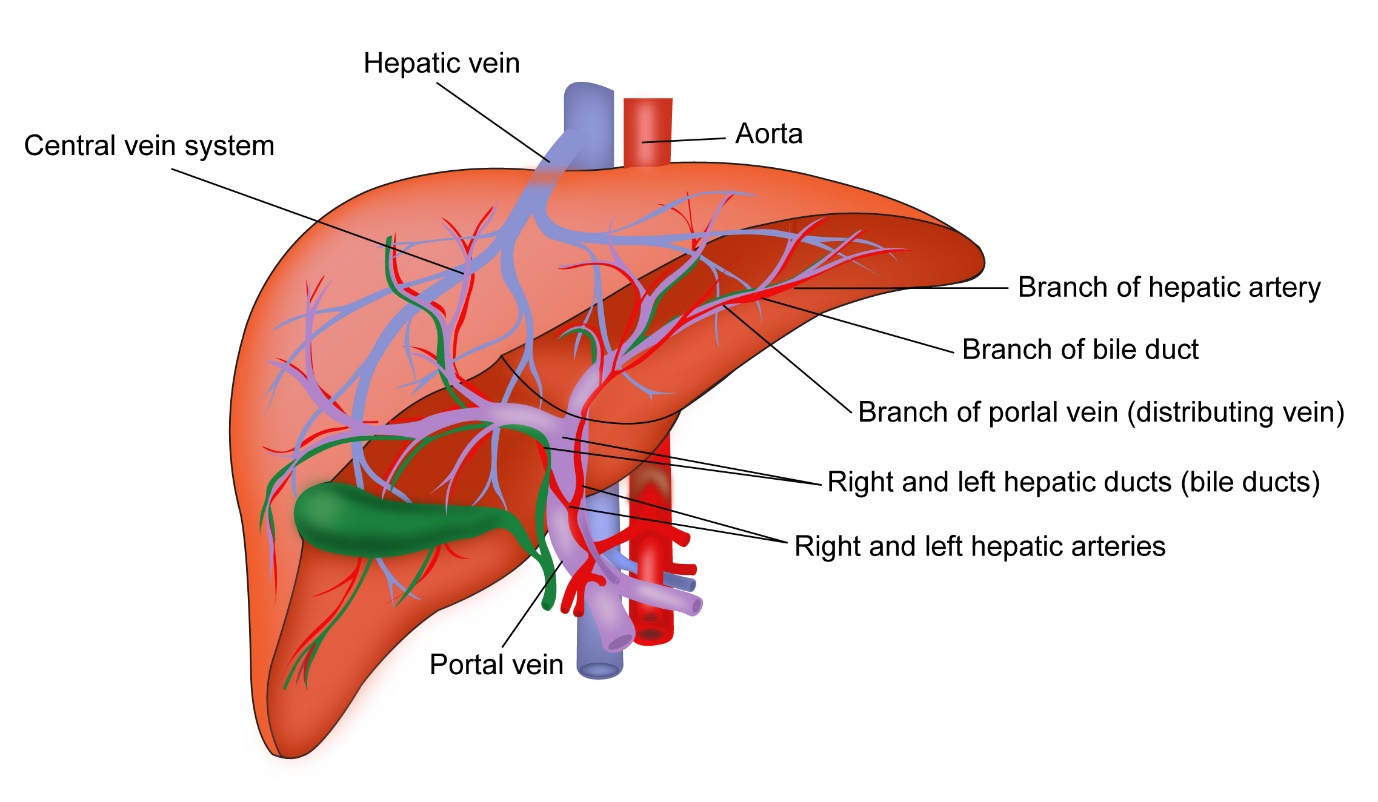
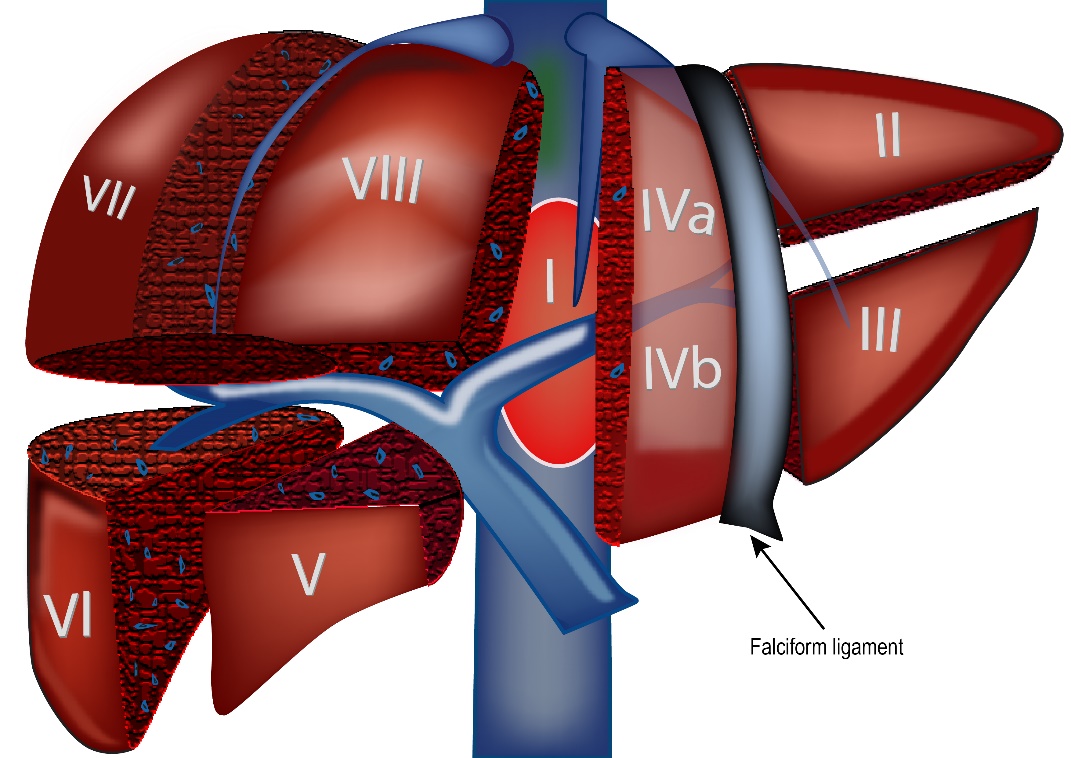
Liver is the largest organ in the body and is present on the right side of the upper abdomen. The liver is made up of two lobes, right and left lobes divided by the falciform ligament. The liver is also divided into 8 segments from 1 to 8. The liver is enclosed in a thick layer called the capsule.
The liver has a number of functions in the body including making of proteins that the body needs. It helps in conversion of digested food into fats and glycogen, which is then stored in the body. It helps in conversion of these foods back into glucose when the body needs it. It produces bile which helps indigestion of food.
Liver cancer is cancer that has started in the liver. It is also known as Hepatocellular carcinoma. It develops from hepatocytes which are the main cells in the lover. Many cancers that have started in other parts of the body can spread into the liver and these are called as secondary liver cancers. According to Globocan data 2018, there were 27,670 liver cancers in India making up 2.4% of all cancers.
Other cancers which start in the liver but are not Hepatocellular carcinomas include lymphomas, sarcomas, hepatoblastomas and neuroendocrine tumours.
This topic is about primary liver cancers which have started in the liver itself.
There are a number of risk factors that can lead to the development of Liver cancer. These are
Cirrhosis
Cirrhosis is a disease of the liver where there is scarring of the liver leading to reduction in size and change in architecture of the liver. This leads to poor liver function. Cirrhosis is caused due to a number of conditions such as excessive alcohol intake, infections with Hepatitis B or C or other conditions such as primary biliary cirrhosis or haemochromatosis.
Alcohol
Intake of excessive alcohol leads to development of Cirrhosis which in turn can lead to the development of Liver Cancer
Non Alcoholic Fatty Liver Disease (NAFLD)
This is a condition where there is excessive accumulation of fat in the liver leading to cirrhosis which then can lead on to development of Liver cancer. This condition is seen more often in patients with Diabetes and Obesity.
Smoking
Smoking is an independent risk factor for developing hepatocellular carcinoma. Smoking along with above risk factors increases the risk even more.
Other causes
Other causes for hepatocellular cancer include reduced immunity due to drugs or infections such as HIV/AIDS, a strong family history of liver cancer. Aflatoxin, which is a toxin present on peanuts, corn, wheat and rice that have been affected by mould(fungus) is a risk factor for liver cancer. Similarly chemicals such as Benzene are also risk factors. Chewing of betel nut is also considered as a risk factor.
Liver cancer does not produce any symptoms when it is small. The symptoms that are seen include tiredness, loss of weight, loose motions, reduced appetite and fever. A mass that can be felt in the abdomen usually suggests an advanced cancer.
Liver cancer is seen in patients with previous liver disease such as Hepatitis B and C, Cirrhosis and other liver conditions. When a liver cancer develops in patients with these conditions, the symptoms related to these conditions worsen. These can be worsening jaundice(yellowing of eyes and skin), bleeding, development of fluid within the abdomen(ascites).
The following investigations are done to help in diagnosis of Liver Cancer
Blood Tests
A range of blood tests are done to help in diagnosis of Liver Cancer and to make decisions regarding best option of treatment.
Blood tests done include
AFP or Alpha Fetoprotein is a protein detected in the blood in patients with liver cancer. Presence of raised AFP in the blood helps in the diagnosis. Some liver cancers do not produce AFP and hence AFP level is not raised in all Liver cancers.
Tests for Hepatitis B and Hepatitis C are also done to confirm or exclude the presence of this infection as this is a risk factor for development of Liver Cancer.
Other routine blood tests done include tests for Liver function(LFT), kidney function and CBC.
Ultrasound Abdomen
An ultrasound abdomen is usually the first scan that is done for symptoms. The scan is able to show the abnormality present in the Liver which raises the suspicion of the presence of cancer. Further scans are needed if this test shows the abnormality.
CT Scan
A CT scan of the liver is one of the main tests used to diagnose a liver cancer or Hepatocellular carcinoma as it is called. This CT scan of the liver is different to the CT scan that is done for other reasons. If a primary liver cancer is suspected, then a triple phase CT scan is needed to accurately scan the suspected area. In patients where contrast material cannot be injected to get a triple phase scan, then an MRI scan is done.
MRI Scan
An MRI scan of the abdomen is as good as a CT scan in making a diagnosis of Primary liver cancer. In some instances, an MRI and CT scan are both needed to make a diagnosis.
PET Scan or PET-CT Scan
The benefit of PET scanning in primary liver cancer is limited as it is not very sensitive in picking up liver cancer. Therefore, this type of scan is not routinely recommended for diagnosis or staging of primary Liver Cancer.
Once a diagnosis of Liver cancer is made, staging is done. This is a process to look for the spread of cancer from its place of origin to other parts of the body.
The following tests are done to complete staging.
Bone Scan
A bone scan is a special scan looking for spread of cancer into the bones. With primary liver cancer, there is a risk of spread of cancer into the bones and hence a bone scan is considered to complete the staging process.
Biopsy
A biopsy of the mass in the liver is sometimes needed to confirm the diagnosis of liver cancer. Generally, if the findings of a triple phase CT or MRI scan is consistent with a primary liver cancer and the AFP is raised, then a biopsy is not usually needed before a definitive treatment option is given. However, a biopsy is recommended when the diagnosis is in doubt on the basis of the scan.
Cancer is given a stage based on the TNM staging system or the number staging system. TNM stands for tumour, node and metastases. Based on these characteristics a score is given for each one. The number staging system is from 1-4 and is listed below for liver cancer.
Stage 1
Stage 1 involves disease when there is a single tumour up to 2cm in size or more than 2cm in size without vascular invasion. There is no involvement of lymph nodes with the cancer or no spread to other parts of the body.
Stage 2
In stage 2 the tumour is either more than 2cm with vascular invasion or multiple tumours none more than 5cm in size. There is no involvement of lymph nodes with the cancer or no spread to other parts of the body.
Stage 3
In stage 3 disease, there are either multiple tumours with at least one of which is more than 5cm or any tumour involving a major branch of the hepatic or portal vein or involvement of major organs other than the gall bladder. There is no involvement of lymph nodes with the cancer or no spread to other parts of the body.
Stage 4
In stage 4 disease, the tumour can be of any size or number, but there is either involvement of lymph nodes or spread to distant areas in the body.
Treatment of liver cancer depends on the stage of the cancer at diagnosis and the location of the cancer in the liver and other parts of the body and the age and fitness of the patient.
There are various options of treatment for primary liver cancer and these include,
- Surgical removal of cancer(resection),
- Transplantation of Liver
- Biological therapy with drugs
- Radiofrequency ablation
- Chemoembolization
- Chemotherapy
- Radiotherapy
Surgical Resection (Partial Hepatectomy, Lobectomy)
Liver resection is an option of treatment for early primary liver cancer. This operation involves removal of a part of the liver or one lobe of the liver that contains the cancer. Generally, patients eligible for this type of resection have limited disease in the liver with good liver function so that the remaining liver after the resection is able to maintain normal functions of the liver. Patients who have large tumours or multiple tumours or tumours involving large blood vessels are not suitable for having this type of treatment.
Liver Transplantation
In patients with primary liver cancer who have poor liver function due to an underlying liver condition such as cirrhosis, liver transplantation is the treatment of choice for treating the cancer as well as the cirrhosis.
The commonest type of liver transplant is an orthotopic liver transplant (OLT). Here, the patient’s liver is removed and an entire liver from a recently deceased person is transplanted into the patient. Not all patients with cirrhosis and liver cancer benefit from a liver transplant. Patients need to have 1 tumour up to 5cm or up to 5 tumours, each one not more than 3cm in size and without involvement of large blood vessels in the liver and no evidence of disease outside the liver.
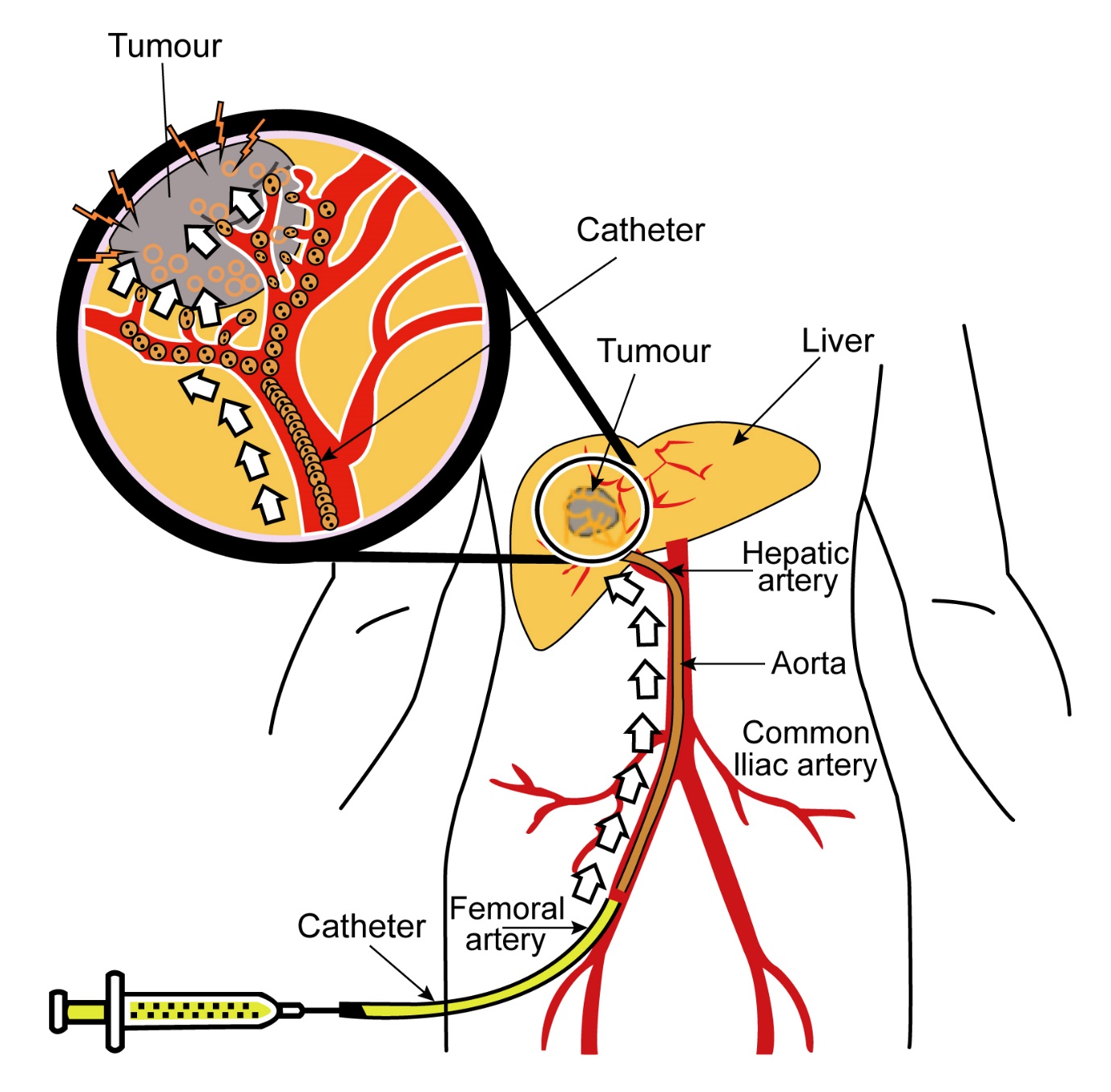
In some situations, if the tumours in the liver are too big, another procedure such as chemoembolization or radiofrequency ablation is done first and transplant done later.
Following an orthotopic liver transplant, all patients need to go on medications called Immunosuppressive drugs. As the transplanted liver is from another person, the body tries to reject the transplant. The rejection can be acute or chronic. Acute rejection can occur a few days after the transplant and chronic rejection may happen even after a few months. This rejection is stopped by using these drugs. The drugs commonly used for this are steroids, Tacrolimus, Mycophenolate Mofetil, Cyclosporine and others. Patients on immunosuppressive drugs have a higher risk of infection especially in the first few months when the immunosuppression is more.
Radiofrequency Ablation (RFA)
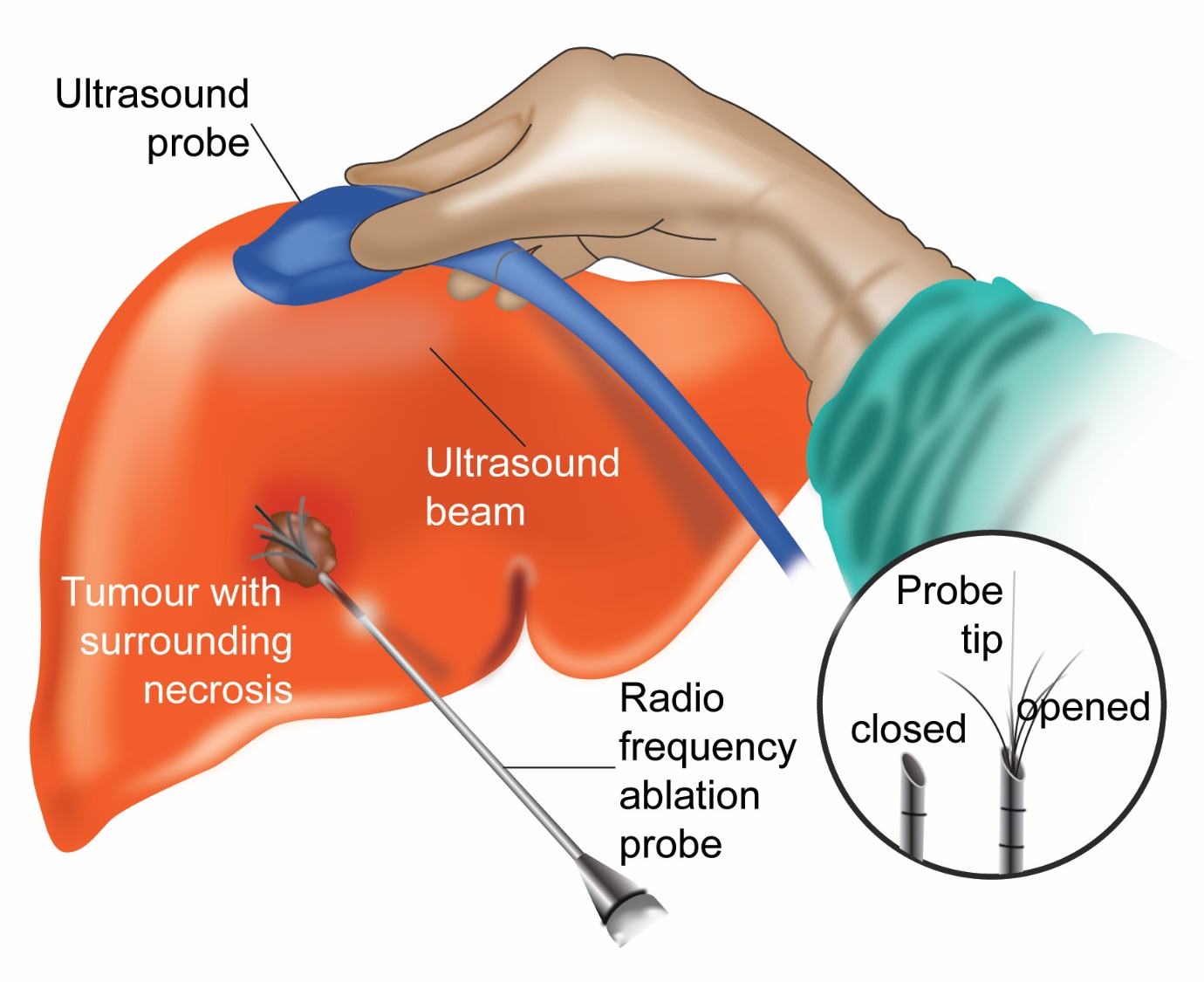
This is a procedure which involves placing a needle(probe) into the tumour through the skin and passing a current through it. This current generates heat within the tumour and destroys it. RFA is done while the patient has a general anaesthetic. It is usually done in tumours which are 4cm or smaller in size. The treatment can be used as a bridge while the patient is waiting for a liver transplant. It is also used as a treatment option in patients who are not suitable for surgery.
Transarterial Chemoembolisation (TACE)
This is a procedure where a chemotherapy drug mixed with a chemical called lipiodol is injected into the hepatic artery that feeds the tumour. This treatment helps embolise (block off) blood supply to the tumour as well as delivering chemotherapy to the tumour directly. This helps in shrinkage of the cancer. TACE is used as a treatment option in patients whose liver cancer is not operable or too large to be operable. It can also be used as a bridging treatment while the patient is waiting for a liver transplant. Not all patients will benefit from this technique and certain criteria need to be met for the patient to benefit.
Transarterial Radioembolisation (TARE)
This is a procedure similar to TACE but where Yttrium 90 labelled microspheres are injected to the area of the cancer. Yttrium-90 is a radioactive substance which releases local radiation, helping to kill of cancer cells. This treatment is considered where the liver cancer is confined to the liver without any disease outside the liver.
Percutaneous Ethanol Injection
This is a procedure where Ethanol(alcohol) is injected through the skin into the liver. The Ethanol kills the cancer cells.
Radiotherapy
Radiotherapy is sometimes used to treat liver cancers. Newer treatment techniques such as stereotactic body radiotherapy (SBRT), are used to deliver a high and precise dose of radiotherapy to the tumour. These techniques allow primary liver cancers to be treated with radiotherapy and is being used more often now.
Molecularly targeted Therapy
Sorafenib
This drug is approved for treatment of advanced or metastatic primary liver cancer that is not amenable for resection. This drug is given in the form of tablets and has shown to improve survival in patients with this condition. Sorafenib is a type of drug called a Tyrosine kinase inhibitor (TKI) and a VEGF inhibitor. It blocks chemical signals emitted in the cancer to help it grow and also stops the development of new blood vessels in the cancer. This drug is not given in patients with very abnormal liver function.
Common side effects associated with this drug include diarrhoea, sore mouth, soreness of hands and feet, tiredness, high blood pressure, bleeding and thinning of hair.
Once sorafenib is started, it is given for as long as the treatment works and the patient is tolerating the treatment well.
Lenvatinib
This drug which also has antiangiogenic properties as Sorafenib can be used as first line treatment for liver cancer that cannot be operated on. It can be used in place of Sorafenib.
Regorafenib
This is another molecular agent approved for use in liver cancer in patients who have already used Sorafenib.
Cabozantinib
Molecular agent that can be used after prior treatment with Sorafenib
Immunotherapy
Immunotherapy is the use of drugs that alter the immune mechanism in the body to enable the body’s immune system to control the cancer. Newer class of immunotherapy drugs called checkpoint inhibitors are now used in a number of cancers including primary liver cancers.
Nivolumab
Nivolumab is a monoclonal antibody against PD-1 receptor. Nivolumab blocks the PD-1 receptor and enables the T cells in the body to attack the cancer. This drug is used in liver cancer after failure of initial therapy such as Sorafenib or Lenvatinib.
Pembrolizumab
Pembrolizumab is a monoclonal antibody against PD-1 receptor. It blcoks the PD-1 receptor and enables the immune system’s T cells to attack and kill the cancer cells.
Side effects of Immune Checkpoint Inhibitors
Generally, immune checkpoint inhibitors are better tolerated by patients than chemotherapy. However, they are associated with side effects, some of which can be serious.
Chemotherapy
Chemotherapy is used to a small extent in the treatment of primary liver cancer. The response of liver cancer to chemotherapy is low and hence it is not used that commonly. Chemotherapy is considered when patients have very advanced or metastatic disease and have used Sorafenib or other drugs listed above before or are not able to use Sorafenib. Chemotherapy can be given either as single drugs or as a combination of drugs depending on the fitness of the patient.




