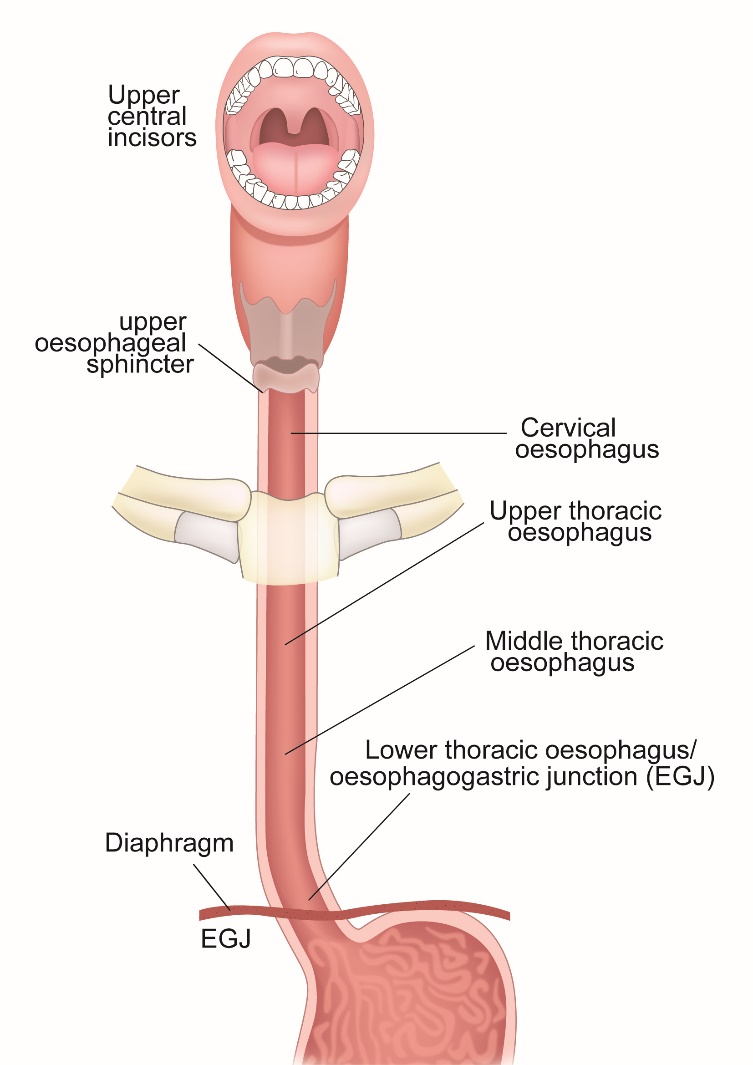
Oesophagus is a tube-like structure in the body that connects the mouth to the stomach.
It is about 25cm long and is made up of four layers, inside to outside- the mucosa, the sub mucosa, the muscle layer and the outer layer called adventitia. The food that is swallowed in the mouth reaches the stomach through the oesophagus. The muscle layer in the oesophagus helps propel the food through it. The junction where the oesophagus ends, and stomach begins is known as the oesophago-gastric junction.
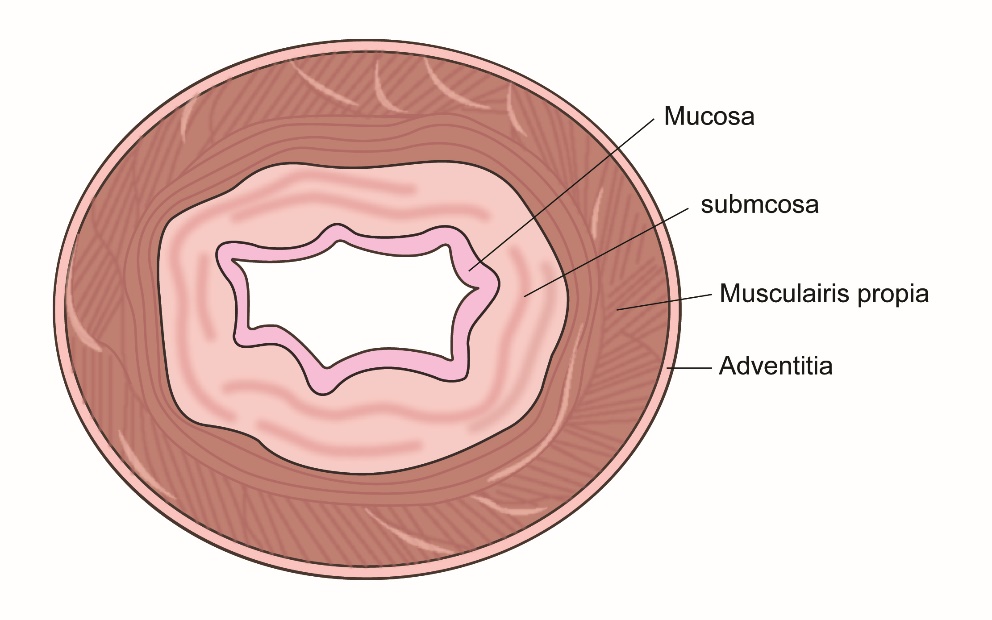
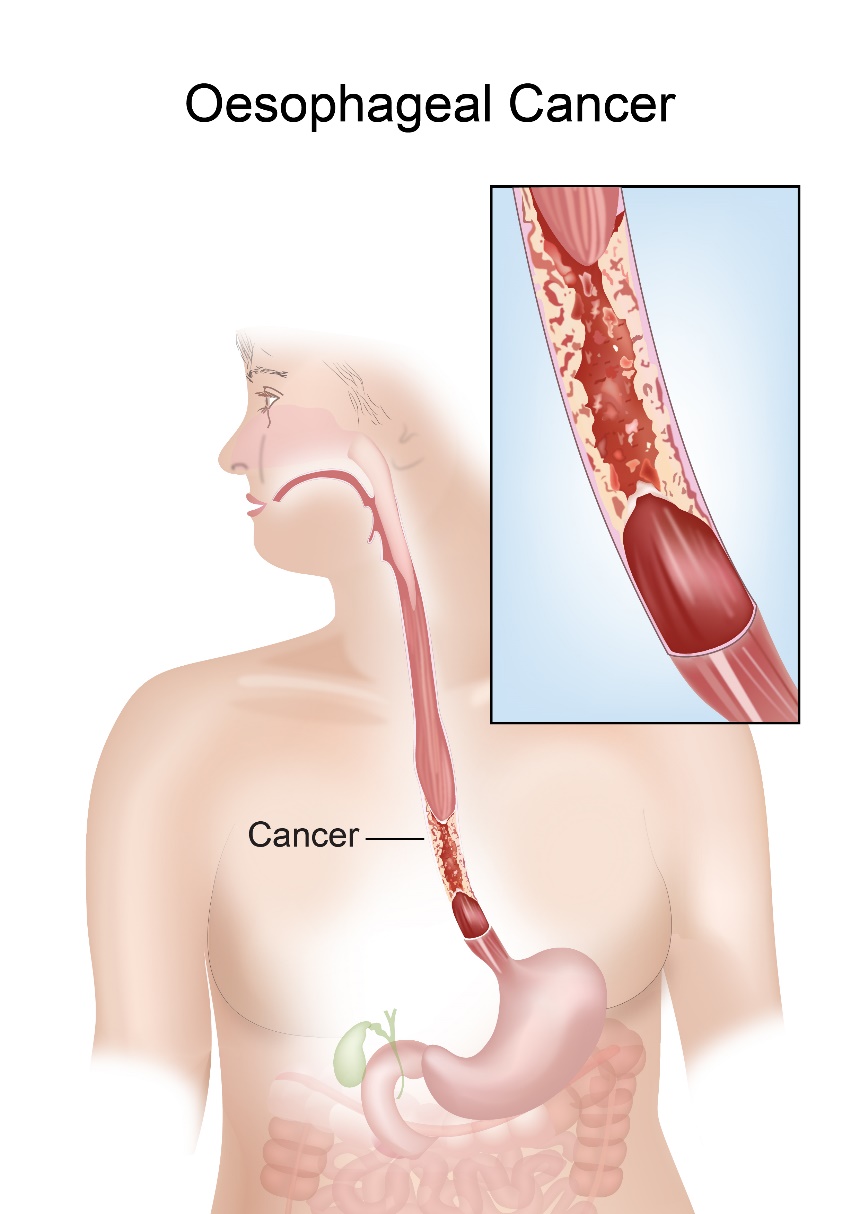
Oesophageal cancer is cancer that has started in the oesophagus. This cancer usually arises in the mucosa which is the inner lining of the tube. Oesophageal cancer can be a Squamous cell carcinoma or Adenocarcinoma. Squamous cell carcinoma arises from the cells lining the mucosa.
Adenocarcinoma arises from the glandular cells that produce mucus in the oesophagus. These two cancers make up over 95% of all oesophageal cancers.
There are various risk factors associated with Oesophageal cancer. These risk factors can be different for Squamous cell and Adenocarcinomas. Some risk factors are common for both types.
Smoking and Alcohol
Smoking and alcohol play an important role in the development of Squamous cell type of cancer. Cigarette smoking has a higher risk than smoking cigars. The total amount of alcohol consumed is the main determinant than the actual type of alcohol consumed.
Diet
Diet high in Nitroso compounds have a higher risk. Raw foodstuffs that are dried, pickled or smoked contain nitroso compounds.
Chewing of betel nut increases the risk. Consuming drinks that are very hot (very hot tea for example) may increase the risk by causing heat injury to the oesophageal lining.
Previous Oesophageal conditions
Having previous or underlying oesophageal conditions such as achalasia cardia, oesophageal strictures or atrophic gastritis increases the risk.
Obesity
Being overweight or obese leads to gasto-oesophageal reflux. Normally the junction of the stomach and oesophagus is closed very tightly and prevents the passage of acid from the stomach into the oesophagus. In obese patients, the junction becomes lax and allows the acid to pass into the oesophagus. This is called reflux disease and can lead to the development of a condition called Barrett’s Oesophagus. This can lead to the development of adenocarcinoma of the oesophagus.
Barrett’s Oesophagus
Barrett’s Oesophagus is a condition where the inner lining of the lower end of the oesophagus changes from one type to another due to persistent exposure to acid from the stomach. Having barrett’s oesophagus increases the risk of developing oesophageal cancer.
Tylosis
Tylosis is a rare form of inherited skin condition. People having this have an increased risk of developing oesophageal cancer.
Oesophageal cancers can produce many symptoms. Having any of these symptoms doesn’t mean that there is cancer, but it is important to see a doctor to have the symptoms investigated. Adenocarcinoma and Squamous cell carcinoma of the Oesophagus present in the same way.
Difficulty in swallowing
This is a common presenting symptom for people with oesophageal cancer. The difficulty in swallowing can initially be for solids and then for liquids. The symptoms are usually progressive and can be associated with loss of weight. Patients may notice that when the difficulty starts, it can be initially overcome by taking a sip of water.
Vomiting or regurgitation of food
Some people notice that food that was eaten before is vomited back or regurgitated into the mouth. Regurgitation of food means food that is swallowed comes back into the mouth without entering the stomach. This happens due to food not being able to go into the stomach after swallowing.
Pain on swallowing
Pain on swallowing can be a symptom and a sign for the presence of oesophageal cancer. The pain can be in the throat region or in the chest behind the breast bone.
Persistent symptoms of heartburn
Heartburn is a common symptom in the general population and is mainly due to non-cancerous conditions. But those people that have persistent heartburn or indigestion should see their doctor as this could be due to the presence of an oesophageal cancer.
Cough or change in voice
Hoarseness of voice and cough can be symptoms of oesophageal cancer.
Other Symptoms
Other symptoms that can be present in oesophageal cancer include vomiting of blood, weight loss or pain in abdomen, tiredness and swelling of the abdomen.
The following investigations are done when Oesophageal cancer is suspected or diagnosed.
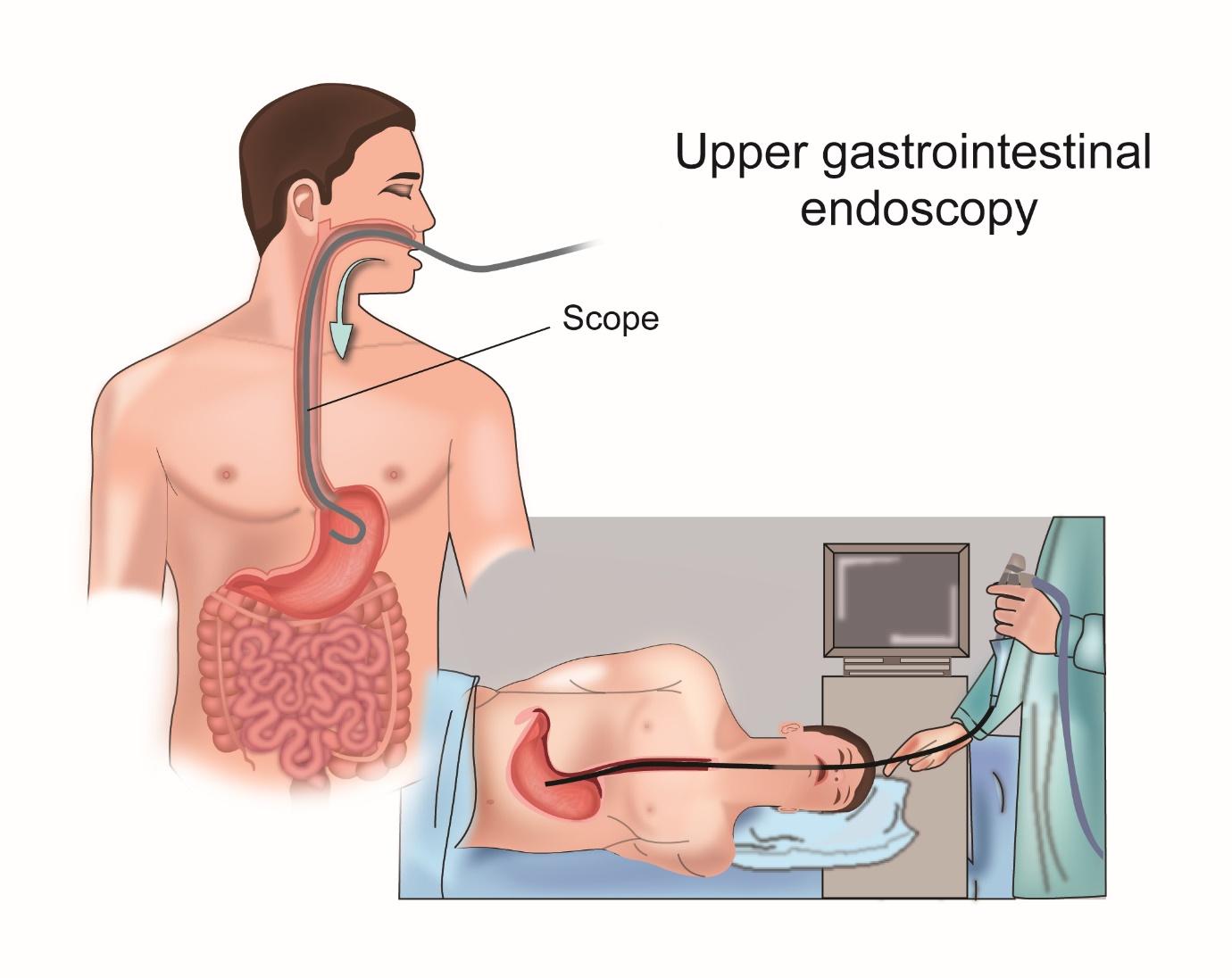
Upper GI Endoscopy
This is a test which involves passing a thin tube into the oesophagus and stomach to look for abnormalities. The tube has a light and a camera at the end of it so that that the doctor doing the procedure can see the oesophagus and stomach. The test is done using mild sedation and is painless.
It is a day case procedure, so the patient doesn’t need to stay overnight in hospital. If the doctor sees an abnormal area on endoscopy, a biopsy can be done at the same time.
CT Scan
A CT or computed tomographic scan is done once a diagnosis of oesophageal Cancer is made on endoscopy. The CT scan uses x-rays to get detailed images of the inside of the body.
Therefore, it can give information about whether the cancer has spread to other parts of the body.
PET Scan or PET-CT Scan
A PET–CT scan is a specialized CT scan where a radioactive tracer is injected into the body prior to the CT scan. This tracer lodges in areas within the body where there is high requirement for glucose. As cancers need a lot of glucose to survive, they take up the tracer much more than the rest of the body. The cancer can then be easily spotted on the scan. A PET-CT scan is more sensitive than a standard CT scan to look for evidence of spread of cancer. It is a very important test in staging of oesophageal cancer prior to treatment.
Endoscopic Ultrasound (EUS)
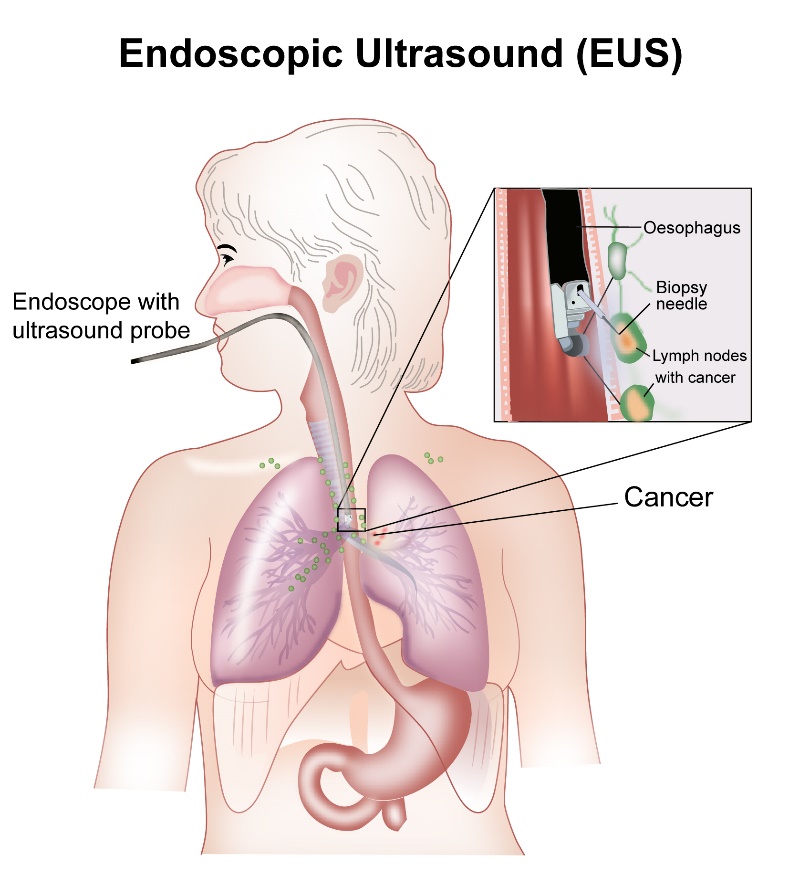
An Endoscopic ultrasound is a test that is like an endoscopy but has an ultrasound scanner at the end of it. This test uses sound waves to look for the depth of spread of cancer into the walls of the oesophagus. The scanner also helps to look for any enlarged lymph nodes that may be present around the cancer. The test is used to help get an accurate stage of the cancer and also to biopsy any abnormal nodes.
Laparoscopy
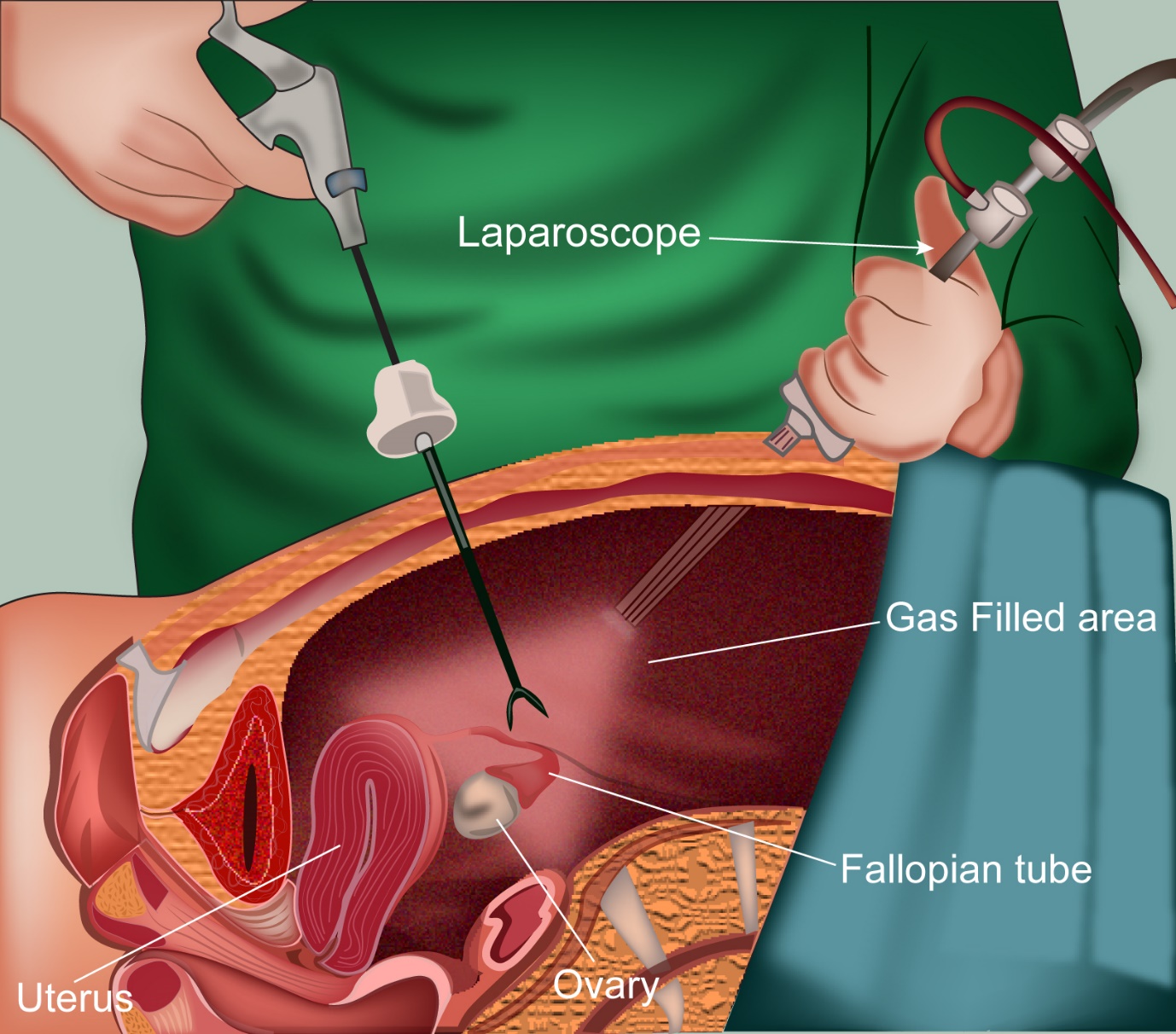
A laparoscopy is a test which helps the doctor to look inside the abdomen. This test is done in some patients with oesophageal cancer to look for evidence of spread of cancer into the abdomen.
The test is done under general anaesthesia and the patient will require a short stay in hospital.
It involves makes a small incision, about an inch in size around the umbilicus. A laparoscope is passed through the incision and the doctor can look inside. If needed, a biopsy can be taken. During the procedure carbon dioxide gas is passed into the abdomen to help get a better view inside. This CO2 gas will go away over time.
Oesophageal cancer is staged based on the TNM staging or the number staging. These two staging systems are listed below.
TNM Staging of Oesophageal Cancer
TNM stands for Tumour, Node and Metastases.
T Staging
T stands for tumour size. T is divided from T1 to T4. T staging in this cancer is based on the depth of spread of the oesophageal wall by the tumour.
| T1 | Tumour invades the lamina propria or sub mucosa |
| T2 | Tumour invades into the muscle layer of the Oesophagus |
| T3 | Tumour invades the outer layer (adventitia) of the oesophagus |
| T4 | Tumour crosses the oesophagus and invades other structures around the oesophagus |
N Staging
N Staging will depend on the involvement of lymph nodes around the oesophagus
| Nx | Lymph node involvement cannot be assessed |
| N0 | No involvement of lymph nodes by the cancer |
| N1 | Involvement of 1-2 lymph nodes by the cancer |
| N2 | Involvement of 3-6 lymph nodes by the cancer |
| N3 | Involvement of 7 or more lymph nodes by the cancer |
M Staging
M staging gives information about whether there is spread of cancer to distant parts of the body
| M0 | No evidence of distant spread of cancer |
| M1 | Presence of distant spread of cancer |
Number Staging
This type of staging stages the cancer from stage 1 to 4 depending on the TNM classification. This staging system in Oesophageal cancer is different for Squamous cell cancer and Adenocarcinoma types. Adenocarcinoma is shown below.
Number staging for Adenocarcinoma
- T1 N0 M0————Stage 1
- T1 N1 M0————Stage 2A
- T2 N0 M0————Stage 2B
- T2 N1 M0————Stage 3
- T2 N0-1 M0———Stage 3
- T4a N0-1 M0——-Stage 3
- T1-4a N2 M0——-Stage 4a
- T4b N0-2 M0——-Stage 4a
- Any T N3 M0——-Stage 4a
- Any T Any N M1—Stage 4b
Grade of Cancer
Grading of cancer is based on how cells look under the microscope. The grading can be from 1 to 3 or 4 in some cancers. Grade 1 being cells looking like normal cells and grade 4 being cells that don’t resemble normal cells at all.
Grades of Oesophageal Cancer
Grade 1- the cells in the cancer are well differentiated (look like normal cells)
Grade 2-The cells in the cancer are moderately differentiated
Grade 3-The cells in the cancer are poorly differentiated (don’t look like normal cells)
Grade4-The cells are undifferentiated (look completely different)
Oesophageal cancer can be treated with Surgery, Chemotherapy, Radiotherapy or a combination of these methods. The precise mode of treatment depends on the stage of cancer at diagnosis and the general physical condition of the patient.
In early Oesophageal cancer, the aim of treatment will be to cure the patient with treatment.
In advanced cancer (stage 4 or bulky stage 3), a cure may or may not be possible, but treatment is given to reduce the cancer and control it.
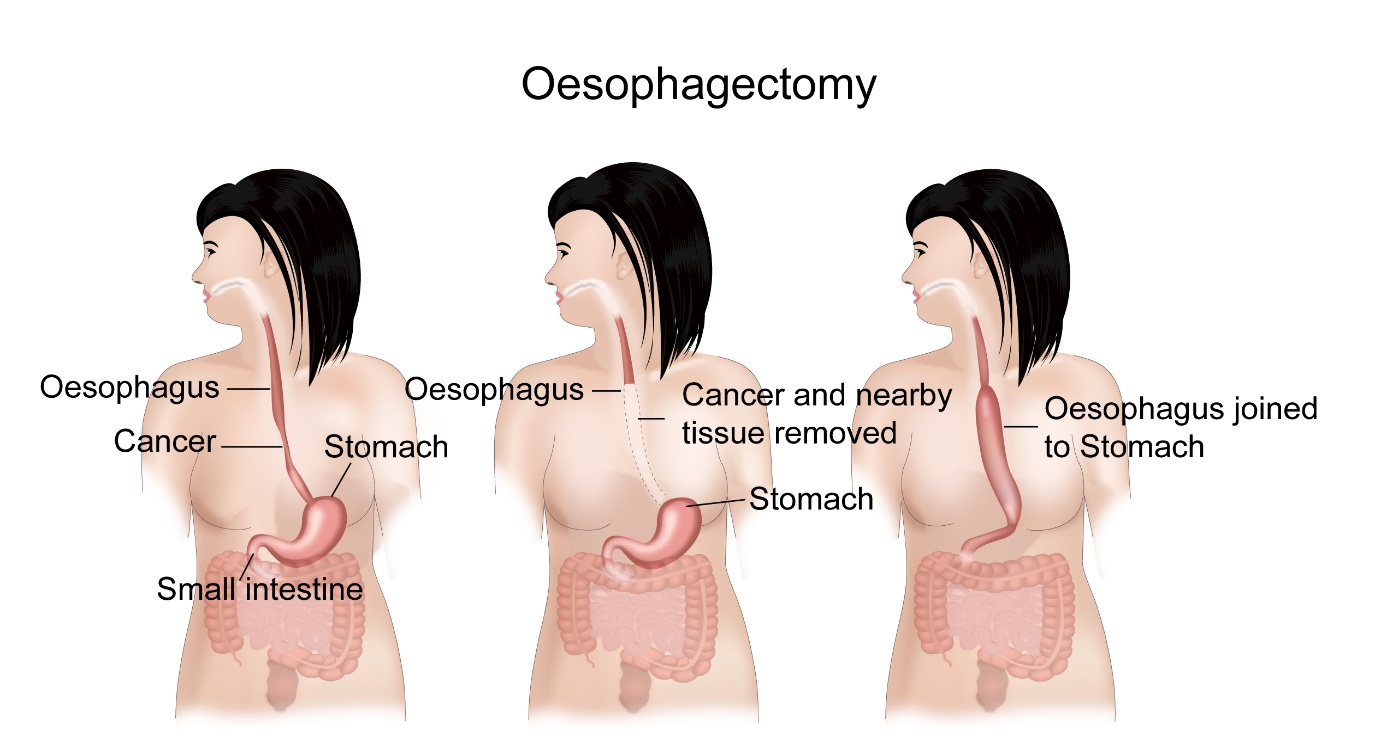
Surgical removal of Oesophageal cancer is a common and an important component of treatment of oesophageal cancer. Removal of the oesophagus is called an Oesophagectomy.
Oesophagectomy is an option in the management of stages 1, 2 and 3 oesophageal (squamous cell or adenocarcinoma) cancers. It is not an option in the management of stage 4 cancer.
Oesophagectomy involves taking out the section of the oesophagus containing the cancer and joining the remaining sections together. The stomach is usually pulled up into the chest to join the remaining oesophagus. Sometimes a part of the colon (large intestine) may be needed to attach the two cut sections together. If the cancer is in the lower oesophagus or at the junction of the oesophagus and stomach, then a part of the stomach is also removed to get adequate margins around the cancer. During the operation, the surgeon will also remove lymph glands present around the oesophagus.
At the time of the operation, a feeding tube can be placed to allow the patient to get all the nutrition he/she needs while recovering from the surgery. This feeding tube can be a feeding jejunostomy where the tube is placed in the small intestine called the jejunum or a gastrostomy, where the tube is in the stomach. These tubes come out of the skin and food and fluids could be pushed inside through the tube.
Types of Surgery
The surgery can be done in three ways-
Trans-thoracic Oesophagectomy-
where incisions are made on the chest and abdomen
Trans-hiatal Oesophagectomy-
where incisions are made in the neck and abdomen
Three-incisional Oesophagectomy-
incisions are made in the neck, chest and abdomen
All three ways are equally effective, and the choice of method depends on the location of cancer and the experience of the surgeon.
Some people may be able to have the operation using keyhole surgery. This is done using a thoracoscope in the chest and a laparoscope in the abdomen.
For operable stage 1 Oesophageal cancer (squamous cell or adenocarcinoma), surgical removal on its own is the treatment of choice provided the patient is fit enough to undergo the operation.
For operable stage 2 and 3 patients, Chemotherapy or combination of Chemotherapy and Radiotherapy (Chemoradiotherapy) is considered prior to surgical removal. Exactly which option to use will depend on the fitness level of the patient.
Following surgery, most patients will spend a few days in intensive care and then be transferred to the ward. Getting back to eating normally will take time and eating habits will usually be different to before the operation. This is because of the change in shape and size of the gullet and the stomach after the operation. The patient may have to eat small meals more often in the day.
Also, the patient may have to take antacids and anti-diarrhoea pills to control symptoms of acid reflux and diarrhoea.
Another side effect after oesophageal and stomach surgery is dumping syndrome. This is a sensation of feeling faint after eating food. This is a common occurrence after this type of surgery and can be reduced by eating slowly, reducing very sugary contents in the diet and eating smaller diets more frequently.
Chemotherapy
Chemotherapy is use of anti-cancer drugs given in the form of injections, drips and tablets. These drugs help kill cancer cells by causing maximum damage to them and at the same time causing some damage to normal tissues. The side effects that happen as a result of Chemotherapy are due to the effect of these drugs on normal tissues. There are a number of Chemotherapy drugs used to treat Cancer. These drugs can be used either in combination or as single agents. Chemotherapy is given as cycles, with each cycle lasting between 1 to 4 weeks, usually 3 weeks. The gap between two Chemotherapy cycles is for the body to recover before the next dose. A course of Chemotherapy usually lasts for some months.
Chemotherapy For Oesophageal Cancer
Chemotherapy is an important component of treatment for Oesophageal Cancer. Chemotherapy is given in different settings in oesophageal cancer.
In stage 1, 2 and 3 Cancers, Chemotherapy can be given along with Radiotherapy. This option is called concurrent Chemoradiotherapy. There, it can be given either once a week or once every three weeks or in the first and last week of radiotherapy. The best strategy will depend on patient’s capacity to tolerate Chemotherapy and patient’s convenience.
In some settings, Chemotherapy can be given prior to surgical removal of oesophageal cancer. This is called neoadjuvant Chemotherapy. Chemotherapy can sometimes be given after surgical removal. This is called as adjuvant Chemotherapy.
In stage 4 Cancer, chemotherapy is used as a combination treatment to control the cancer and the symptoms that the cancer is producing.
The purpose of chemotherapy in stages 2 and 3 is to cure the patient from the cancer and in stage 4 is to control the cancer and prolong life.
Commonly used chemotherapy drugs in oesophageal cancer include
Epirubicin, Doxorubicin, 5 Fluorouracil (5FU), Capecitabine, Cisplatin or Carboplatin, Oxaliplatin, Irinotecan, Docetaxel, Paclitaxel and Trastuzumab.
When these drugs are used as combinations, the common combinations are
DCF (Docetaxel, Cisplaitin and 5FU)
ECF (Epirubicin, Cisplatin, 5FU)
ECX (Epirubicin, Cisplatin, Capecitabine)
EOX (Epirubicin, Oxaliplatin, Capecitabine)
FOLFOX (Oxaliplatin and 5FU)
XELOX (Oxaliplatin and Capecitabine)
Cisplatin and 5FU
HER2 Testing and Trastuzumab
HER2 is an epidermal growth factor receptor 2, which when increased in oesophagogastric cancer can lead to increase of the cancer. Up to 35% of all oesophago-gastric cancers are HER2 positive and this should always be tested for at the diagnosis of the cancer. The HER2 status is tested on the cancer specimen that is got on biopsy or at surgery. This test will tell whether Her2 is amplified or increased in the cancer by giving a result of 3+. Sometimes, the initial HER2 test is equivocal(2+), when a further test (FISH) is required.
If HER2 test is positive, antibodies against the HER2 receptor are available and used as treatment for this type of cancer.
Trastuzumab is an antibody for HER2 receptor and use of this drug along with chemotherapy in Her2 positive patients provides additional benefit. This drug is only used with chemotherapy in stage 4 patients.
Side effects of chemotherapy
Chemotherapy for Oesophageal Cancer is associated with side effects. These depend on the drugs that are administered. Some of these side effects can be well controlled with medications. Tolerability of Chemotherapy varies from person to person. Some people cope with treatment very well without any side effects, while other may have side effects. common side effects are
Hair loss
This is common with the above mentioned Chemotherapy regimens. Hair loss usually starts after the second week of the first cycle. Hair grows back after Chemotherapy is finished. Some centres may offer a “cold cap” service which can reduce the chance of hair loss.
Nausea and vomiting
This is a known side effect of Chemotherapy, but with modern medications, these symptoms are very well controlled.
Tiredness
Tiredness is a common side effect. It is usually more in the first week and then gradually improves after that.
Soreness in the mouth
Common after Chemotherapy. This will settle by itself and it is recommended to use a mouth wash 3-4 times a day to keep the mouth clean.
Loose Motions
This symptom can occasionally occur after chemotherapy. Speak to your doctor if it happens as it can be controlled well with medications.
Constipation
Constipation is a common side effect of Chemotherapy. This can happen as a result of the Chemotherapy drug itself but mainly it is due to the effect of the anti nausea drugs that are given along with Chemotherapy. Constipation happens in the first few days of Chemotherapy.
Risk of Infection
This is an important side effect of Chemotherapy. It happens as Chemotherapy reduces the capacity of the body to fight infections. Therefore, it is very important to contact a doctor urgently if there is a fever at any time (even if it is in the middle of the night) during Chemotherapy.
Taste changes
This is common with Chemotherapy and therefore food wont taste as before. Taste will recover after Chemotherapy is finished.
Tingling in Hands and feet
Some Chemotherapy drugs produce this side effect. Report them to the doctor at your next visit.
Anaemia
This can happen as a result of Chemotherapy. Usually this can just be observed and it will improve after treatment finishes. Sometimes blood transfusion or other treatment is necessary to improve it.
Bleeding
There is a small risk of bleeding with Chemotherapy. If this happens, you need to contact your doctor straight away.
Cough, Breathlessness or swelling of feet
These effects can happen in patients having Trastuzumab and should be reported to the doctor if they happen.
What is Radiotherapy
Radiotherapy is the use of high energy x-rays given to kill cancer cells. These x-rays cause damage to the DNA of the cancer cells and thereby kill them. Radiotherapy is a local treatment and has its effect in the area that it is given to. It is given using a large machine (Linear accelerator) which generates the x-rays and delivers the treatment to the patient. This method is called as external beam therapy. The other way to give radiotherapy is to insert radioactive sources into the cancer itself. This method is called Brachytherapy and is used to treat some types of oesophageal cancers.
Radiotherapy for Oesophageal Cancer
Radiotherapy is an important component of treatment for Oesophageal Cancer. It is used to treat all stages of oesophageal Cancer (stages 1 to 4). In stages 1, 2 and 3, Radiotherapy is used with a curative intent which means it aims to get rid of the cancer completely without it coming back in the future. In such circumstances, treatment is given daily, five days a week for five to seven weeks.
In stage 1 Oesophageal cancer, Radiotherapy is used in patients who are not fit to have Surgery. In that setting, Radiotherapy is given along with Chemotherapy (Chemoradiotherapy) or on its own depending on the fitness of the patient.
In stage 2 and 3 patients, Chemoradiotherapy or Radiotherapy is given either as treatment on its own or prior to curative surgery again depending on the fitness of the patient.
In stage 4, Radiotherapy is used mainly to control symptoms. Here, it is given over a shorter period lasting 1 to 3 weeks. Brachytherapy can also be used in stage 4 patients. It involves putting a radioactive source into the oesophagus for a brief period to deliver the radiation locally. This treatment can be used on its own or can be combined with external beam radiotherapy.
When chemoradiotherapy is used, the chemotherapy is given in two fashions depending on the drugs used. Commonly, this is in the form of chemotherapy once every week during radiotherapy or continuously for 5 days in the first and last week of treatment.
Radiotherapy can be given using different techniques and these are listed here below.
3D conformal Radiotherapy
This is a way of planning and giving Radiotherapy, where CT, MRI scans are used to get a three-dimensional image of the tumour. This allows the planning process to be made in three dimensions.
It allows the Radiation treatment to be more precise than standard 2D radiotherapy.
Intensity modulated Radiotherapy (IMRT)
IMRT is a type of 3D conformal treatment planning and delivery method, where radiation beams can be precisely shaped to fit the shape of the tumour. This helps in minimizing toxicity to surrounding normal structures in the body. The difference between IMRT and 3D conformal radiotherapy is that IMRT can be more precisely shaped to fit the shape of the tumour. Therefore, side effects will be lesser. Also, with IMRT, there is the possibility of delivering different doses of radiotherapy to different parts of the same tumour. IMRT is done by using multiple radiation beams directed at the tumour from different angles.
Arc based Treatment
Arc based therapy (Rapid Arc, VMAT) is delivery of radiotherapy with the linear accelerator going around the patient in an arc like fashion. This type of therapy can be more precise than standard IMRT and quicker to deliver. It is also more expensive.
Image guided Radiotherapy (IGRT)
Image guided radiotherapy is the use of imaging systems such as CT scanners to monitor treatment accuracy. Normally, in standard 3D conformal radiotherapy, a CT scan is done prior to start of treatment for planning purposes. In IGRT, a CT scan or x-ray can be done prior to every radiotherapy treatment to test for accuracy of the treatment.
Side effects of radiotherapy to Oesophagus
The side effects associated with radiotherapy to the oesophagus depend on the dose of radiotherapy given, the duration of treatment and the area that is being treated. Side effects will be more in patients having chemoradiotherapy and radiotherapy with intention of cure as dose of radiotherapy will be higher.
Side effects of oesophageal radiotherapy include tiredness, nausea and vomiting, acid reflux and burning sensation in the chest, sore throat and difficulty swallowing, stricture (narrowing of oesophagus), cough and breathlessness. The side effects can be acute, where they happen during and immediately after treatment or late when they happen more than 3 months after treatment. Acute side effects take about 4 weeks to improve after completion of treatment.
Managing Swallowing Difficulty
In patients who have swallowing difficulty and are not able to take an adequate diet, a feeding tube can be placed to allow the patient to get all the nutrition he/she needs while receiving the treatment and recovering from it. This feeding tube can be a feeding jejunostomy where the tube is placed in the small intestine called the jejunum or a gastrostomy, where the tube is placed in the stomach. These tubes come out of the skin and food and fluids could be put inside through the tube.
Immunotherapy with Pembrolizumab can be used in patients who are PD-L1 positive or have high levels of microsatellite instability (MSI) and have very advanced or metastatic oesophageal cancer. This treatment may not be suitable for all patients in this setting. Pembrolizumab may also be used as a later line of treatment after chemotherapy in above mentioned patients.
Insertion of oesophageal stents is an option in patients who have cancers and are not able to swallow food. Stents help in opening of the lumen of the oesophagus allowing food to pass through. A stent is a metallic mesh wire that is inserted into the oesophagus by endoscopy. Once it is in place, it can be expanded. Side effect of stent placement include discomfort in the chest, pain and heartburn.




