Radiotherapy FAQ’s
What is Radiotherapy?

Radiotherapy is the use of high energy x-rays given to kill cancer cells. These x-rays cause damage to the DNA of the cancer cells and thereby kill them. Radiotherapy is a local treatment and has its effect in the area that it is given to. Radiotherapy is of different types. The standard form of radiotherapy is delivered through a machine called a linear accelerator as shown in the picture below. This type of machine delivers two types of rays. One is high energy x-rays called photons and the other is electrons. A Cobalt-60 machine is another type of radiotherapy machine that delivers gamma rays. These machines are not as common now. A proton therapy machine also is a radiotherapy machine but delivers protons which are used to treat cancer. All of these are called as external beam radiotherapy.
Brachytherapy is another form of radiotherapy where radioactive sources are inserted into the cavities of the body or into the cancers. These radioactive sources such as Iodine 125 (I125), Caesium 137, Iridium or others are available as seeds, pins, wires etc and are used for insertion.
Radiotherapy is given in what are called as fractions. A fraction is one radiotherapy treatment and can last for some minutes. Usually, these fractions are given once a day for 5 days a week. Sometimes, two fractions a day can be given. A course of radiotherapy may contain several fractions, with some courses lasting up to seven weeks.
How does Radiotherapy work?
The high energy x-rays produced from a standard radiotherapy machine (linear accelerator) kills cancer cells by causing damage to the DNA in these cells. The normal cells in the body can also be damaged by radiotherapy but have a better capacity to repair and recover than cancer cells. The damage of normal cells from radiotherapy is what causes the side effects of radiotherapy.
What are the types of Radiotherapy?
Radiotherapy (external beam) can be given in different ways depending on the necessity and also on the type of machine and technology available. Some techniques are better than others in treating the cancer and limiting the side effects. These are briefly described below.
3D conformal Radiotherapy
This is a way of planning and giving radiotherapy, where CT, MRI scans are used to get a three-dimensional image of the cancer. This allows the planning process to be made in three dimensions.
It allows the radiation treatment to be more precise than standard 2D radiotherapy. 3D conformal radiotherapy is usually the minimum standard of treatment these days.
Intensity modulated Radiotherapy (IMRT)
IMRT is a type of 3D conformal treatment planning and delivery method, where radiation beams can be precisely shaped to fit the shape of the tumour. This helps in minimizing side effects to surrounding normal structures in the body. The difference between IMRT and 3D conformal radiotherapy is that IMRT can target the cancer more accurately reducing side effects. Also, with IMRT, there is the possibility of delivering different doses of radiotherapy to different parts of the same tumour. IMRT is done by using multiple radiation beams directed at the tumour from different angles.
Arc based Treatment
Arc based therapy (Rapid Arc, VMAT) is delivery of radiotherapy with the linear accelerator going around the patient in an arc like fashion. This type of therapy is also IMRT but in certain situations can be more precise than standard IMRT. Arc based therapy is delivered much quicker than standard IMRT and therefore the duration of treatment each day is much shorter for the patient.
Stereotactic body Radiotherapy (SBRT) or SABR (Stereotactic Ablative Radiotherapy)
This is a newer technique of radiotherapy that is being used to treat early stage lung cancers and cancers of the liver, prostate, pancreas and others. It is also being used to treat cancers that have recurred such as in the spine or other areas. The treatment involves use of very advanced radiation planning tools and radiotherapy machines. As a result, radiotherapy delivery can be ultra-precise, enabling the oncologist to give very high doses of radiation to the tumour and at the same time minimising side effects to surrounding normal organs. The treatment duration for example in lung cancer with SBRT can be very short ranging from one to two weeks as compared to 6 to 7 weeks for standard radiotherapy.
Image guided Radiotherapy (IGRT)
Image guided radiotherapy is the use of imaging systems such as x-rays or CT scanners to monitor treatment accuracy. Normally, in standard 3D conformal radiotherapy, a CT scan is done prior to start of treatment for planning purposes. During treatment, the accuracy of treatment is verified with megavoltage x-rays done now and again. In IGRT, a CT scan or kilovoltage x-ray can be done prior to every radiotherapy treatment to ensure accuracy of the treatment. By being very accurate, the side effects of treatment are few, the target is not missed and a higher dose of radiotherapy can be delivered to kill the cancer.
Tomotherapy
Tomotherapy is external beam radiotherapy given with a specific type of machine called tomotherapy. It is not much different to a modern advanced linear accelerator. A tomotherapy machine is capable of doing IMRT and IGRT treatments.
Cyberknife
A Cyberknife machine is an external beam radiotherapy machine like a linear accelerator. This machine has the capability of doing real time tracking of the patient during treatment using x-ray monitoring. This type of tracking enables Cyberknife to treat certain cancers very accurately. Real time tracking options are available on other types of linear accelerators too. Cyberknife unlike advanced linear accelerators does not have CT based image guidance. However, the x-ray based image guidance is quite advanced and hence used for treatment of cancers such as those in the brain, spine or near the spine where x-rays can accurately image the bones. A fraction of cyberknife treatment usually takes longer than that of a good linear accelerator.
Stereotactic Radiosurgery (SRS)
This is a type of radiotherapy using high energy x-rays (linear accelerator, cyberknife, tomotherapy) or gamma rays (gamma knife machine) to treat small areas of cancer very precisely using high doses of radiotherapy. The technique allows treating certain types of cancer very well and in a short period of time. The treatment is done using a single fraction of radiotherapy. The duration of this single fraction can range from a few minutes to more than an hour. Not all cancers can be treated with this method.
Proton Therapy
Proton therapy is another form of external beam radiotherapy. Proton therapy uses protons instead of photons as in a linear accelerator. The physical properties of proton beams are different to an electron or photon beams. This enables proton beams to accurately target certain cancers that are difficult to reach without causing side effects. These are usually tumours behind the eye, those close to the spine and cancers in children. For other cancers, the benefit of proton therapy over standard radiotherapy is small.
What are the other terminologies used for Radiotherapy?
Curative radiotherapy
Here radiotherapy is given with the aim to kill off all the cancer cells and cure the cancer. Curing the cancer implies that the cancer never comes back.
Palliative Radiotherapy
Palliative radiotherapy is used in a situation when cure is not possible with any treatment option. The aim of palliative radiotherapy is to control symptoms caused from the cancer. Symptoms can include pain, bleeding, cough, obstruction, fracture of bone due to cancer etc.
What happens once decision made for Radiotherapy
Radiotherapy Planning (External beam therapy)
Once the doctor has decided to give radiotherapy and the patient consents for treatment, the radiotherapy planning process begins.
Mould room

For radiotherapy to be precise and accurate, the patient needs to be in the same position every day of treatment. This position has to be very accurate to the nearest millimetre. To achieve this, various tools are used to enable the patient to remain very still during treatment.
A thermoplastic mask is commonly used for patients having treatment involving the upper body. vacuum generated bags, foam pillows, pads, mouth bites etc are used. The exact item to be used is decided by the doctor and this is prepared in the mould room.
Radiotherapy Planning Scan
Once the mould room process is complete, the patient is taken into the scanning room and a radiotherapy planning CT or a PET-CT scan is done. This scan is done with the patient lying in the same position as he/she would do during treatment. This scan enables the doctor to define the areas to treat and is needed to do the treatment. Sometimes an MRI scan is also done in this process.
Volume Contouring
Once the planning scan is complete, the doctor will then define the area to be treated on the scan by using specialist software.
Radiotherapy Physics
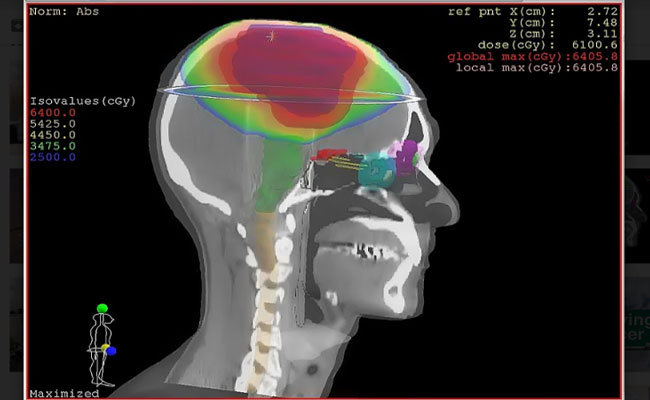
Once contouring is completed by the doctor, the radiotherapy physics team get on with the planning of the treatment. This is done with the help of very advanced radiotherapy planning systems. The aim of a good plan is to maximise the radiotherapy dose to the cancer while giving minimum dose possible to the normal structures and organs around the cancer. Once the plan is complete a quality assurance test is done to check for accuracy.
If above all goes well, treatment then commences. A minimum of 2-3 days are needed between the decision to treat with radiotherapy and the start of treatment
Side Effects of Radiotherapy
Radiotherapy can cause a variety of side effects depending on the area of the body being treated.
There are some general side effects which can happen with most radiotherapy treatments and then some specific side effects for different body areas are listed below. When talking about side effects of treatment, it should be understood that not all patients experience these side effects, and some patients may have more side effects than others for the same treatment.
General side effects
Tiredness
Begins a few days to weeks after start of treatment and settles a few weeks after completion of treatment.
Skin changes
Whichever part of the body is treated, the skin is in the line of treatment and will have some side effects. These effects are minimal for shorter treatments and more for treatments lasting many weeks. Common effects include
Dryness of skin, Itchiness of skin, Redness of skin, occasional breaking of skin, hair loss, skin discolouration, thickening of skin. Rarely oozing from the skin is seen.
Most of these skin effects will subside a few weeks after completion of treatment. Skin discolouration make take a few months to settle.
Loss of Hair
There can be loss of hair in the treated area due to radiotherapy. Usually, hair does grow back but may not grow fully if high doses of radiotherapy were used.
Other side effects which are specific to the area being treated are listed in other sections of the website.




