Immunotherapy FAQ’s
What is Immunotherapy in cancer?
Immunotherapy is the use of drugs that modify the immune system to help control and treat cancer.
What is the immune system and what is its function?
The immune system in the body consists of white blood cells in the blood, the bone marrow, lymph nodes present all over the body and organs such as the spleen. All of these help the body to fight off infections and external threat that the body receives.
Does the Immune system kill cancer?
The body’s immune system has the capacity to identify external threats such as bacteria, viruses etc and differentiate them from host cells. Therefore, when the immune system is activated in the presence of these external threats, the system kills off these threats but does not cause any damage to normal cells of the host.
When cancer develops in the body, the immune system either does not identify the cancer as foreign and therefore does not try to destroy it or identifies it but is unable to kill it. The cancer also grows and mutates in such a way that it avoids detection by the immune system.
How does Immunotherapy work?
Immunotherapy consists of a number of drugs that modify the immune system by for example-identifying the cancer cells as foreign, by enhancing the potency of the immune system by altering the mechanism.
What are the different types of Immunotherapy available?
There are many different types of Immunotherapy available and some of these are listed below.
Checkpoint Inhibitors
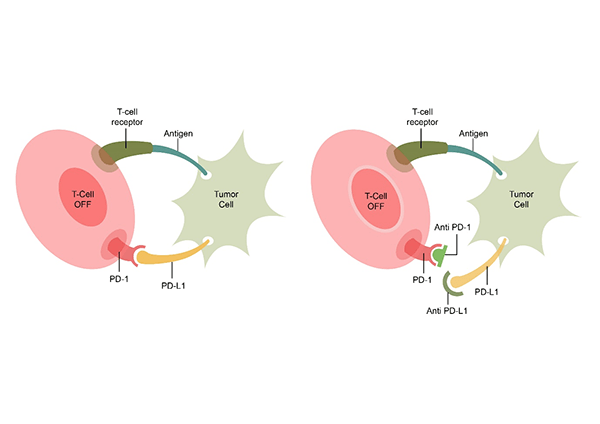 These drugs are monoclonal antibodies (mabs) that attach themselves on the surface of cancer cells making them more visible to the immune system. The system then is enabled to kill the cancer cells. A number of these checkpoint inhibitors are available for treatment in cancer. They are usually used in stage 4 cancer and help to control the cancer and prolong life. They are not able to cure cancers completely. Some of the checkpoint inhibitors used include Nivolumab, Pembrolizumab, Atezolizumab, Avelumab, Durvalumab etc. The below diagram shows how the checkpoint inhibitors work. The T Cell receptor on the body’s immune cell (T Cell) binds with the antigen of the cancer cell. Also, below, the PD-1 receptor and PD-L1 ligand combine. This combination inhibits the destruction of the cancer cell by the T Cell. In the second image, there is blockage of the PD1 and PD-L1 by checkpoint inhibitors(either anti PD-1 or anti PD-L1). This then leads to activation of the T cell and destruction of the cancer cell.
These drugs are monoclonal antibodies (mabs) that attach themselves on the surface of cancer cells making them more visible to the immune system. The system then is enabled to kill the cancer cells. A number of these checkpoint inhibitors are available for treatment in cancer. They are usually used in stage 4 cancer and help to control the cancer and prolong life. They are not able to cure cancers completely. Some of the checkpoint inhibitors used include Nivolumab, Pembrolizumab, Atezolizumab, Avelumab, Durvalumab etc. The below diagram shows how the checkpoint inhibitors work. The T Cell receptor on the body’s immune cell (T Cell) binds with the antigen of the cancer cell. Also, below, the PD-1 receptor and PD-L1 ligand combine. This combination inhibits the destruction of the cancer cell by the T Cell. In the second image, there is blockage of the PD1 and PD-L1 by checkpoint inhibitors(either anti PD-1 or anti PD-L1). This then leads to activation of the T cell and destruction of the cancer cell.
PD-L1 Status
The level of PD-L1 present in the cancer can be checked with a test. This test is done in certain cancers when a drug such as Pembrolizumab is planned to be given. The result of the PD-L1 status come as a percentage and this allows the drug to be used in certain settings. PD-L1 testing is now done routinely in lung cancer patients.
Cytokines
Cytokines are substances that are normally produced by the immune system to boost the response. These cytokines such as Interleukin and Interferon when given as an injection can enhance the effect of the immune system on cancer and help to control it. Cytokines have been used as cancer treatments for a number of years. Their benefit is mild and are used in cancers of the skin(melanoma) and kidney.
Cancer Vaccines
This type of treatment involves injecting a vaccine treatment that has been primed with the patient’s own cancer. This vaccine helps control the cancer. This is an exiting mode of treatment but only one such treatment is currently available for Prostate cancer and has not been shown to be very effective.
Adoptive Cell Therapy
Car T Cell Therapy
A new type of immunotherapy and one of the types of adoptive cell therapy where the patient’s T lymphocytes (type of white blood cells) are removed from the bloodstream and are reprogrammed to express chimeric antigen receptors (CAR). These receptors are present on the surface of these T-cells and when injected back into the patient will enable the cells to track and kill cancer cells. This therapy has been found to be very effective and is used to treat certain blood cancers in children. It is currently very expensive.
Do Immunotherapy treatments have side effects?
Yes, immunotherapy treatments have side effects, some of them could be serious and life threatening. Saying that, overall the side effects of immunotherapy drugs in general are less than those of chemotherapy. Regular tests, especially blood tests are done to look for potential side effects of these drugs. When the immune system is activated or enhanced, there is a risk of the treatment damaging normal cells also and has to be closely monitored by blood tests and how the patient is feeling.
Do Immunotherapy treatments work every time?
Like all other treatments in cancer, immunotherapy treatments do not work in every patient. The chances of response to these drugs varies from the cancer being treated to the drug being used. In those patients where there has been a good response of the cancer to these treatments, these responses tend to last for a longer period of time.




