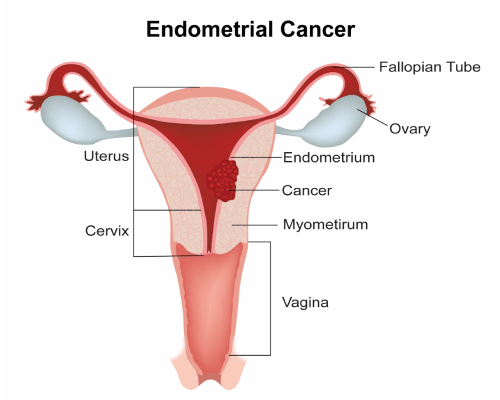
Uterus is a medical name given to the womb. Along with the cervix, vagina, ovaries and fallopian tubes, it makes up the female reproductive system.
The uterus is a muscular sac in which the baby grows. The innermost lining of the uterus is called as endometrium. The uterus has a muscular layer around the endometrium called the myometrium.
The lower part of the uterus is called the cervix which opens into the vagina. The uterus is connected to the ovaries through the fallopian tubes.
A cancer that starts in the uterus is called as uterine cancer. The cancer usually develops in the endometrium and hence uterine cancer is also called as endometrial cancer. Uterine sarcomas are different to endometrial cancers and arise from the muscle layer or other cells in the uterus. According to Globocan data 2018, there were 13,328 uterine cancers in India making up 1.2% of all cancers.
The most common type of Uterine cancer is an endometrial carcinoma which account for about 90% of all uterine cancers. Adenocarcinomas are by far the most common endometrial carcinomas.
Less common tumours or cancers of the uterus include uterine sarcomas. Uterine sarcomas can be mixed mullerian tumours (carcinosarcoma), endometrial stromal sarcoma and leiomyosarcomas.
There are various risk factors associated with cancer of the Uterus and are listed below. A risk factor is one that increases the risk of getting cancer.
Age
Uterine cancer is more common in women of older age. Less than 1% of uterine cancer occurs in women under the age of 40. It is most common in women after the menopause.
Obesity and overweight
Being obese is a significant risk factor for development of endometrial cancer. This amount of risk increases with increasing amount of obesity. This is mainly due to increased amount of the hormone oestrogen present in the body of obese women.
Diabetes
The risk of endometrial cancer increases in people with diabetes.
Drugs
Use of oestrogen only hormone replacement therapy in menopausal women can increase the risk of endometrial cancer. Also use of drug called Tamoxifen increases the risk.
Polycystic Ovary Disease
Women with a condition called polycystic ovary disease have an increased risk of developing uterine cancer mainly due to hormonal imbalances present in this condition.
Family History
Women with a mother who had endometrial cancer have a slightly increased risk. Also, families with a history of a genetic condition called HNPCC are at risk of developing endometrial cancer.
Early Menarche and Late Menopause
Women in whom periods start early in life and those in whom menopause is late have an increased risk of uterine cancer, again mainly due to increased amount of Oestrogen produced by the ovaries during this period.
Factors that reduce the risk of getting uterine cancer include physical activity and using the oral contraceptive pill.
Endometrial cancers generally present early and are usually diagnosed in early stages due to the nature of symptoms they produce. By far the most common symptom of presentation is vaginal bleeding.
Post Menopausal bleeding
The commonest presenting symptom of endometrial cancer is bleeding from the vagina in women after the menopause. This can be any bleeding including slight spotting or staining.
Other Vaginal Bleeding
Bleeding in between periods or prolonged and heavy bleeding may also be a sign of endometrial cancer and should be investigated.
It is important to note that most often above symptoms are not related to endometrial cancer, but it is important to have the symptoms evaluated.
Other Symptoms
Symptoms such as feeling a lump or mass in the abdomen, passing of blood in the urine, constipation, bleeding from the anus, back pain, weight loss, reduced appetite pain etc are present in patients with advanced disease but are uncommon in this type of cancer.
The following investigations are done to confirm and stage Uterine or endometrial cancer after a thorough physical examination by a Gynaecologist.
Pelvic Ultrasound
An ultrasound scan of the pelvis is done to look for thickening in the endometrium. As explained in the other section, the endometrium is the lining of the uterine cavity and a thickening of this lining can be seen on the ultrasound scan particularly in a transvaginal ultrasound scan. Here the scan probe is inserted in the vagina to get clear images of the endometrial cavity. A thickening of the endometrium can be due to endometrial cancer but most of times it isn’t. If a thickening is seen, more tests are needed to determine the cause.
Endometrial Pipelle Biopsy
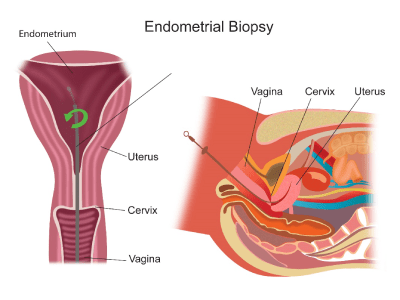
Hysteroscopy and Biopsy
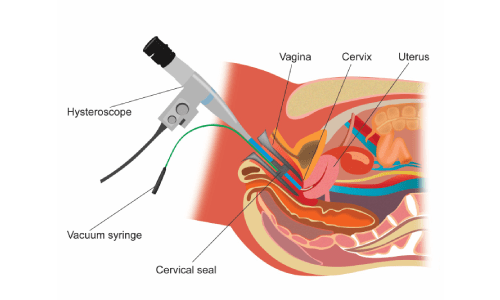
D and C (Dilatation and Curettage)
Here the doctor dilates(expands) the endometrial cavity and does a curettage (complete removal) of the endometrial lining and this is sent off for a biopsy. This is done in some situations instead of sampling of a small amount of the lining. This procedure can be done with the use of a hysteroscope.
Other Investigations
Once an endometrial cancer is diagnosed on biopsy, other tests are done to stage the cancer.
Staging tests help identify the presence or absence of spread of endometrial cancer from its place of origin to other areas either locally or to other parts of the body. Accurate staging helps define the most appropriate treatment strategy.
Endometrial cancer is usually diagnosed in an early stage. Therefore, any staging investigations done are mainly to assess the local spread of disease in the pelvis.
MRI Scan Pelvis
An MRI scan of the pelvis helps in assessing the spread of endometrial cancer in the uterus, cervix and beyond. It also gives information about spread of the cancer into the lymph nodes of the pelvis.
MRI scan is said to be better than CT and PET-CT scans in this setting to stage this cancer.
CT Scan chest Abdomen
A CT scan of the chest and abdomen looks for spread of the cancer into the chest and abdomen areas. This scan is not routinely needed but done when there is high suspicion of spread.
Blood Tests
Routine blood tests are done prior to treatment of this condition. Special tests such as CA125 are sometimes done for this cancer.
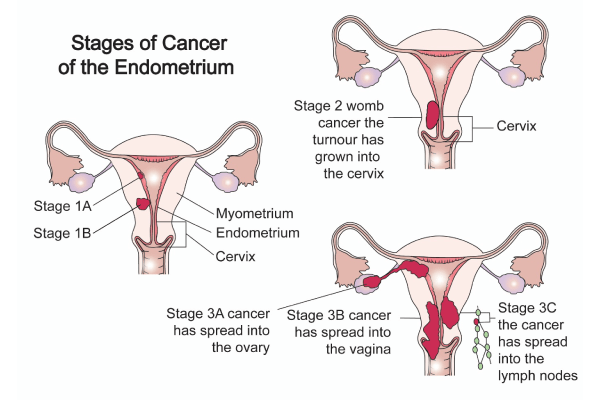
Endometrial Cancer is staged based on the TNM staging system and FIGO staging system.
These stages are listed below.
T stage and FIGO stage
| TNM Stage | FIGO Stage | |
|---|---|---|
| T1 | 1 | Tumour present in Uterus only |
| T1a | 1a | Tumour present in endometrium only or extends to inner half of muscle layer |
| T1b | 1b | Tumour extends to outer half of muscle layer |
| T2 | 2 | Tumour extends into the cervix |
| T3a | 3a | Tumour involves outer layer of uterus or fallopian tubes or ovaries |
| T3b | 3b | Tumour involves vagina or area surrounding the uterus (parametria) |
| T4 | 4a | Tumour involves urinary bladder or bowel |
N Stage and FIGO stage
| N0 | Lymph nodes not involved by tumour | |
| N1 | 3C1 | Tumour spread to pelvic lymph nodes |
| N2 | 3C2 | Tumour spread to para-aortic node |
M Stage and FIGO Stage
| M0 | No distant spread | |
| M1 | 4b | Distant spread of cancer present |
Risk stratification
Endometrial cancer is also classified into low risk, intermediate risk and high risk, based on its grade at diagnosis, type of cancer and stage of cancer. This helps the doctor and patient to understand the risk of recurrence of cancer after surgery and will help the doctor to devise the most appropriate treatment.
Low risk cancer is when the cancer is grade 1, is confined to the endometrium and does not have a cell type that is high risk.
Intermediate risk cancer is one where the cancer has spread into the muscle layer or cervix (stage 2) and does not have a cancer type that is classified as high risk. Intermediate risk cancer is again subdivided into low-intermediate risk and high-intermediate risk. Those that are high-intermediate risk include those that are grade 2 and 3, involve the outer one third of the uterine muscle or have lymphatic or vascular invasion seen on biopsy or operation specimen.
High risk cancer is one where the cancer is staged as stage 3 or 4 or are found to be serous adenocarcinoma or clear cell adenocarcinoma.
Grading of Cancer
Endometrial cancer is divided into three grades based on the aggressiveness of the cancer seen under the microscope after biopsy. These grades are named as 1, 2 and 3 with 1 being least aggressive, 3 being most aggressive and 2 in between. The grading plays a part in determining the choice of treatment.
Treatment of Uterine or Endometrial cancer is mainly determined by the stage of cancer at diagnosis. The treatment options include surgery, chemotherapy and radiotherapy and are explained below.
Surgery
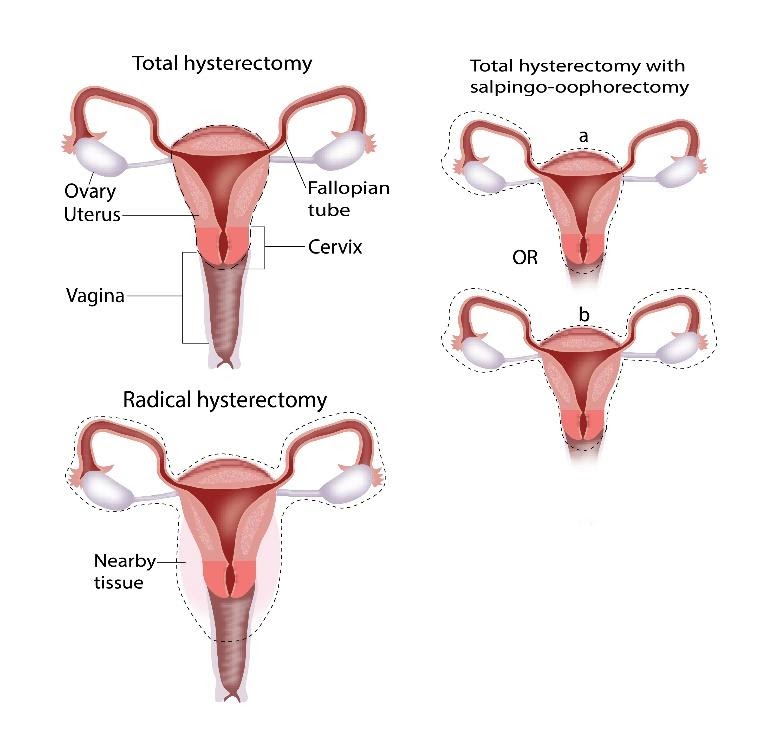
In certain types of endometrial cancer, a part of the abdomen called radical hysterectomy
Radiotherapy
Radiotherapy is an important component of treatment of endometrial cancer. Here, radiotherapy is mainly used after surgery and is called as adjuvant radiotherapy. The idea of adjuvant radiotherapy is to maximise the chances of cure that have been achieved by surgery.
Radiotherapy is given in two ways. One is external beam radiotherapy, where the treatment is given with a machine present in the room which delivers the treatment from outside the body. It is similar to having an x-ray, except that the rays are stronger than standard x-rays.
The other way to give radiotherapy is called brachytherapy, where a radioactive source is inserted into a part of the body where treatment is intended.
In endometrial cancer, the treatment may involve brachytherapy alone or a combination of external beam radiotherapy and brachytherapy. Which treatment to give is based upon the stage of cancer that is found after completion of surgery.
Following surgery, women are classified into having low risk, intermediate risk and high-risk endometrial cancer based on the stage of cancer that is found and other features seen on examination of the operated cancer. Patients with very low risk cancer do not need any adjuvant radiotherapy at all. Other patients may need brachytherapy alone or a combination of external beam and brachytherapy treatments.
External Beam Radiotherapy
When this treatment is given in endometrial cancer, it is done over a period of 5-6 weeks, once each day for 5 days a week. The treatment area will be the pelvis (lower part of abdomen). This treatment can be delivered with techniques like 3D conformal or IMRT.
Potential side effects of radiotherapy include symptoms such as tiredness, redness of skin, loss of hair in the treated area, loose motions, passing urine more frequently, burning sensation when passing urine. Most of these side effects peak towards the end of treatment and for a week after and settle down a few weeks after treatment is finished.
Brachytherapy
The aim of brachytherapy treatment in uterine cancer is to give a high dose of radiotherapy to an area at the top of the vagina to reduce the risk of recurrence of cancer in that area. In this treatment, a vaginal cylinder is inserted into the vagina. This cylinder is attached to the brachytherapy machine and a radioactive source is passed into the cylinder to deliver the radiotherapy to the intended area. The cylinder is kept in place for a few minutes for each treatment. Anaesthetic is not needed for the procedure and a total of 3-5 treatments are given either once or twice a week. Potential side effects of this treatment include small risk of loose motions, long term narrowing of vagina. This can be reduced by using vaginal dilators on a regular basis for some time after completion of treatment.
Chemotherapy
Chemotherapy in uterine cancer is used in two settings. One is called as adjuvant chemotherapy, where this treatment is given after surgery to maximise the chances of a cure. The other setting is in advanced or metastatic disease where chemotherapy is used to control the cancer.
Adjuvant chemotherapy is given after surgery in some intermediate risk uterine cancer and most high-risk uterine cancers. Usually a combination of two drugs are used. They are given once every three weeks(cycle) for up to 6 cycles. Common drugs used for adjuvant chemotherapy include Carboplatin and Paclitaxel.
Treatment of Isolated recurrences
Some patients can have recurrence of cancers in only one area of the body after they complete initial treatments. These recurrences can be in the uppermost part of the vagina called the vaginal vault or in the area called the pelvis. These recurrences can be treated with radiotherapy or surgery depending on whether radiotherapy was used earlier or not. If radiotherapy was used before, it cannot be used again, and surgery will be the only option in that setting. When isolated recurrences are treated there is a reasonable chance of long term control of the disease.
Treatment of Metastatic Disease
Metastatic disease or disease which is stage 4 is treated differently to other stages of cancer. Once metastatic disease is diagnosed, treatment options are mainly to control the disease rather than to cure it.
In metastatic endometrial cancer, chemotherapy is commonly used to control the cancer and the symptoms that it produces. The aim of chemotherapy here is to control the cancer and prolong life.
Common chemotherapy drugs used in this setting include Carboplatin, Paclitaxel, Bevacizumab among others.
Radiotherapy is also an option in some settings where it is used to control symptoms produced by the cancer. In this instance, treatment duration is usually shorter. Radiotherapy is also used when there is a recurrence of cancer in one area only after previous treatment.
Hormonal therapy is used in metastatic endometrial cancer when chemotherapy options have been exhausted or the patient is not physically well enough to receive chemotherapy. In hormonal therapy, drugs such as progesterone and Tamoxifen are used.
Surgery can sometimes be an option of treatment in metastatic endometrial cancer when the bulk of disease is in the uterus. Surgery can be used to remove the uterus with the disease if it is felt to be operable.




