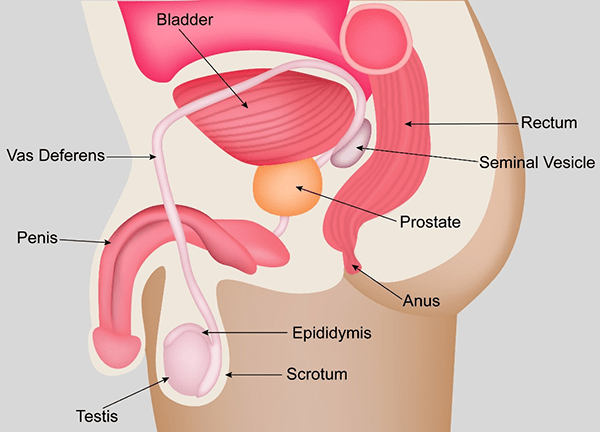
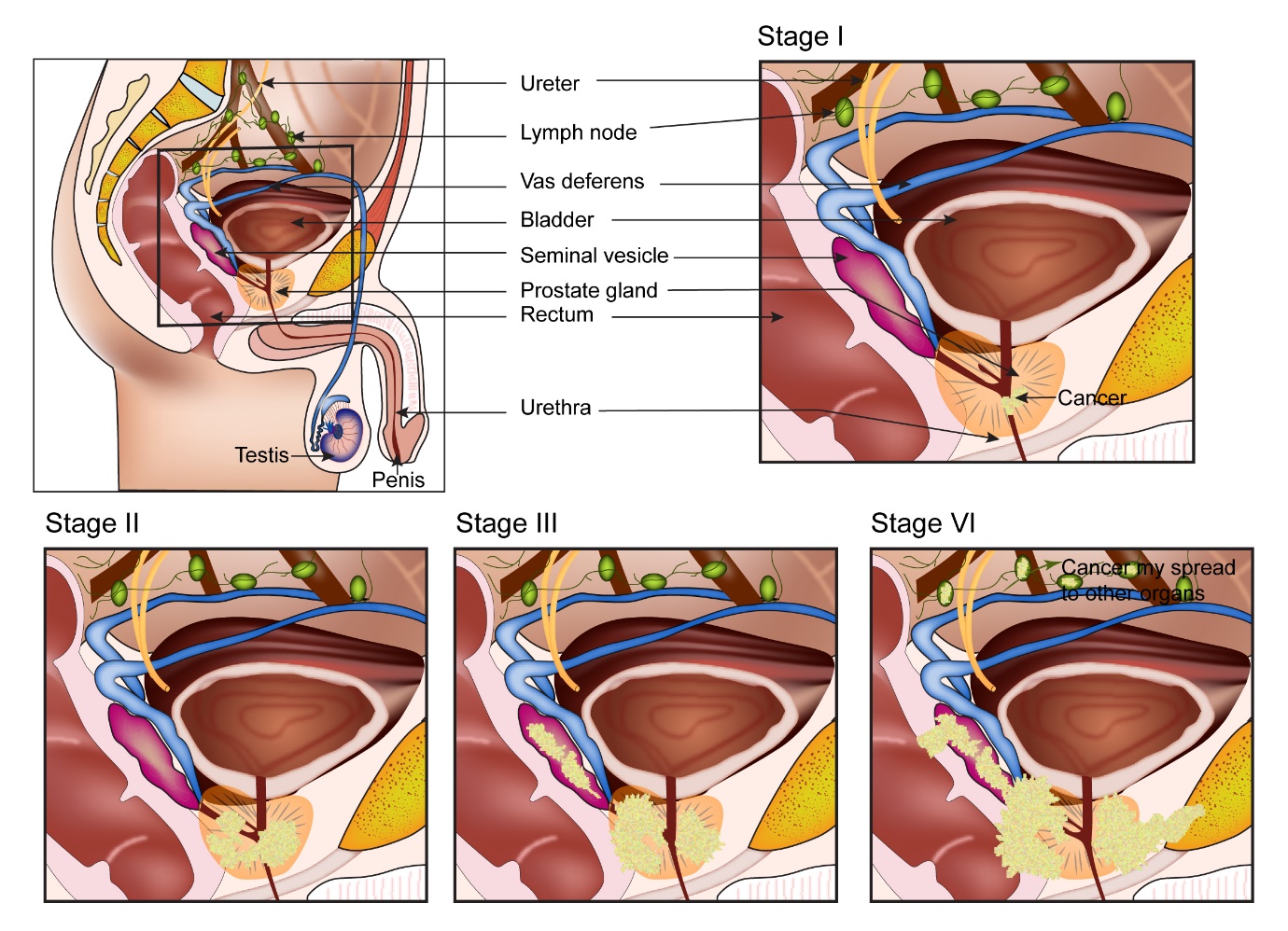
The Prostate is a male reproductive gland present in the lower part of the tummy called the pelvis. It is present in front of the rectum (lower part of large intestine) and below the urinary bladder. It encircles the upper part of the urethra and is roughly the size of a walnut. The prostate gland produces thick, white fluid which mixes with the sperm to make up semen. The prostate gland can normally increase in size with age. It produces a protein called Prostate specific antigen (PSA).
The prostate gland normally enlarges with increasing age and produces urinary symptoms associated with this enlargement. This is called as benign prostatic hyperplasia (BPH). With this increase in size it causes difficulty with passing urine as it squeezes on the urethra it encircles.
Prostate cancer is cancer that starts in the prostate when some of the prostate gland cells grow out of control. The cancer is usually an adenocarcinoma and rarely can be of other types such as small cell carcinoma of lymphoma.
According to Globocan data 2018, there were 25,696 new prostate cancers in India in 2018, making up 2.2% of all cancers.
The risk factors associated with prostate cancer include
Age
Prostate cancer is generally a cancer that manifests in the elderly age group. The risk of getting the cancer increases with age.
Genetic
About 5-10% of all prostate cancer are genetically linked, which means the cancer occurs due to inheritance of faulty genes in families.
Diet
A diet low in vegetables and fruit and high in animal fats may be a risk factor for prostate cancer.
Prostate cancer does not produce any symptoms in the early stages. When the prostate gland increases in size with age, it can produce some urinary symptoms which are commonly seen. This enlargement of the gland with age is called as benign prostatic hyperplasia (BPH).The symptoms produced by a prostate cancer can be very similar to that of BPH. These symptoms are
- Difficulty passing urine
- Going to the toilet to pass urine more often during day or night
- Feeling of incomplete emptying of bladder after passing urine
- Pain or burning sensation when passing urine
- Passing of blood in the urine
- Feeling the need to pass urine urgently
- Poor flow of urine while passing
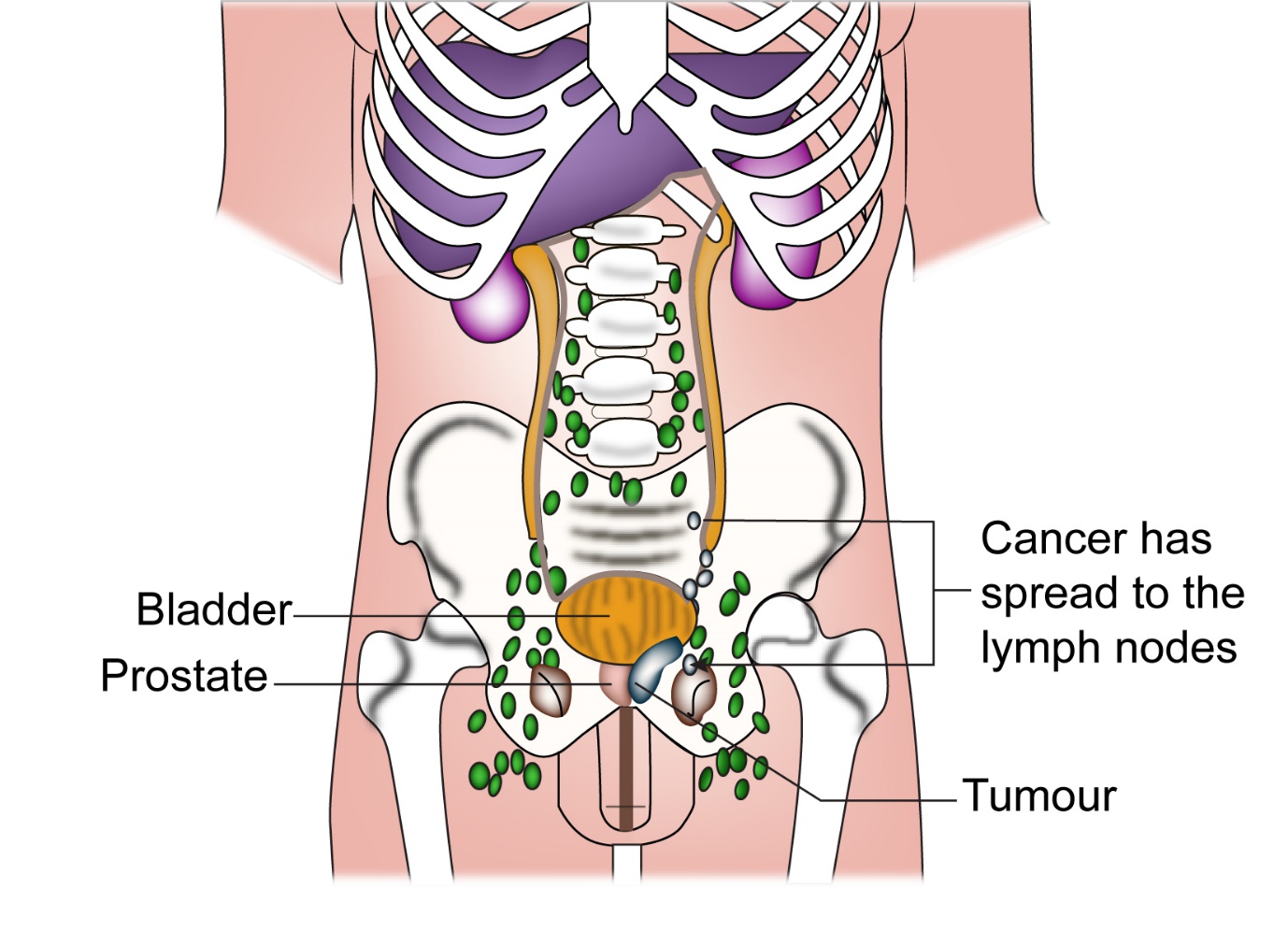
Other symptoms such as pain in other parts of the body particularly in the spine, and the areas of the hips can be seen in patients where prostate cancer has spread to the bones. Swelling of feet and legs are also sen in advanced prostate cancer.
If you have any of the above symptoms, it is important that you have them checked by your doctor.
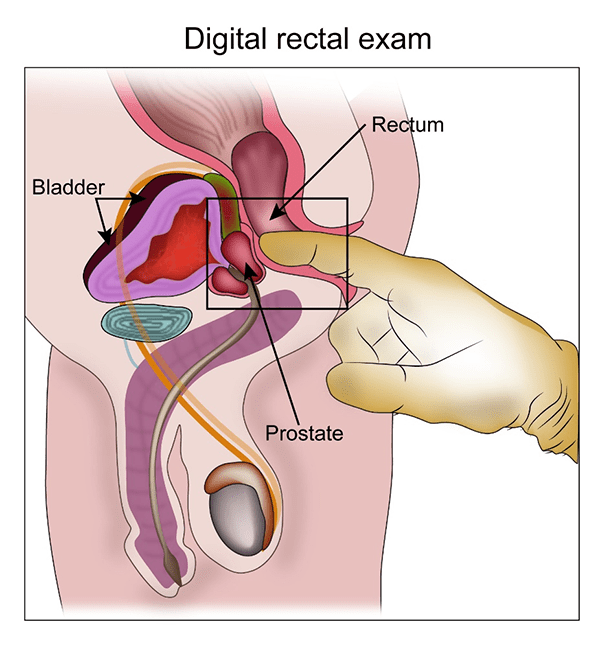
Rectal Examination
Once symptoms are present which raise the suspicion of prostate cancer, the doctor will do an examination to check for an enlarged prostate. To do that, the doctor places his finger in the rectum and will be able to tell whether the prostate is enlarged or not and whether the enlargement is possibly cancer or not.
Also, a blood test for PSA is done which will give additional information about the prostate.
PSA
A PSA test may show a normal PSA level or an elevated level. The PSA level increases slightly with age and a raised PSA doesn’t always mean presence of cancer. If the PSA is very much elevated, the chances of there being cancer is higher. Sometimes, an infection in the prostate gland can also elevate the PSA.
MRI Scan
If a PSA is abnormal or there is suspicion of Prostate cancer on examination, an MRI scan of the pelvis is done to look for changes consistent with prostate cancer. The scan helps in identifying areas of cancer on the prostate and guides the person doing the biopsy later to target the right areas. This scan is known as multiparametric MRI.
Biopsy
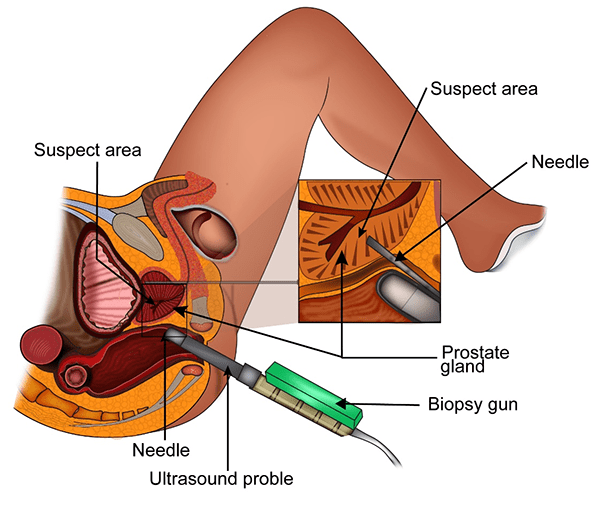
If there is a suspicion of Prostate cancer on examination and/or PSA and MRI, a biopsy is done of the prostate gland. This is usually done through the rectum with the help of an ultrasound scan and is called a trans rectal biopsy of the prostate. (TRUS biopsy)
Following the biopsy, some people may notice mild discomfort, blood in the urine or semen.
Biopsy Result
A few days after the biopsy, the result will be available which may confirm the presence of Prostate cancer. If prostate cancer is found, it is given a grade called Gleason grade. This grade is from 6 to 10 with 6 being less aggressive and 10 being most aggressive. This score of 6 to 10 is given as a sum of two numbers, for example gleason 10 is 5+5 and so on.
Based on the grade, the cancer can be classified as low grade (Gleason 6), intermediate grade (Gleason 7) and high grade (Gleason 8-10).
Once a prostate cancer is diagnosed, the following investigations can be done.
MRI Scan
An MRI of the prostate and pelvis is done if it was not done prior to the biopsy. MRI gives very good detail of the prostate gland and its surroundings and helps with staging the cancer.
Isotope Bone Scan
An isotope bone scan is done to look for the presence of cancer in the bones. A radio isotope called Technitium99 is injected into the vein prior to the scan. The scan is reported as positive if cancer is detected in the bones. Prostate cancer is one of the cancers than spreads to the bones. But the risk of spread to the bones is dependent on the nature of the cancer. Bone scan is advised in intermediate and high risk cancers but is not needed in low risk cancer. Another type of bone scan called F18 bone scan is also done. F18 bone scan is said to be more sensitive and is better in finding spread of cancer into the bones. Either of these scans is good for staging purposes.
CT scan
A CT scan is done in instances when an MRI is not available or when it is needed to assess the other parts of the body as part of staging particularly in high risk prostate cancer. CT scan uses x-rays to get detailed images of the body.
PET CT
PET CT scan is not routinely recommended for staging of prostate cancer as uptake of the radioactive tracer used in standard PET CT (18 FDG) is not consistently taken up by the cancer cells. Newer PET CT tracers such as 18 F-Choline PET or PSMA PET are said to be more useful in this setting.
The stage of a cancer is a term used to describe the size and location of the cancer in the body.
Knowing the stage of the cancer helps the doctors to decide on the most appropriate treatment. Prostate cancer is staged based on the TNM staging system or the number system.
Staging with either system is based on the extent of the tumour in the prostate, the spread of the cancer locally in the prostate and into the lymph nodes and spread of cancer into other parts of the body.
TNM Staging
T staging
| T1 | The tumour is neither felt on examination nor visible on scan |
| T1a | Tumour is an incidental finding in less than 5% of tissue removed |
| T1b | Tumour is an incidental finding in more than 5% of tissue removed |
| T1c | Tumour seen on biopsy (biopsy done as PSA high) |
| T2 | Tumour confined to within the prostate gland |
| T2a | Tumour involves one half of one lobe of prostate or less |
| T2b | Tumour involves more than half of one lobe |
| T2c | Tumour involves more than one lobe of prostate |
| T3 | Tumour extends outside the prostate capsule |
| T3a | Tumour reaches outside the capsule |
| T3b | Tumour involves seminal vesicles |
| T4 | Tumour invades other structures or is fixed |
N Staging
| Nx | Lymph nodes were not assessed |
| N0 | No involvement of lymph nodes |
| N1 | Involvement of lymph nodes with cancer |
M Staging
| M0 | No metastatic disease |
| M1 | Metastatic disease present |
Number staging
| I | T1a-c | N0 | M0 | |
| T2a | N0 | M0 | ||
| T1-2a | N0 | M0 | ||
| IIA | T1a-c | N0 | M0 | |
| T1a-c | N0 | M0 | ||
| T2a | N0 | M0 | ||
| T2a | N0 | M0 | ||
| T2b | N0 | M0 | ||
| T2b | N0 | M0 | ||
| IIB | T2 | N0 | M0 | |
| T1-2 | N0 | M0 | ||
| T1-2 | N0 | M0 | ||
| III | T3a-b | N0 | M0 | |
| IV | T4 | N0 | M0 | |
| Any T | N1 | M0 | ||
| Any T | Any N | M1 |
Prognostic Groups
Prostate cancer can also be grouped in to low, intermediate and high risk cancers depending on the T stage, N stage, Gleason score and PSA levels. Here is a limited version of the different groups. Treatment decisions are based on these risk categories.
Low Risk
- PSA less than or equal to 10
- T1-T2a
- Gleason 6
Intermediate Risk
- PSA 10-20
- T2a-T2b
- Gleason 7
High Risk
- PSA more than 20
- T2c or more
- Gleason 8-10
Treatment of Prostate cancer depends very much on the stage of cancer at diagnosis and whether the cancer is low, intermediate, high risk or metastatic.
Listed below are options of treatment for each category.
Treatment of Low risk Prostate Cancer
Low risk prostate cancer is one where the risk of spread of cancer to other parts of the body is low and the cancer is less aggressive when compared to other groups. Low risk prostate cancer is in patients with a PSA less than 10, Gleason score of 6 and T1 stage. The various options of treatment are
Active surveillance
This is an option in some patients where the risk of cancer increasing or spreading is very low. Here treatment of any form is not given, and patient is actively monitored until a time comes when the disease shows signs of increasing. Large studies have shown that there will be a group of patients with prostate cancer whose cancer will not increase over a number of years and they can continue to be on active surveillance over that time. Curative treatment can be offered at a time when there is a sign that the cancer is increasing. This is a treatment option that can be discussed with your Oncologist as not all people will be suitable for it.
Radical Prostatectomy
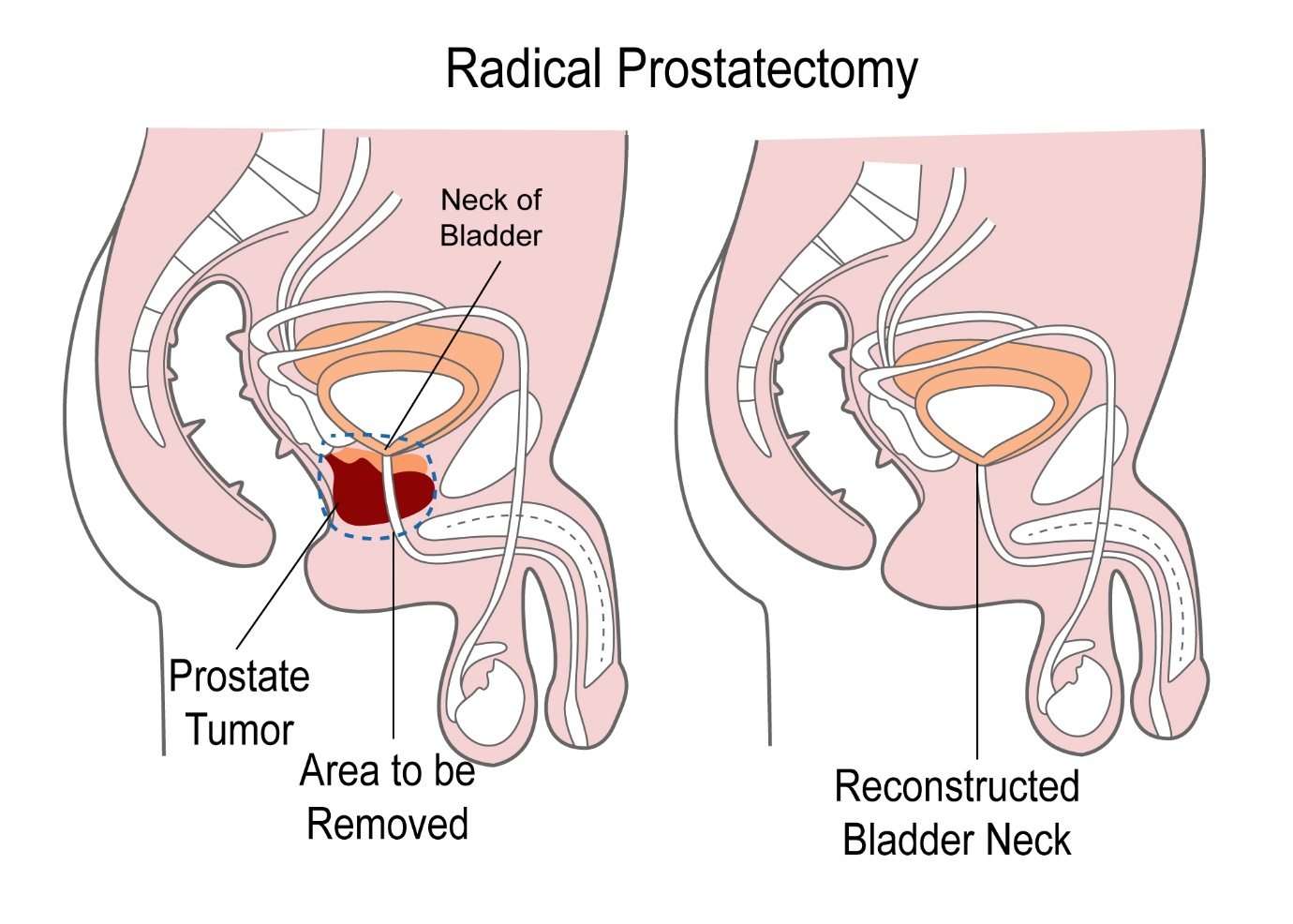
This is a surgical option of treatment of prostate cancer. Here the prostate along with lymph nodes in the pelvis are removed to cure the cancer. This operation can be done by an open method or laparoscopic method or robotic method. The laparoscopic or robotic method are less invasive, and patients recover more quickly.
In open prostatectomy, the surgeon makes an incision in the lower part of the abdomen. This is called retropubic prostatectomy. The other option(perineal) some surgeons use is to make an incision between testes are the anus. The prostate gland is removed along with the lymph nodes of the pelvis as well as the seminal vesicles which are present behind the prostate.
In the laparoscopic operation, the surgeon uses a tube with a light source which is connected to a camera and this helps to surgeon to look inside of the tummy. A small cut is made in the abdomen to insert this tube. Other cuts are made in other parts of the abdomen to insert surgical instruments. The prostate and other tissues are removed is on the above procedure.
This method is known to reduce bleeding as well as to reduce hospital stay and has similar outcomes as compared to standard surgery.
The robotic method involves use of the da vinci system. This is another form of laparoscopic surgery where the surgeon uses the help of a robot. This is a machine which has 4 arms. One arm holds the camera and the other 3 arms hold the surgical instruments. The surgeon sits at a separate console from where the operation is done. This method has been shown to be at least as effective as the laparoscopic operation if not better.
Like all treatments, radical prostatectomy has side effects. These can be in the form of impotence, leakage of urine (incontinence). In early prostate cancer, a nerve sparing prostatectomy can be done which reduces the risk of impotence after surgery.
Radiotherapy
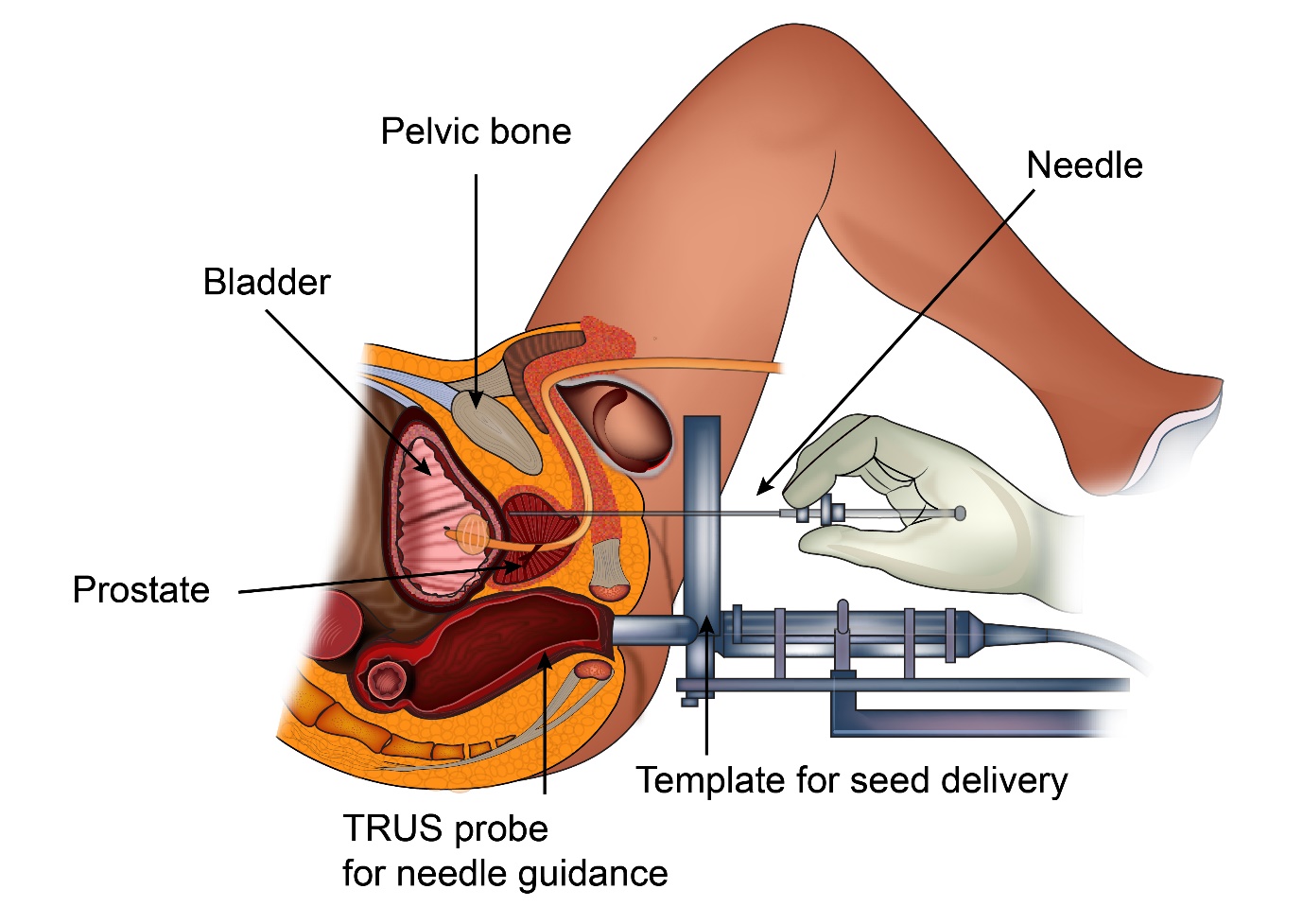
Radiotherapy is another curative treatment option in this group of patients. In radiotherapy, there are two main ways of giving the radiotherapy.
External beam radiotherapy is an option where radiotherapy is given with a machine that is outside (like an x-ray machine) and delivers high energy x-rays to the prostate.
The other option is Brachytherapy where radioactive sources are inserted into the prostate, where these sources deliver the radiation. Not all patients are suitable to have brachytherapy as a mode of treatment. Patients who will not be suitable for this approach include those with a large prostate and those with a lot of urinary symptoms among other things. Sometimes, a combination of external beam radiotherapy and brachytherapy is used. Below is a picture of how brachytherapy is given.
In external beam radiotherapy, various techniques of delivering the radiotherapy exist.
3D conformal radiotherapy is a method where a CT scan is used to plan the treatment and the treatment is shaped to fit the shape of the prostate. This is an old technique and is the minimum standard of care in treating this condition.
Intensity modulated radiotherapy or IMRT is a more specialised method than 3D conformal treatment in that the area that is being treated with radiation can be shaped even more accurately than the above method. This helps in reducing the side effects and also to give a higher dose of radiation to the target.
Rapid Arc or VMAT is a specialised form of intensity modulated radiotherapy where the treatment is given in the form of an arc and can be more accurate with less toxicity as compared to standard intensity modulated radiotherapy.
Cyberknife is also a form of intensity modulated radiotherapy which is given with a type of machine called CyberKnife. This machine delivers external beam radiotherapy similar to Rapid Arc or VMAT but the differences lie with CyberKnife being a completely different type of radiotherapy machine using different methods of delivering radiotherapy and is known to be as accurate as the above treatments. Proton beam radiotherapy which uses protons to deliver radiotherapy is also used to treat prostate cancer.
When external beam radiotherapy is used for prostate cancer, the standard treatment last for about seven and a half weeks. New treatment techniques give the same radiotherapy over 4 weeks and if Stereotactic Radiotherapy (SBRT) is used for early prostate cancer, it is over 2 weeks.
Side effects of prostate radiotherapy include mild tiredness, urinary symptoms in the form of burning sensation, increased frequency of urination during the day and night, urgency of urination, loose motions, passing of mucus and increased frequency of passing motions, bleeding when passing motions, worsening of piles when present. These effects will be at their maximum after completion of treatment and will usually resolve a few weeks after treatment. Some long term side effects of radiotherapy are also possible. These are related to the urinary and bowel symptoms and the risk of getting them is under 10%. Impotence after radiotherapy is also a side effect of treatment.
Hormone Treatment or Orchidectomy
In a small group of patients with low-risk prostate cancer who are not suitable for either surgery or radiotherapy, may benefit from having hormone treatment with tablets or injections. There is also an option of having an orchidectomy (removal of testes) instead of using hormonal medications. Either of these options will help control prostate cancer.
Treatment of intermediate risk prostate cancer
Patients with intermediate risk prostate cancer are those with a PSA between 10-20, or Gleason score 7, stage IIa-IIb. The options of treatment for patients in this group include radical prostatectomy, radiotherapy, and hormones. Active surveillance is usually not an option in this set of patients.
In patients with intermediate risk prostate cancer choosing to have radiotherapy, hormones in the form of LHRH analogues are given for 2-3 months prior to, and during radiotherapy. This helps in achieving better control on the prostate cancer. The option of having hormones is not recommended for patients going for prostatectomy as a benefit has not been shown.
In patients who are not fit for either surgery or radiotherapy, hormones alone can be an option of treatment.
Treatment of high risk prostate cancer
Prostate cancer is said to be a high risk when the PSA is greater than 20, or the Gleason score is 8 or more, or it is stage TIIc or more.
When the disease is said to be confined to the prostate gland, radical prostatectomy is still an option of treatment. However when disease is found to be extending outside the prostate gland, radiotherapy is usually the main option of treatment. Hormonal treatment is used along with radiotherapy. It is given for 3 months prior to radiotherapy, during radiotherapy and for up to 2-3 years in total duration.
In patients not suitable for radiotherapy, hormonal treatment is given on its own. The other option is an orchidectomy (removal of testes) which does the same job.
In patients with advanced prostate cancer, where the cancer is advanced around the prostate but has not spread to other organs in the body, chemotherapy with a drug called Docetaxel or other hormones such as Abiraterone or Enzalutamide may be added to standard hormone treatment (LHRH analogues) to get additional benefit. The decision whether to go ahead is made after discussion of pros and cons with the doctor and patient.
Metastatic prostate cancer is, when there is spread of prostate cancer to distant sites in the body. The following are the treatment options available in metastatic prostate cancer.
Once, metastatic prostate cancer is diagnosed, treatment options are mainly able to control the disease.
Hormonal treatment
This form of treatment is the mainstay in management of metastatic prostate cancer. Hormones can be given as tablets or injections and are usually given from the time of diagnosis of metastatic disease. Prostate cancer tends to grow by feeding on testosterone produced in the body. The hormonal agents that are used help by either reducing the production of testosterone or blocking the effects of testosterone.
Hormonal agents such as Leuprorelin, Goserelin, Triptorelin and Degarelix are used which are given in the form of injections usually once every 1-3 months. Other agents such as Bicalutamide, Cyproterone, Enzalutamide, Abiraterone are given as tablets. Hormonal treatment works for a period of time after which the cancer can start to grow again. It is then called hormone refractory cancer. The usual time period for which the hormones work is measured in years.
Orchidectomy, which is removal of both the testes is as good as injections with LHRH analogues in controlling Prostate cancer especially at diagnosis. It can be a cheaper option of treatment than hormone injections.
As hormone treatments stop the reduction or reduce the effect of testosterone in the body, the side effects are related to reduced testosterone levels. Common side effects include sweating, hot flushes, weight gain, increase in body fat, reduced muscle in the body, thinning or reduction in body hair. Breast enlargement can be a side effect of drugs such as Bicalutamide.
Chemotherapy
Chemotherapy is frequently used for treatment of Prostate Cancer.
Commonly used drugs in this setting are Docetaxel, Mitoxantrone, and Cabazitaxel. These agents can be given at the same time as hormonal treatment or after hormonal treatment stops working. These drugs help to reduce the prostate cancer and improve symptoms associated with cancer. They help in prolonging survival. When given, chemotherapy in prostate cancer is given once every 21 days for up to 6 months. Treatment is monitored with PSA measurements and scans to look for response to such treatment. Common side effects with these drugs include hair loss, tiredness, loose motions, risk of infection, changes in nails, tingling in hands and feet and soreness in mouth.
Radiotherapy
Radiotherapy in metastatic prostate cancer is mainly used to control the symptoms that are being produced by the cancer. These symptoms could be varied and include those such as pain and bleeding. Radiotherapy is very effective in treating pain caused by cancer present in the bones. The duration of radiotherapy in this setting is usually short ranging from 1-10 treatments. Radiotherapy lasting up to 20 treatments is used to treat the prostate in patients who have limited disease in the bones.
Other treatments
Other treatments that are used in metastatic prostate cancer include Steroids, Oestrogen and Progesterone. Radioactive sources such as Strontium-89 and Radium 223 are used for treatment of bone metastases.
Drugs called bisphosphonates and Denosumab are used to strengthen the bones in patients with disease in the bones. Strengthening the bones reduces symptoms from bone metastases such as pain and risk of fractures. These drugs are given every 3-4 weeks.
Monitoring of disease in metastatic prostate cancer is usually done with the help of serial PSAs and scans. The scans used are CT scans, isotope bone scans. PET CT scans are usually not recommended for regular monitoring of metastatic disease but newer types of PET-CT such as PSMA PET or Choline PET may be useful.




