer in the colon and at metastatic sites.
Treatment of Colon cancer involves use of surgery, chemotherapy and sometimes radiotherapy.
Surgery
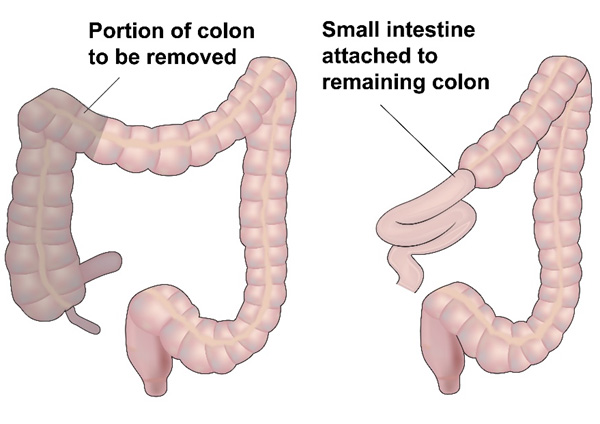
Surgery forms the main curative option of treatment for colon cancer. In colon cancer localised to the colon and surrounding lymph nodes, surgery aims to remove part of the colon and all lymph nodes in the region with the aim of curing the patient of the disease. Removal of lymph nodes is called as lymph node dissection and at least 12 nodes are to be removed to get a good result.
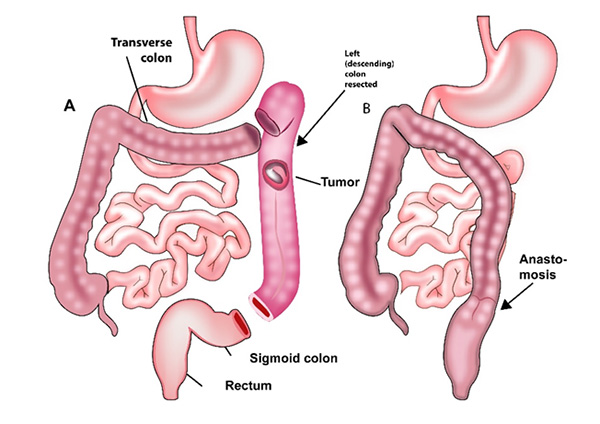
The surgery that is done is dependent on the location of the tumour in the colon.
The tumour present on the right side of the colon in the caecum or ascending colon will have a right hemicolectomy along with removal of lymph nodes around that part of the colon. This involves removing the right side of the colon, the appendix, the caecum and up to the transverse colon. An extended right hemicolectomy is done for cancers present in the hepatic flexure and this involves removal of a part of the transverse colon.
Tumours present in the transverse colon are removed with an extended right or left hemicolectomy depending on the location of tumour in the transverse colon. Occasionally a transverse colectomy is done.
Tumours on the descending colon are treated with left hemicolectomy and tumours in the sigmoid colon are treated with a sigmoid colectomy. The left hemicolectomy involves removal of a part of the transverse colon, the splenic flexure and descending colon and a part of the sigmoid colon.
A sigmoid colectomy is done for removing a tumour in the sigmoid colon.
The above surgeries are done by an open method, where an incision is made on the abdomen or through laparoscopic method. The laparoscopic surgery, when done by an experienced surgeon leads to quicker recovery after surgery. All surgeries are usually done under general anaesthesia.
After removal of the diseased colon, the remaining colon ends are attached and this is called an anastomosis. Sometimes, to allow the bowel to heal, an anastomosis is delayed and an ostomy is done. The involves bringing the end of the cut bowel as an opening onto the abdomen. A bag is attached to the ostomy, into which faeces and fluid collects. This ostomy is a colostomy, if the colon is brought out or an ileostomy if the end of the small intestine is brought out. This procedure can be reversed at a later date.
Surgery for Early colon cancer
In very early colon cancer, when the tumour is only limited to the innermost layer of the colon, local resection or endoscopic resection can be done. Here, a colonoscope is inserted into the colon and the seen tumour is cut out with a margin of normal colon as well. This is then reviewed by the pathologist. If resection is complete, no further treatment is necessary. However, if the resection is incomplete or there is evidence of involvement of the deeper layers of the colon, a standard colectomy as described above needs to be done.
Follow Up
Following curative treatment of colon cancer that includes surgery and possibly chemotherapy depending on the stage of disease, the patient should be closely monitored in the out patient clinic on a regular basis. This follow up is done for a period of five years with scans and colonoscopy in between. This process helps detect any recurrence of cancer earlier and enables effective treatment again quickly.
Surgery in Metastatic disease
In metastatic disease, surgical removal of the colon is sometimes done particularly when there is an obstruction to the passage of digested food in the colon. Here either an anastomosis is formed after removal or more commonly, a colostomy is done.
Colon cancer spreads to other parts of the body, commonly to the liver and lungs apart from other areas. Generally, when cancer spreads to distant areas of the body, curative surgery is not considered. However, in some colon cancers, when there is limited disease in the liver or lungs, surgery is done to remove the cancer altogether. This involves removal of a part of the liver or lung that contains the cancer in it. Many factors are taken into account regarding the suitability of the patient for surgery such as general fitness, amount of disease present, function of the relevant organ, response to previous chemotherapy and surgical expertise.
Chemotherapy is an important component of treatment for Colon cancer. Chemotherapy is given in a number of settings in this condition.
Adjuvant Chemotherapy
Adjuvant chemotherapy is given to patients after definitive surgical removal of the cancer. The purpose of adjuvant chemotherapy is to reduce the risk of recurrence of cancer after curative resection. Chemotherapy is definitely indicated in patients with stage 3 cancer and some patients with stage 2 cancer. The pros and cons of chemotherapy in this setting can be discussed with an Oncologist. The drugs commonly used are Fluorouracil, Capecitabine and Oxaliplatin. When Oxaliplatin is used, it is given in combination with Fluorouracil or Capecitabine. The duration of treatment can be up to 3-6 months and is given once every two or three weeks depending on the drugs selected.
Palliative Chemotherapy
Palliative chemotherapy is given when there is stage 4 cancer. The purpose of chemotherapy is to reduce the cancer and its symptoms and to prolong life.
Drugs used for stage 4 Colon cancer include chemotherapy drugs such as Fluorouracil, Capecitabine, Oxaliplatin and Irinotecan. Oxaliplatin is given in combination with Fluorouracil (FOLFOX) or Capecitabine (XELOX). Similarly, Irinotecan can be combined with Fluorouracil (FOLFIRI) or Capecitabine (XELIRI). These combination regimens are given once every two or three weeks depending on the regimen selected. The chemotherapy regimens can be combined with additional drugs such as antiangiogenic agents or anti EGFR antibodies, the details of which are listed below.
The duration of palliative chemotherapy ranges from 3-6 months for one drug or combination of treatment. The total duration of that particular regimen is dependent on response of the cancer to that treatment and the tolerance of the treatment by the patient.
Following completion of one regimen of treatment, further chemotherapy may be needed either soon after the first one or sometime later, depending on the status of the cancer at that time.
Chemotherapy prior to resection of metastatic disease
In some patients with stage 4 cancer, the disease is just confined to the liver which may be amenable for surgical resection. In such a setting, chemotherapy is given for around three months prior to liver resection to maximise the chances of good control of disease. This chemotherapy can be restarted after surgery and continued for a total of six months.
Anti EGFR antibodies
Anti EGFR antibodies are drugs that target the EGFR receptor present on the cancer cell. This stops the cells from growing. Two drugs that are used are Cetuximab and Panitumumab. These are given alone or in combination with chemotherapy. Not all patients with colon cancer benefit from these drugs. At the time of biopsy, a special test (RAS testing) is done to determine whether a KRAS or NRAS mutation is present in the tumour or not. If KRAS or NRAS mutation is present, these drugs will not be suitable. However, if KRAS or NRAS mutation is not present (KRAS wild type), these drugs will be beneficial. Both Cetuximab and Panitumumab are given through the vein and are usually well tolerated. Common side effects of these drugs include skin rash, diarrhoea, sore mouth and tiredness.
Anti Angiogenic Agents
Angiogenesis is growth and development of new blood vessels. Cancers need to develop new blood vessels to continue to grow. Anti angiogenic drugs stop the development of new blood vessels and in turn stop the progression of cancer. The drugs available are Bevacizumab (Avastin), Aflibercept (Zaltrap) and Regorafenib (Stivarga). These drugs can be given on their own or in combination with chemotherapy. They are suitable to be given in all patients with stage 4 colon cancer and do not need any special testing.




