Treatment of Cancer
Once a cancer diagnosis is made and tests are done to get a stage for the cancer, a treatment plan is made by the treating Oncologist. In a good cancer centre or cancer department, the treatment plan is made by a multidisciplinary team or a tumour board. This tumour board consists of professionals such as Oncologists, Radiologists, Pathologists, Physicians, Nurses and other professionals. They together discuss each patient’s details and all aspects of the person’s cancer. The treatment plan for the cancer is then made jointly by the team and not an individual. A tumour board meeting may happen once a week, twice a week or even daily depending on the volume of patients in that centre.
There are various forms of treatments for a cancer. These include
- Surgery
- Radiotherapy
- Chemotherapy
- Biological therapy
- Immunotherapy
- Hormonal therapy
- Supportive Care
Other less common approaches such as Radiofrequency ablation, Cryotherapy
See the sections below that describe each of these treatments.
Surgery is used in cancer in different scenarios.
Curative surgery
The aim of curative surgery is to remove all the cancer that is seen on tests. This type of surgery enables a cure from the cancer. Curative surgery is done in early stages of cancer and in some instances when the cancer is stage 3. Curative surgery is either done alone or is combined with chemotherapy and/or radiotherapy given after the surgery. These treatments may increase the chances of cure when compared to surgery alone. Where these additional treatments are used depends on the type and stage of cancer at the time of treatment.
Non-Curative surgery (Palliative Surgery)
Here surgery is done with the intention to control symptoms and make the patient better rather than to aim to cure the patient. This type of surgery is done in patients where the cancer is so advanced that it is not possible to remove all of it or the cancer has spread to different parts of the body (stage 4) and hence not curable. Examples of this type of surgery include bypassing a blocked intestine, debulking surgery-to reduce the bulk of cancer to improve symptoms for the patient.
Potentially curative surgery
Some patients who have had curative treatments in the past may have a recurrence of their cancer in one area of the body. Treatment options are discussed and if this recurrence is isolated and operable, a potentially curative surgery is done. The aim is to maximise control of the cancer with the chance of a cure.
Diagnostic surgery
This type of surgery is done to help in the diagnosis of the cancer as well as a treatment at the same time. Normally a biopsy is first done before major surgery is undertaken, but in certain circumstances both can be done at the same time.
Preventive Surgery
Here the surgery is done prior to the patient being diagnosed with cancer. This type of surgery is applicable only to patients where there is a very high risk of getting a type of cancer. For example, removal of breasts in a BRCA gene carrier-where risk of breast cancer is high.
Restorative/Cosmetic/Reconstructive surgery
This type of surgery is commonly done in cancers of the head and neck region, breast and limb cancers. Usually these surgeries are done along with or after curative cancer surgeries. They are used to restore the function of the organ that has been operated upon or to improve the cosmetic outcome after major surgery.
What are the different methods of surgery used in Cancer?
Surgery is done in different forms to treat cancer
Open surgery
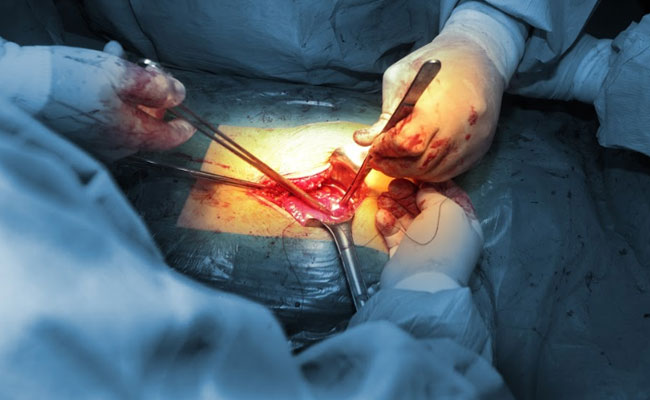
This is the standard form of surgery where a cut is made in the area to be treated and the cancer is removed through that. For example, if the cancer is in the abdomen, a large cut is made in the abdomen for the operation to take place. The advantages of this method are that it is technically easier to do and the only option in some situations. The recovery period is longer compared to other methods.
Laparoscopic surgery

This is a type of surgery where 3-4 small holes about 1-2cm in size are made and the operation is done through them. A laparoscope is an instrument with a camera and is inserted into one of the holes. The operating surgeon is able to see inside of the body (area of surgery) with this instrument. The operating instruments are inserted through the other holes. The advantage of this technique is that the scar is smaller, and healing is quicker. This technique is not suitable in all cancer surgeries. The disadvantages are that the duration of the operation can be longer than the open method and special training and skills are needed to gain expertise.
Robotic Surgery
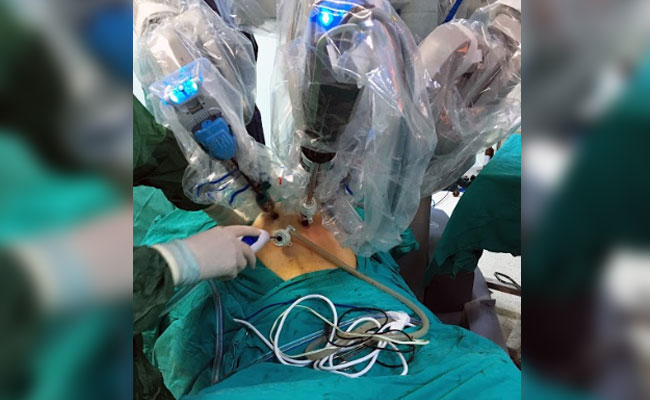
This is another form of laparoscopic surgery but with the help of robotic system which controls the instruments. Here, like laparoscopy, small holes are made in the area of surgery. The surgeon sits at a console away from the patient and uses the computer to perform the operation. Any movements made by the surgeon are transferred to the instruments through the robotic system. This method is used to treat some cancers and like laparoscopy can help in quicker recovery of patients. In some types of cancer surgery, side effects may also be less than other forms of surgery. This method though is significantly more expensive than other options.
Less common types of surgery
Less common types of surgery used to treat cancers include
Laser surgery- where lasers are used to burn out cancer cells and used to treat some early stage cancers such as cervix, anus etc.
Cryotherapy-where a probe is inserted into the cancer and the cancer cells are frozen at very cold temperatures
Radiofrequency ablation-where a probe is inserted into the cancer and high energy radio waves are passed which heat the cancer cells and kill them.
It is important to note that these techniques are used for only very limited number of cancers.
What happens after decision is made for surgery?
Once the doctor and the patient have decided for a type of surgery, the patient is made to have a set of blood tests as well as a consultation with the anaesthetic team and other specialists such as physicians or cardiologists to assess and see whether the patient is fit enough to have the operation.
What type of Anaesthesia is used during cancer surgery?
Anaesthesia is use of medications to reduce the discomfort and pain that is associated with surgery. Anaesthesia can be of many types and the common ones are listed below.
Local
Local anaesthesia is where a medicine is injected around the site where the surgery is due to take place. The medicine numbs the area so that the patient does not feel any pain during surgery. The effect of the medicine usually wears off a few minutes to hours after the surgery.
Regional
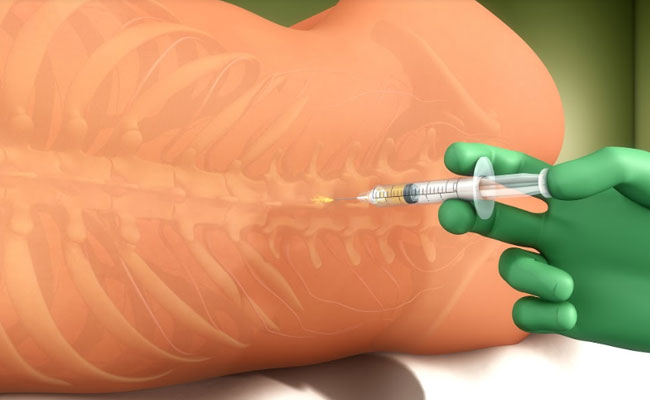
In this type of anaesthesia, medicine is given to numb a larger area than in local anaesthesia. Medications to cause mild sleepiness can also be used along with regional anaesthesia to improve comfort for the patient. This type of anaesthesia is a nerve block or spinal anaesthesia.
General
This is a type of anaesthesia where the patient is put to sleep with an injection. A tube is inserted into the windpipe to help the patient to breathe. This is the most common type of anaesthesia used for cancer surgery.
What happens following surgery?

After the surgery, the patient stays in hospital for a few days. Drains(tubes) are placed at the site of the operation to help drain any fluid that collects at the surgical site. These are removed after a few days once the fluid stops draining. Once the Patient begins to eat and is feeling better, he/she is discharged home and is seen in the outpatient clinic in about two weeks for removal of sutures or surgical clips which are placed at the time of the operation.
The surgeon will also explain to the patient in that visit about the outcome of the surgery and the histology report. This report explains in detail about the cancer and will guide as to whether further treatment is needed.
What are the potential complications of cancer surgery?
Like any surgery, cancer surgery can be associated with side effects and complications. Most of these are specific to the type of surgery that is being done but some common complications associated with surgery include
Infection
Infection is an important complication associated with any surgery. Infection can occur at the operated area or in other areas such as lungs or urinary tract. Generally, all precautions are taken prior to, during and after surgery to reduce the risk of infection.
Pain
Pain is a common side effect of surgery but can be controlled with good pain killers.
Loss of Blood
Blood is lost during surgery, is usually minimal, but sometimes a blood transfusion is needed during or after surgery.
What is Radiotherapy?

Radiotherapy is the use of high energy x-rays given to kill cancer cells. These x-rays cause damage to the DNA of the cancer cells and thereby kill them. Radiotherapy is a local treatment and has its effect in the area that it is given to. Radiotherapy is of different types. The standard form of radiotherapy is delivered through a machine called a linear accelerator as shown in the picture below. This type of machine delivers two types of rays. One is high energy x-rays called photons and the other is electrons. A Cobalt-60 machine is another type of radiotherapy machine that delivers gamma rays. These machines are not as common now. A proton therapy machine also is a radiotherapy machine but delivers protons which are used to treat cancer. All of these are called as external beam radiotherapy.
Brachytherapy is another form of radiotherapy where radioactive sources are inserted into the cavities of the body or into the cancers. These radioactive sources such as Iodine 125 (I125), Caesium 137, Iridium or others are available as seeds, pins, wires etc and are used for insertion.
Radiotherapy is given in what are called as fractions. A fraction is one radiotherapy treatment and can last for some minutes. Usually, these fractions are given once a day for 5 days a week. Sometimes, two fractions a day can be given. A course of radiotherapy may contain several fractions, with some courses lasting up to seven weeks.
How does Radiotherapy work?
The high energy x-rays produced from a standard radiotherapy machine (linear accelerator) kills cancer cells by causing damage to the DNA in these cells. The normal cells in the body can also be damaged by radiotherapy but have a better capacity to repair and recover than cancer cells. The damage of normal cells from radiotherapy is what causes the side effects of radiotherapy.
What are the types of Radiotherapy?
Radiotherapy (external beam) can be given in different ways depending on the necessity and also on the type of machine and technology available. Some techniques are better than others in treating the cancer and limiting the side effects. These are briefly described below.
3D conformal Radiotherapy
This is a way of planning and giving radiotherapy, where CT, MRI scans are used to get a three-dimensional image of the cancer. This allows the planning process to be made in three dimensions.
It allows the radiation treatment to be more precise than standard 2D radiotherapy. 3D conformal radiotherapy is usually the minimum standard of treatment these days.
Intensity modulated Radiotherapy (IMRT)
IMRT is a type of 3D conformal treatment planning and delivery method, where radiation beams can be precisely shaped to fit the shape of the tumour. This helps in minimizing side effects to surrounding normal structures in the body. The difference between IMRT and 3D conformal radiotherapy is that IMRT can target the cancer more accurately reducing side effects. Also, with IMRT, there is the possibility of delivering different doses of radiotherapy to different parts of the same tumour. IMRT is done by using multiple radiation beams directed at the tumour from different angles.
Arc based Treatment
Arc based therapy (Rapid Arc, VMAT) is delivery of radiotherapy with the linear accelerator going around the patient in an arc like fashion. This type of therapy is also IMRT but in certain situations can be more precise than standard IMRT. Arc based therapy is delivered much quicker than standard IMRT and therefore the duration of treatment each day is much shorter for the patient.
Stereotactic body Radiotherapy (SBRT) or SABR (Stereotactic Ablative Radiotherapy)
This is a newer technique of radiotherapy that is being used to treat early stage lung cancers and cancers of the liver, prostate, pancreas and others. It is also being used to treat cancers that have recurred such as in the spine or other areas. The treatment involves use of very advanced radiation planning tools and radiotherapy machines. As a result, radiotherapy delivery can be ultra-precise, enabling the oncologist to give very high doses of radiation to the tumour and at the same time minimising side effects to surrounding normal organs. The treatment duration for example in lung cancer with SBRT can be very short ranging from one to two weeks as compared to 6 to 7 weeks for standard radiotherapy.
Image guided Radiotherapy (IGRT)
Image guided radiotherapy is the use of imaging systems such as x-rays or CT scanners to monitor treatment accuracy. Normally, in standard 3D conformal radiotherapy, a CT scan is done prior to start of treatment for planning purposes. During treatment, the accuracy of treatment is verified with megavoltage x-rays done now and again. In IGRT, a CT scan or kilovoltage x-ray can be done prior to every radiotherapy treatment to ensure accuracy of the treatment. By being very accurate, the side effects of treatment are few, the target is not missed and a higher dose of radiotherapy can be delivered to kill the cancer.
Tomotherapy
Tomotherapy is external beam radiotherapy given with a specific type of machine called tomotherapy. It is not much different to a modern advanced linear accelerator. A tomotherapy machine is capable of doing IMRT and IGRT treatments.
Cyberknife
A Cyberknife machine is an external beam radiotherapy machine like a linear accelerator. This machine has the capability of doing real time tracking of the patient during treatment using x-ray monitoring. This type of tracking enables Cyberknife to treat certain cancers very accurately. Real time tracking options are available on other types of linear accelerators too. Cyberknife unlike advanced linear accelerators does not have CT based image guidance. However, the x-ray based image guidance is quite advanced and hence used for treatment of cancers such as those in the brain, spine or near the spine where x-rays can accurately image the bones. A fraction of cyberknife treatment usually takes longer than that of a good linear accelerator.
Stereotactic Radiosurgery (SRS)
This is a type of radiotherapy using high energy x-rays (linear accelerator, cyberknife, tomotherapy) or gamma rays (gamma knife machine) to treat small areas of cancer very precisely using high doses of radiotherapy. The technique allows treating certain types of cancer very well and in a short period of time. The treatment is done using a single fraction of radiotherapy. The duration of this single fraction can range from a few minutes to more than an hour. Not all cancers can be treated with this method.
Proton Therapy
Proton therapy is another form of external beam radiotherapy. Proton therapy uses protons instead of photons as in a linear accelerator. The physical properties of proton beams are different to an electron or photon beams. This enables proton beams to accurately target certain cancers that are difficult to reach without causing side effects. These are usually tumours behind the eye, those close to the spine and cancers in children. For other cancers, the benefit of proton therapy over standard radiotherapy is small.
What are the other terminologies used for Radiotherapy?
Curative radiotherapy
Here radiotherapy is given with the aim to kill off all the cancer cells and cure the cancer. Curing the cancer implies that the cancer never comes back.
Palliative Radiotherapy
Palliative radiotherapy is used in a situation when cure is not possible with any treatment option. The aim of palliative radiotherapy is to control symptoms caused from the cancer. Symptoms can include pain, bleeding, cough, obstruction, fracture of bone due to cancer etc.
What happens once decision made for Radiotherapy
Radiotherapy Planning (External beam therapy)
Once the doctor has decided to give radiotherapy and the patient consents for treatment, the radiotherapy planning process begins.
Mould room

For radiotherapy to be precise and accurate, the patient needs to be in the same position every day of treatment. This position has to be very accurate to the nearest millimetre. To achieve this, various tools are used to enable the patient to remain very still during treatment.
A thermoplastic mask is commonly used for patients having treatment involving the upper body. vacuum generated bags, foam pillows, pads, mouth bites etc are used. The exact item to be used is decided by the doctor and this is prepared in the mould room.
Radiotherapy Planning Scan
Once the mould room process is complete, the patient is taken into the scanning room and a radiotherapy planning CT or a PET-CT scan is done. This scan is done with the patient lying in the same position as he/she would do during treatment. This scan enables the doctor to define the areas to treat and is needed to do the treatment. Sometimes an MRI scan is also done in this process.
Volume Contouring
Once the planning scan is complete, the doctor will then define the area to be treated on the scan by using specialist software.
Radiotherapy Physics
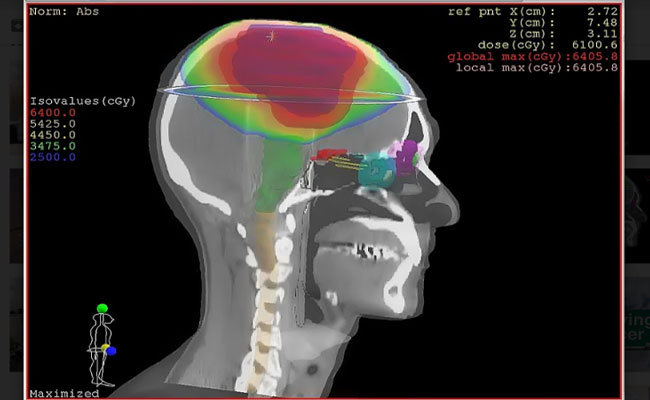
Once contouring is completed by the doctor, the radiotherapy physics team get on with the planning of the treatment. This is done with the help of very advanced radiotherapy planning systems. The aim of a good plan is to maximise the radiotherapy dose to the cancer while giving minimum dose possible to the normal structures and organs around the cancer. Once the plan is complete a quality assurance test is done to check for accuracy.
If above all goes well, treatment then commences. A minimum of 2-3 days are needed between the decision to treat with radiotherapy and the start of treatment
Side Effects of Radiotherapy
Radiotherapy can cause a variety of side effects depending on the area of the body being treated.
There are some general side effects which can happen with most radiotherapy treatments and then some specific side effects for different body areas are listed below. When talking about side effects of treatment, it should be understood that not all patients experience these side effects, and some patients may have more side effects than others for the same treatment.
General side effects
Tiredness
Begins a few days to weeks after start of treatment and settles a few weeks after completion of treatment.
Skin changes
Whichever part of the body is treated, the skin is in the line of treatment and will have some side effects. These effects are minimal for shorter treatments and more for treatments lasting many weeks. Common effects include
Dryness of skin, Itchiness of skin, Redness of skin, occasional breaking of skin, hair loss, skin discolouration, thickening of skin. Rarely oozing from the skin is seen.
Most of these skin effects will subside a few weeks after completion of treatment. Skin discolouration make take a few months to settle.
Loss of Hair
There can be loss of hair in the treated area due to radiotherapy. Usually, hair does grow back but may not grow fully if high doses of radiotherapy were used.
Other side effects which are specific to the area being treated are listed in other sections of the website.
What is Chemotherapy?

Chemotherapy is the use of drugs in the form of tablets, injections and drips to treat Cancer. These drugs are given as single agents or combinations of them.
How does Chemotherapy work?
Different Chemotherapy drugs have different ways of killing Cancer cells. For example, some drugs damage the cell wall, others stop the growth of cells and some others cause death of the cell by damaging the DNA.
How often is Chemotherapy given?
Chemotherapy is given in cycles. A typical cycle lasts three weeks but can be every week or every two or four weeks. Usually 4-6 such cycles are used. For example, if a cycle is every 3 weeks and 6 cycles are needed, then the Chemotherapy lasts for 18 weeks or 4.5 months. This is called as a course.
How long does it take for chemotherapy to be given?
The duration of Chemotherapy depends on the type of drugs used. Some drugs take less than a minute while others are given over an hour to a few hours. Some chemotherapy schedules involve continuous infusion of the drug over a number of weeks.
When is Chemotherapy used?
Chemotherapy can be used at different stages of the cancer treatment process. First, a diagnosis of cancer is confirmed with a biopsy. After that the stage of cancer is determined based on the results of all the tests including scans. Then treatment options are made based on the type of cancer, fitness of the patient and stage of the cancer. It is usually decided by then whether the cancer is potentially curable or not.
Potentially curable Cancer
Here, the treatment offered for the cancer has the chance of curing it completely. In this setting, Chemotherapy is used in the following ways.
Neo-adjuvant
This is a setting where Chemotherapy is used prior to a definitive treatment for cancer such as Surgery or Radiotherapy. The benefit of Chemotherapy here is to enhance the effect of the definitive treatment.
Adjuvant
Here the Chemotherapy is used after the definitive treatment has been done such as surgery or radiotherapy. Again, the benefit of chemotherapy here is to maximize the effect of the definitive treatment.
Concurrent
Here the chemotherapy is given at the same time as definitive treatment, usually radiotherapy. This type of treatment is called as concurrent chemo radiotherapy.
Chemotherapy alone
Some Cancers such as those arising from the blood or lymphatic system are treated with chemotherapy being the most important or the only form of treatment.
Non-Curable Cancer
In cancers that are stage 4 or non-curable, Chemotherapy forms a very important option to help control the Cancer, improve symptoms and prolong survival. This form of Chemotherapy is called as Palliative Chemotherapy, where the aim is not cure as it is not possible.
Do I need to have a central line inserted to have Chemotherapy?
Normally, Chemotherapy is given into a vein on the back of the hand or on the forearm. In situations, where the access to the veins is difficult or when the course of chemotherapy is prolonged or when continuous infusion of chemotherapy is needed, a central line is inserted to make it easy to give the treatment. There are different types of lines that can be placed as these are briefly described below. For more detail, see faq’s on chemotherapy lines.
What are the side effects of Chemotherapy?
Chemotherapy consists of a number of drugs and each drug can cause different side effects. The side effects a patient will experience will depend on the type of Chemotherapy that is given. Below are some of the general side effects that can happen with many drugs. For side effects of specific drugs, please look at the product leaflet of the drugs used.
Nausea and Vomiting- Vomiting is a side effect of Chemotherapy and therefore good medicines are given prior to chemotherapy to prevent this side effect. Tablets have to be taken for a few days after Chemotherapy also to prevent vomiting.
Hair Loss- This is a known side effect of some but not all Chemotherapy drugs. Your doctor will explain to you if it is likely to happen. If hair loss occurs, it happens in the 2nd and 3rd week after 1st chemotherapy cycle. Hair usually grows back once chemotherapy is finished.
Risk of Infection- Chemotherapy reduces the number of cells in the blood (white blood cells) that protect against infection. Therefore, there is an increased risk of infection during the period of treatment. If the patient develops a fever above 100F or feels unwell, the patient should seek medical advice urgently as infections can increase quickly.
Risk of Bleeding- Just like white blood cells, other cells in the blood called platelets can also decrease after Chemotherapy. This increases the risk of bleeding and therefore any bleeding symptoms should be reported to the doctor urgently.
Anaemia- Reduced Haemoglobin (Hb) in the blood also called anaemia can be a side effect of chemotherapy.
Loss of taste- Chemotherapy reduces the number of taste buds on the tongue and therefore food does not taste as before. This along with reduced appetite makes it difficult to eat well.
Tiredness and weakness- This is a common side effect of Chemotherapy and is variable depending on the drugs used and the fitness of the patient.
Effect on Periods- Periods can stop temporarily or permanently in women who have Chemotherapy. They tend to stop permanently in older women who are close to menopause. In younger women, there may be a temporary stoppage of periods, but these can return in a few months after completing chemotherapy.
Reduced Fertility- Chemotherapy can cause reduced fertility, that is it can reduce the chances of having a baby later if it is given. Therefore, in patients who have not completed a family but need to have chemotherapy should see a fertility specialist to discuss available options. Options of fertility preservation include sperm banking in a male where the semen is collected and stored prior to start of treatment. In women, the options include storage of oocytes (egg) or storage of embryos.
Drug dependent side effects- Some side effects that happen depend on the type of drugs that are used as Chemotherapy and the common ones are given below.
Platinum drugs- Platinum drugs such as Cisplatin and Carboplatin can affect the kidneys and close monitoring of the kidney function is needed. Cisplatin can cause reduced hearing. Oxaliplatin causes neuropathy leading to tingling in the hands and feet.
Taxanes- Common taxane drugs such as Docetaxel and Paclitaxel cause neuropathy which leads to development of tingling and numbness in the hands and feet. They can also also mucositis leading to a sore mouth, tummy pain and loose motions. Hair loss and changes in the nails also happen.
Capecitabine and Fluorouracil- These drugs are commonly used and can cause soreness in the mouth, loose motions, redness and soreness of the hands and feet, dry skin and cracking of the skin.
Anthracyclines- These drugs can affect the heart in the long term and anyone due to have these drugs has an Echocardiogram and ECG to make sure their cardiac function is adequate.
What is the cost of chemotherapy?
Chemotherapy includes a number of drugs given in various forms including tablets, injections and drips. Each of these drugs used has a price. Some of these drugs are very cheap costing less than Rs100, where as others may cost up to Rs100,000 or more. Therefore, the cost of chemotherapy treatment depends on the type of drugs used to treat the cancer. Along with the cost of the drugs, other charges such as bed charges, nursing and doctor charges are added on. It is important to ask the doctor about the approximate cost of each cycle of Chemotherapy before the treatment starts.
It is also important to consider other costs that can occur during Chemotherapy. These include costs related to hospital admissions to manage any side effects of the treatment.
How do I know if the chemotherapy is working?
A scan is typically done after two or three cycles of treatment and compared with the scan prior to the start of treatment. This will enable us to tell whether the treatment is working or not. Some cancers such as Breast, Prostate, Ovarian, Colon or Pancreatic Cancers have tumour marker blood tests which can also tell whether the Cancer is responding to treatment or not.
What is Biological therapy in Cancer?
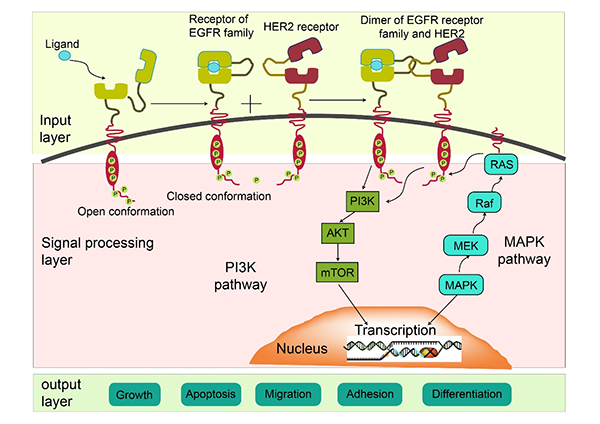
Biological therapy is the use of drugs that target specific areas of the Cancer cell and its environment. Over the last 15 years or so, there has been a significant increase in the use of biological agents in the treatment of Cancer. Biological therapy includes a vast number of treatments including angiogenesis inhibitors, monoclonal antibodies, immunotherapy, gene therapy, vaccine therapy, cytokine therapy and targeted drug therapy.
Biological therapies can be broadly divided into two groups “nibs” and “mabs”
“nibs” are agents that target specific receptors in the cancer cell pathway and stop the cancer cells from dividing and increasing. Normally the cancer grows and develops using specific pathways. These pathways are present in the growth of normal cells in the body too, but some cancers develop processes to amplify these pathways allowing them to grow faster. These drugs have names that end with “nib”. Examples include Sunitinib, Sorafenib, Erlotinib etc.
“mabs” are types of drugs which again target specific areas in the cancer cell or its pathways. Mabs are antibodies developed against specific targets in these areas. There are different types of mabs working in different areas of the Cancer pathways. Some of the common mabs used include Rituximab, Bevacizumab, Trastuzumab etc.
The below picture shows some of the pathways present in the cell that the cancer and normal cells use to grow in size and increase in number. Biological drugs act on specific areas in the pathway, blocking it.
Others
Other biological agents acting on different parts of the cancer pathways include “mibs”, for example Bortezomib and Carfilzomib used in Myeloma.
Do biological therapies produce less side effects than Chemotherapy?
By and large biological treatments have fewer side effects than Chemotherapy as they act on specific targets in the cell. However, they do have side effects and some of them can have serious side effects. So, it is not safe to assume that these drugs are not toxic. The same care and attention should be given to patients on these drugs as is given to those on Chemotherapy.
Can biological therapies be used instead of chemotherapy?
In some situations, there is a choice between Chemotherapy and a Biological agent. In others, there is benefit of using both treatments. So, which treatment to use depends on the type of Cancer, its stage, the presence of certain genetic changes in the cancer cell, the cost of treatment and the fitness of the patient.
Are biological therapies more expensive than Chemotherapy?
The cost of biological therapies varies depending on the drug used and the country in which it is used. Some biological drugs are not expensive, but others can be very expensive. By and large, on average biological therapy can be more expensive than chemotherapy.
How are Biological agents given?
Biological agents are present in tablet and injection forms. Those in injection form are given through the vein or under the skin. Tablet forms are taken by mouth.
How often are they given?
Some drugs particularly tablets are given on a daily basis. Others are given once every week to once every 3-4 weeks.
What is Immunotherapy in cancer?
Immunotherapy is the use of drugs that modify the immune system to help control and treat cancer.
What is the immune system and what is its function?
The immune system in the body consists of white blood cells in the blood, the bone marrow, lymph nodes present all over the body and organs such as the spleen. All of these help the body to fight off infections and external threat that the body receives.
Does the Immune system kill cancer?
The body’s immune system has the capacity to identify external threats such as bacteria, viruses etc and differentiate them from host cells. Therefore, when the immune system is activated in the presence of these external threats, the system kills off these threats but does not cause any damage to normal cells of the host.
When cancer develops in the body, the immune system either does not identify the cancer as foreign and therefore does not try to destroy it or identifies it but is unable to kill it. The cancer also grows and mutates in such a way that it avoids detection by the immune system.
How does Immunotherapy work?
Immunotherapy consists of a number of drugs that modify the immune system by for example-identifying the cancer cells as foreign, by enhancing the potency of the immune system by altering the mechanism.
What are the different types of Immunotherapy available?
There are many different types of Immunotherapy available and some of these are listed below.
Checkpoint Inhibitors
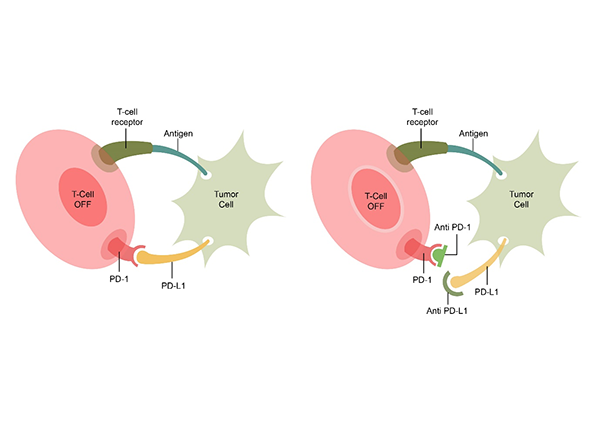
These drugs are monoclonal antibodies (mabs) that attach themselves on the surface of cancer cells making them more visible to the immune system. The system then is enabled to kill the cancer cells. A number of these checkpoint inhibitors are available for treatment in cancer. They are usually used in stage 4 cancer and help to control the cancer and prolong life. They are not able to cure cancers completely. Some of the checkpoint inhibitors used include Nivolumab, Pembrolizumab, Atezolizumab, Avelumab, Durvalumab etc. The below diagram shows how the checkpoint inhibitors work. The T Cell receptor on the body’s immune cell (T Cell) binds with the antigen of the cancer cell. Also, below, the PD-1 receptor and PD-L1 ligand combine. This combination inhibits the destruction of the cancer cell by the T Cell. In the second image, there is blockage of the PD1 and PD-L1 by checkpoint inhibitors(either anti PD-1 or anti PD-L1). This then leads to activation of the T cell and destruction of the cancer cell.
PD-L1 Status
The level of PD-L1 present in the cancer can be checked with a test. This test is done in certain cancers when a drug such as Pembrolizumab is planned to be given. The result of the PD-L1 status come as a percentage and this allows the drug to be used in certain settings. PD-L1 testing is now done routinely in lung cancer patients.
Cytokines
Cytokines are substances that are normally produced by the immune system to boost the response. These cytokines such as Interleukin and Interferon when given as an injection can enhance the effect of the immune system on cancer and help to control it. Cytokines have been used as cancer treatments for a number of years. Their benefit is mild and are used in cancers of the skin(melanoma) and kidney.
Cancer Vaccines
This type of treatment involves injecting a vaccine treatment that has been primed with the patient’s own cancer. This vaccine helps control the cancer. This is an exiting mode of treatment but only one such treatment is currently available for Prostate cancer and has not been shown to be very effective.
Adoptive Cell Therapy
Car T Cell Therapy
A new type of immunotherapy and one of the types of adoptive cell therapy where the patient’s T lymphocytes (type of white blood cells) are removed from the bloodstream and are reprogrammed to express chimeric antigen receptors (CAR). These receptors are present on the surface of these T-cells and when injected back into the patient will enable the cells to track and kill cancer cells. This therapy has been found to be very effective and is used to treat certain blood cancers in children. It is currently very expensive.
Do Immunotherapy treatments have side effects?
Yes, immunotherapy treatments have side effects, some of them could be serious and life threatening. Saying that, overall the side effects of immunotherapy drugs in general are less than those of chemotherapy. Regular tests, especially blood tests are done to look for potential side effects of these drugs. When the immune system is activated or enhanced, there is a risk of the treatment damaging normal cells also and has to be closely monitored by blood tests and how the patient is feeling.
Do Immunotherapy treatments work every time?
Like all other treatments in cancer, immunotherapy treatments do not work in every patient. The chances of response to these drugs varies from the cancer being treated to the drug being used. In those patients where there has been a good response of the cancer to these treatments, these responses tend to last for a longer period of time.
Hormonal therapy is the use of drugs or hormones that have an effect in reducing the cancer. Some cancers like breast or prostate cancers grow and increase by using the hormones that are naturally produced in the body. Hormonal therapy uses drugs that block that or increase or decrease the hormonal effect to stop the cancer from increasing. These hormonal therapies are given by tablets, injection, implants or patches. Commonly used hormonal therapies include drugs such as Tamoxifen, Letrozole, Anastrazole, Faslodex in breast cancer and Bicalutamide, Apalutamide, Enzalutamide. Goserelin, Triptorelin and Degarelix in prostate cancer. Other drugs used include Octreotide in Pituitary and Neuroendodrine tumours, Oestrogen in Ovarian and Endometrial cancers etc. Hormone therapies are effective and have less side effects than other forms of cancer treatments.
Cryotherapy in Cancer
Cryotherapy is use of very low temperatures to freeze and kill the cancer cells. This is done with the help of a cryo probe which is placed into the cancer. This type of treatment is used in cancers that have recurred and the cancer is small and limited to one part of the body. The treatment can be effective in that setting.
Radiofrequency Ablation
This is use of heat to destroy cancer cells. Like cryotherapy, there is use of a radiofrequency probe that is inserted into the cancer and heat is passed into it which kills off the cancer cells. This mode of treatment is used in cancer that has recurred in a part of the body and the recurrence is small and limited to that part of the body only. Commonly used areas in the body are when cancers have spread to the liver and the lung, for example in colon or rectal cancer.




